Abstract
One of the most important complications during thyroid surgery is injury to the recurrent laryngeal nerve (RLN) which leads to dysfunction and palsy of the vocal folds. Adequate knowledge about the location of the RLN supported by neuromonitoring can help the operating surgeon to prevent this complication. Visualization of the nerve alone seems not enough. An estimation of the function of the RLN is very important. Recently, the use of neuromonitoring has been increasingly employed to predict and document nerve function at the end of thyroidectomy. The aim of the study was to verify the usefulness of neuromonitoring in identifying the recurrent laryngeal nerve and to predict postoperative outcome in patients undergoing thyroid surgery for different indications. Between March 2009 and October 2010, 91 patients (26 men, 65 women; mean age 53 (range 26–83) underwent thyroidectomy. Intraoperative neuromonitoring (IONM) was registered for 91 patients. Eighty-four total thyroidectomies and seven lobectomies were performed with IONM. Eight unilateral postoperative transient paresis were identified without any permanent paralysis. Intraoperative neuromonitoring has an excellent specificity and negative predictive value in which an unchanged positive signal is highly predictive of intact nerve function. Intraoperative neuromonitoring during thyroid surgery is a reliable tool for early recurrent laryngeal nerve localization and identification, certainly in complicated thyroid operations. The probability is high for correctly predicting an intact postoperative nerve function by neuromonitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most important complications during thyroid surgery is injury to the recurrent laryngeal nerve (RLN), which leads to dysfunction and palsy of the vocal cords. Recurrent laryngeal nerve palsy is an important and potentially catastrophic complication of thyroid surgery. Permanent RLNP occurs in 0.3–3 % of the cases, with transient palsies in 5–8 %. Adequate knowledge about the location of the RLN supported by neuromonitoring can help the operating surgeon to prevent this complication. Visualization of the nerve alone is the gold standard but seems not to be enough. Much more important is an estimation of the function of the RLN. One can say that nowadays we are in the passing era (transition period) of only visualization of the recurrent laryngeal nerve during operation and entering the era of its neuromonitoring. Neuromonitoring gives us the information about the location and function of the RLN. Neuromonitoring gives us information about the location and function of the RLN. Using this equipment, thyroid surgery becomes safer not only for the patients but also for the operating surgeon especially for surgical complications (malpractice, law suits, etc,). In thyroid surgery, intraoperative neuromonitoring of the recurrent laryngeal nerve (RLN) and vagal nerve (VN) is performed as an adjunct to the gold standard of optical visualization of the RLN, and subsequently paralysis of the vocal cords. Intermittent intraoperative neuromonitoring (phrase incomplete).
Material and methods
Between March 2009 and October 2010, 91 patients [65 females and 26 males, with a mean age of 53 years (range 26–83 years)] with 175 nerves at risk (NAR) were enrolled in this study. Operations for benign multinodular goiter in 66 % of the cases, for toxic goiter in 13 % of the cases and for thyroid cancer in 2 % of the cases.
The used device (Neurosign 100) consisted of an endotracheal-based surface electrode and a bipolar stimulator. Tube was carefully placed at the glottis level, placing the electrodes between the vocal cords. No neuromuscular blocking agent was used during the procedure.
Laryngeal neuromonitoring was outlined according to the following scheme: (a) Preparation of the operative space. Before any manipulation of the thyroid gland, the vagus nerve was dissected over a short (2 cm) stretch to allow for the atraumatic placement of a vessel loop, a procedure that took about 1–5 min and that did not result in any complication. (b) Vagal nerve stimulation (V1) was performed by placing the bipolar concentric stimulating probe onto the vagus nerve; the current amplitude was 1 mA (rectangular 3 Hz pulse for 1–2 s). The electrical field response can be documented by recording the potentials or by converting the electric field response of the muscle to an acoustic signal. (c) The thyroid lobe was mobilized, and the branches of the upper thyroid pole were ligated and severed. (d) Visualization, stimulation (R1), and dissection of the RLN. An attempt was made to identify the recurrent nerve using the electrode rather than by palpation and surgical dissection. Neuromonitoring is being advocated for the rapid and reliable identification of the recurrent laryngeal nerve and for predicting the postoperative vocal cord mobility. This obviously required electrical stimulation of structures that looked like a nerve. It is also worth pointing out that the recurrent laryngeal nerve was successfully identified by this approach by moving the electrode through the retrothyroidal space. (e) The resection of the thyroid lobe was conducted under visual control of the nerve and under neuromonitoring. (f) Final hemostasis. (g) After the removal of the thyroid and prior to wound closure, the stimulating electrode was placed onto the recurrent laryngeal nerve and the vagus nerve (V2, R2).
Neuromonitoring was performed with the Neurosign 100 device. The signal parameters amplitude, latency and thresholds of nerve conductance were compared starting thyroid resection and after finishing thyroid preparation. The diagnosis was performed by standard procedures. Vocal cord function was determined in all patients before surgery and on day six or seven after surgery by laryngoscopy.
Postoperative nerve injuries were followed-up at regular intervals (on day 15, after 1, 3, 6 and 9 months).
To account for the different types of operation (i.e., unilateral and bilateral procedures). We present the data based on the number of nerves at risk.
Sensitivity, specificity, positive, and negative predictive value for individual patient group were calculated from the MedCalc® software. Wilcoxon test was used for median comparison after normality rejection by the D’Agostino-Pearson test for Normal distribution.
Loss of signal was defined by an EMG change from initial satisfactory waveform and/or the absence or low response (100 μV) with stimulation at 0.5 mA in a dry field.
Results
Intraoperative neuromonitoring was registered for 91 patients. Vagal nerve stimulation was feasible in all cases and did not result in any morbidity. All the vagal nerve stimulation signals were successfully obtained within 30 min of the start of the operation and all showed a clear and reliable laryngeal electromyography (EMG) response.
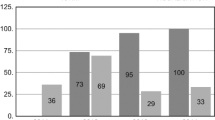
The intraoperative electromyography (EMG) (amplitude and latency, respectively) of 167/175 RLN showed no difference of the RLN registered before (R1) and after the dissection (R2) (p = 0.64 and p = 0.70 respectively) (Tables 1, 2).
Eight nerves (4.5 %) experienced loss of R2 (recurrent laryngeal nerve after dissection) and V2 (vagus nerve after dissection) signals. 80 % of lesions occurred in the distal 1 cm of the course of the RLN near the ligament of Berry. The electrical field response was normal over the entire cervical course of the nerves. The mechanism of injury was most probably traction (80 %). In all instances, the nerves were anatomically intact.
In one case, a drastic diminution of the amplitude (0.59–0.048 mV) was noted. In three cases, no difference was observed concerning the registration of the amplitude after the RLN stimulation only (Table 3) but well after the vagus nerve stimulation.
Concerning these three cases, a total absence of response after vagus nerve stimulation was noted in two cases and a 36 % decrease of amplitude was registered in the last case (1.515–1.003 mV), raising the negative predictive value (VPN) to 100 % (Table 4).
Discussion
There is continued debate over the value of laryngeal nerve monitoring (LNM) during thyroidectomy [1]. Currently, no consensus exists regarding the use of LNM during thyroid surgery. However, results of an anonymous survey of the members of the American Head and Neck Society suggest that LNM use has become more widespread.
Therefore, there are three arguments in favor of neuromonitoring during thyroid surgery. First, neuromonitoring increases the ability of the surgeon to reliably identify the recurrent laryngeal nerve, and this is presumably one of the reasons for its increasing popularity. The second reason is to verify the functional integrity of the recurrent laryngeal nerve prior to ending the surgical procedure. Thirdly, neuromonitoring may provide guidance for the surgeon in difficult situations such as anatomic variants, reoperations and surgery for malignant disease [2].
A literature review thought us that recurrent laryngeal nerve damage is an important catastrophic complication of thyroid surgery. Permanent recurrent laryngeal nerve palsy occurs in 0.3–3 % of cases, and transient palsies in 5–8 % [3].
However, some authors believe that intraoperative neuromonitoring (IONM) during thyroid surgery does not bring any additional reduction in the paralysis rate of the recurrent laryngeal nerves [4, 5].
In their retrospective study [5], Alesina et al. reviewed their patients treated by total thyroidectomy with or without intraoperative neuromonitoring. 250 patients underwent 250 operations for goiter, hyperthyroidism or thyroid cancer. In the neuromonitoring group, the number of nerves at risk was 128 and, in the direct visualization group, the number of nerves at risk was 161. They registered eight recurrent laryngeal nerve palsies in the neuromonitoring group (6.2 %) and four in the group of patients with direct nerve visualization (2.5 %) (p = 0.1).
However, other researchers defend its use but only in selected cases and in very specific situations [2, 7].
In their study [7], Barczynski et al. [6] compared the outcomes of 151 patients treated by total thyroidectomy with IONM with level IV lymph node clearance for well-differentiated thyroid cancer and 151 patients undergoing surgery without IONM. Among the patient operated with vs. without IONM, the early RLN injury rate was 3 vs. 6.7 % (p = 0.02), including 2 vs. 5 % (p = 0.04) of temporary nerve lesions, and 1 vs. 1.7 % of permanent nerve events (p = 0.31), respectively. They concluded, based on their results, that the use of IONM may improve the outcomes of surgery among these patients by both increasing the completeness of total thyroidectomy and significantly reducing the prevalence of temporary RLN injury.
Frattini et al. [8] concluded the same in their retrospective series study. Intraoperative neuromonitoring during thyroidectomy is an effective procedure in thyroid cancer patients. In their retrospective series, the overall RLN morbidity was 3.9 % in the IONM group and 9.2 % in the control group (p < 0.05).There have been two cases of permanent RLNP (2.6 %) in the control group and one in the IONM group (1.3 %), one case of bilateral RLN injury in the control group. The incidences of temporary RLNP in the IONM group have been 2.6 vs. 6.5 % in the control group.
Finally, some surgeons advocate the routine use of intraoperative neuromonitoring in all thyroidectomies.
In their study, Chiang et al. [9] evaluated the routine use of IONM in thyroid operations. Their prospective study enrolled 220 consecutive patients (333 RLNs at risk) who underwent thyroid operations with application of IONM. All the RLNs, including 87 (26 %) nerves that were regarded as difficult to identify, were successfully localized and identified. The stimulation level for RLN localization was 2 mA in 315 nerves (95 %) and 3 mA in the other 18 nerves (5 %). The palsy rate was 0.6 % and no permanent palsy occurred.
In our series, all the recurrent laryngeal nerves, including nerves that were regarded as difficult to identify, were successfully localized and identified. The palsy rate was higher (4.5 %) but comparable with the rate described in the literature (5–8 %) and no permanent palsy occurred. RLN injury was rare if the nerve was definitely identified early in the thyroid operation.
Our data, compared to the results reported in the literature [10–13], confirmed that intraoperative neuromonitoring during thyroid surgery has an excellent specificity and negative predictive value in which an unchanged positive signal is highly predictive of intact nerve function.
Based on these data, some authors [14, 15] advocated changing the operative strategy during bilateral thyroid procedures to avoid bilateral recurrent laryngeal nerve palsy (RLNP). They recommend a two-stage thyroidectomy after signal loss on the primary side of resection. In their opinion, the change in operative strategy will lead to an almost 0 % rate of bilateral laryngeal nerve palsy. While this strategy is comprehensible for the surgeon, the question remains, whether it is always necessary.
Clearly, the staged thyroidectomy is not supported by Sitges-Serra et al. [16]. In their study, two-hundred and ninety patients were included. Loss of signal on the first side was noted in 16 procedures (5.5 %). Thyroidectomy was completed and, at retesting, 15 of 16 initially silent nerves recovered an electromyographic signal with a mean amplitude of 132 mcV. Mean time of recovery was 20.2 min (range 10–35). No patient had a bilateral loss of signal (no reason for staged thyroidectomy). Only three of 15 nerves with a recovered signal were associated with transient vocal cord dysfunction.
After loss of signal of the recurrent laryngeal nerve dissected initially, there was a 90 % chance of intraoperative signal recovery. In this setting, bilateral thyroidectomy can be performed without risk of bilateral recurrent nerve paresis.
In conclusion, intraoperative neuromonitoring during thyroid surgery has an excellent specificity and negative predictive value (100 % in our series) in which an unchanged positive signal is highly predictive of intact nerve function. This technique facilitates recurrent laryngeal nerve identification in altered anatomy and increases the security of the surgeon in this technique. However, IONM failed to reduce the rates on nerve injury.
References
Singer MC, Rosenfeld RM, Sundaram K (2012) Laryngeal nerve monitoring: current utilization among head and neck surgeons. Otolaryngol Head Neck Surg 146:895–899
Chiang FY, Lu IC, Tsai CJ, Hsiao PJ, Hsu CC, Wu CW (2011) Does extensive dissection of recurrent laryngeal nerve during thyroid operation increase the risk of nerve injury? Evidence from the application of intraoperative neuromonitoring. Am J Otolaryngol 32:499–503
Hayward NJ, Grodski S, Yeung M, Johnson WR, Serpell J (2013) Recurrent laryngeal nerve injury in thyroid surgery: a review. ANZ J Surg 83:15–21
Cernea CR, Brandao LG, Brandao J (2012) Neuromonitoring in thyroid surgery. Curr Opin Otolaryngol Head Neck Surg 20:125–129
Alesina PF, Rolfs T, Hommeltenberg S, Hinrichs J, Meier B, Mohmand W, Hofmeister S, Walz MK (2012) Introperativeneuromonitoring does not reduce the incidence of recurrent laryngeal nerve palsy in thyroid reoperations : results of a retrospective comparative analysis. World J Surg 36:1348–1353
Barczynski M, Konturek A, Stopa M, Hubalewska-Dydejczyk A, Richter P, Nowak W (2011) Clinical value of intraoperative neuromonitroing of the recurrent laryngeal nerves in improving outcomes of surgery for well-differentiated thyroid cancer. Pol Przeglchir 83:196–203
Lang BH, Lo CY (2010) Technological innovations in surgical approach for thyroid cancer. J Oncol 2010. doi:10.1155/2010/490719
Frattini F, Mangano A, Boni L, Rausei S, Biondi A, Dionigi G (2010) Intraoperative neuromonitoring for thyroid malignancy surgery : technical notes and results from a retrospective series. Updates Surg 62:183–187
Chiang FY, Lu IC, Chen HC, Chen HY, Tsai CJ, Lee KW, Hsiao PJ, Wu CW (2010) Intraoperative neuromonitoring for early localization and identification of recurrent laryngeal nerve during thyroid surgery. Kaohsiung J Med Sci 26:633–639
Hemmerling TM, Schmidt J, Bosert C (2001) Intraoperative monitoring of the recurrent laryngeal nerve in 151 consecutive patients undergoing thyroid surgery. Anesth Analg 93:396–399
Timmerman W, Dralle H, Hamelmann W (2002) Does intraoperative nerve monitoring reduce the rate of recurrent nerve palsies during thyroid surgery? Zentrabl Chir 127:395–399
Ram K, Dam L, in’t Hof KH, Nieveen van Dijkum EJ (2012) Introperative neuromonitoring during endocrine surgery. Ned TijdschrGeneeskd 156: 4483
Pardal- Refoyo JL (2012) Usefulness of neuromonitoring in thyroid surgery. Acta Otorinolaringol Esp 63:355–363
Melin M, Schwarz K, Lammers BJ, Goretzki PE (2013) IONM-guided goiter surgery leading to two stage thyroidectomy: indication and results. Langenbecks Arch Surg 398:411–418
Sadowski SM, Soardo P, Leuchter I, Robert JH, Triponez F (2013) Systematic use of recurrent laryngeal nerve neuromonitoring changes the operative strategy in planned bilateral thyroidectomy. Thyroid 23:329–333
Sitges-Serra A, Fontané J, Duenas JP, Duque CS, Lorente L, Trillo L, Sancho JJ (2013) Prospective study on loss of signal on the first side during neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy. Br J Surg 100:662–666
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dequanter, D., Charara, F., Shahla, M. et al. Usefulness of neuromonitoring in thyroid surgery. Eur Arch Otorhinolaryngol 272, 3039–3043 (2015). https://doi.org/10.1007/s00405-014-3293-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3293-y