Abstract
The most commonly used treatment for sensorineural sudden hearing loss (SSHL) in clinical practice is the administration of steroids; however, a favorable result is not always obtained. We studied 58 patients who failed to recover after primary treatment with IV steroids, 44 of these met our inclusion criteria (mean age 50.7, 27 males, range 30–74). We treated 23 patients (mean age 47.3, 16 males, age range 22–74) with hyperbaric oxygen therapy (HBO) (2.5 ATA for 60 min for 15 treatments), while 21 (mean age 54.5, 11 males, age range 22–71) patients refused to be treated and served as a non-randomized control group. Patients treated with HBO had a mean improvement of 15.6 dB (SD ± 15.3), with 1 of them completely healed, 5 with a good recovery, 10 with a fair recovery and 7 unchanged. Patients who were not treated had a spontaneous mean improvement of 5.0 dB (SD ± 11.4) with 3 patients with a good recovery, 1 patient with a fair recovery and 17 patients unchanged. Mean improvement was significantly better in patients treated with HBO compared to controls (p = 0.0133). Patients with worst hearing had the greater degree of improvement whether or not they were treated in the first 10 days after the onset of the hearing loss or between 11 and 30 days. In conclusion, hyperbaric oxygen therapy can lead to significant improvement of pure tone hearing thresholds in patients with SSHL who failed primary corticosteroid treatment and are within 4 weeks of the onset of deafness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden sensorineural hearing loss (SSHL), defined as hearing loss of at least 30 dB in three sequential frequencies in the standard pure tone audiogram occurring over 3 days or less, has an estimated incidence of 5–20 per 100,000 persons per year [1]. This number seems to be increasing, especially in the elderly, as shown in recent studies [2]. Some authors have reported an incidence of 160 cases per 100,000 per year and conclude that this condition should no longer be considered rare [3]. Moreover, the incidence is likely to be underestimated because many patients recover spontaneously and do not seek medical help.
In fact, the spontaneous remission rate has been reported as 45–65 % [4]. The natural history of SSHL is highly variable, suggesting that multifactorial pathogenesis is involved, including viral infection, vascular occlusion, breaks of the labyrinthine membranes, immune-mediated mechanisms and abnormal cellular stress responses [5, 6]. A variety of medical therapies have been proposed with varying results. The most commonly used treatment in clinical practice is the administration of steroids [7], which can be administered orally, intravenously or by intratympanic (IT) injections. Evidence of the usefulness of steroids is not strong and is mostly based on retrospective series [8] and few placebo controlled trials [7, 9]. The dosage and the route of administration of steroids influence the concentration of the drug in the inner ear and for this reason IT steroids, which offer the higher concentration with less systemic effects, have gained popularity [10]. Even when patients are treated in the early phases after onset, a favorable result is not always obtained and approximately 40 % do not respond fully to systemic treatment [9]. Permanent hearing loss is a dramatic consequence, so the use of secondary treatment modalities, which include intratympanic steroids [11], hyperbaric oxygen therapy (HBO) [12] and plasmapheresis [13], has been advocated. Hyperbaric oxygen therapy (HBO) has been proposed because whether or not hypoxia is the initial cause or a consequence of other inflammatory processes, the ischemia which results is known to greatly affect the functioning of the cochlea. In particular, ischemia induces transcription of hypoxia inducible genes, which are involved in acute as well as chronic damage to microcirculation [14].
Despite many studies on HBO as a primary treatment [15–17], there are few prospective studies about HBO as a salvage treatment and no studies with a control group in the acute phases of SSHL have been carried out, to the best of our knowledge. The aim of the present study was to evaluate the hearing improvement in patients with SSHL refractory to steroid treatment treated with HBO in comparison with patients who received no further treatment.
Materials and methods
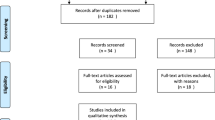
From March 2011 to February 2013, 168 patients with SSHL presented to our department. Patients underwent clinical history taking, complete ENT examination, audiological testing and brain MRI. Thirty-three patients, who presented more than 30 days after disease onset, who had hearing loss lesser than 30 dB in three contiguous frequencies, who had a history of fluctuant hearing loss or evidence of acoustic neuroma, were excluded.
The remaining 135 patients were all treated with corticosteroids (intravenous betamethasone at doses of 4 mg) and osmotic diuretics (intravenous administration of 250 cc of mannitol 18 %) for 6 days consecutively (Fig. 1). Patients were assessed with audiometry after the primary treatment with IV steroids to assess if the response was adequate. Mean hearing thresholds were expressed as the pure tone average (PTA) of the 0.25-, 0.5-, 1.0-, 2.0-, 3.0-, 4.0-, 6.0-, and 8.0-kHz hearing thresholds. Mean hearing gain was calculated as the difference between PTA prior and post the treatment. If hearing had worsened, was unchanged or if mean hearing gain was ≤10 dB patients were considered to have failed to recover and were further treated with a course of oral steroids (dexamethasone 25 mg once a day) for 7 days. Moreover, a cycle of hyperbaric oxygen therapy was offered to all patients, except to those having medical comorbidities contraindicated in HBO, such as untreated pneumothorax, uncontrolled seizure disorders, severe chronic obstructive pulmonary disease (COPD) [18]. The patients able to undergo HBO, but who refused it were not treated anymore, were considered as control group. HBO sessions were performed once a day for 15 consecutive days in a 12 place chamber (Model type Zyron-12. Hipertech®, Istanbul, Turkey) using the following protocol: 12 min for compression time, 30 min for breathing O2 at 2.5 ATA, 3 min for breathing environmental air, 30 min for breathing O2 at 2.5 ATA and 15 min of decompression time. Our treatment protocol is reported in Fig. 1.
The degree of the residual hearing loss after primary therapy was classified as mild (≤40 dB), moderate (41–70 dB), severe (71–90) or profound (≥91). We classified the degree of recovery into four categories: complete (hearing return to the same level of the unaffected ear), good (hearing return to within 15 dB of the unaffected ear), fair (hearing level improved by more than 10 dB but not returned to within 15 dB of the unaffected ear) and poor (hearing level worsened, unchanged or improved by less than 10 dB). Baseline patients’ characteristics are shown in Table 1. The study was approved by the Ethics Committee of our institution. All patients gave a signed inform consent describing the interventional procedure.
Statistical analysis
Comparisons between the intervention group (HBO) and the control group (no HBO) were analyzed using Pearson Chi squared tests for categorical data and unpaired t test for continuous data (e.g., means). Odds ratios (OR) with 95 % confidence intervals (CI) were calculated to measure possible univariate associations between HBO and different outcomes, such as recovery, degree of recovery (complete, good, fair), PTA gain, days after onset, age, also stratified by categories of hearing loss (profound/severe vs. moderate/mild) to assess for possible effect modification. To assess for possible confounding, OR for recovery were also calculated between different categories of hearing loss (mild, moderate, profound, and severe), age, sex, and days after onset and recovery. OR for continuous variables (e.g. age) were calculated using a univariable logistic regression model. Outcomes and possible confounding factors were also introduced in a final multivariable logistic regression model. All analyses were carried out using Stata® 10 (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP).
Results
Fifty-eight patients failed to recover from primary therapy among whom eight patients had medical contraindication to HBO and six patients were treated with HBO but did not come for the audiometry scheduled after 3 months and were, therefore, excluded from the study group. Therefore, only 44 patients (mean age 50.7, range 30–74, 27 males) were allocated to the study group. Among these, 23 patients (mean age 47.3, 16 males, age range 22–74) were treated with HBO while the remaining 21 (mean age 54.5, 11 males, age range 22–71) patients refused to be treated and served as a control group. Table 1 presents characteristics of case and control groups. There were no significant differences in baseline characteristics between cases and controls. Table 2 shows comparison of outcomes in the control and study group. Mean PTA gain was significantly better in patients treated with HBO compared to controls (p = 0.01). There was a significant difference in patients experiencing recovery (complete, good, fair, or unchanged) between the two groups (Table 2). There was a significant positive association between recovery and the degree of PTA gain, having received HBO. When recovery was broken down into three categories, experiencing a fair recovery was the only one significantly associated with HBO, while complete and good recoveries were not. The OR for recovery in the profound and severe hearing loss stratum were similar to the moderate and mild ones, whereas PTA gain was only significantly associated with HBO in the latter stratum and being male in the former (Table 3). Having experienced a mild hearing loss and increasing days after onset were negatively associated with recovery (Table 4). In the first multivariable model, recovery was the only variable positively associated with HBO (Table 5); while in the second only experiencing a fair recovery and being male were positively associated with HBO (Table 6). When stratified by gender, the OR between HBO and recovery were 7.5 (95 % CI 0.96–87.24; p = 0.023) in the male group and 24.00 (95 % CI 1.27–1,236.47) in the female group.
HBO did not cause clinical side effects other than mild middle ear barotrauma in four patients and one episode of confinement anxiety. Barotrauma, due to wrong equalization maneuvers, was characterized by pain and discomfort during the descent phase but did not lead to middle ear effusion and was managed with a topical decongestant and the use of slower compression speed. Confinement anxiety was managed with the administration of low doses of benzodiazepine during treatment (oral diazepam 2 mg).
Discussion
We found that in patients with SSHL, refractory to a first-line treatment based on intravenous steroids, the administration of HBO + oral steroids led to better hearing gain compared to a control group that received only oral steroids. Our protocol included the administration of oral steroids to all patients (control and study groups) who failed to recover after intravenous steroids, so we considered the positive results obtained in the study group due to HBO. Patients with worse hearing had the greater degree of improvement whether or not they were treated in the first 10 days after the onset of the hearing loss or between 11 and 30 days. However, only a small percentage of patients returned to hearing thresholds prior to the damage. In fact, from the univariable and multivariable models used, it seemed that the association of HBO therapy with fair recovery was stronger than the one with recovery in general, suggesting that HBO may be less effective to achieve a complete recovery compared to a partial one.
Regardless of the initial nature of the damage (vascular, viral or autoimmune) decreased cellular oxygenation is an important pathogenetic step in the development of SSHL [19]. It has also been demonstrated that perilymphatic oxygen tension decreases significantly in patients with sudden hearing loss [20]. In fact, a decreased blood flow is followed by a reduced pO2 of the inner ear fluids, which supply nourishment to the organ of Corti [21].
These factors led to the use of HBO as a way to increase cochlear and neural oxygenation. Since the first investigations in 1960, many studies have shown that HBO therapy may produce an increase as high as 125 % in blood oxygen content and increase the oxygen tension in plasma and other tissue fluids [22]. Moreover, HBO may have an effect not only directly on the damaged area but also on the perilesioned penumbra, where ischemic events lead to induction of hypoxia-induced factor 1a and delayed neuronal apoptosis. HBO diminishes the expression of hypoxia-induced factor 1a and its target genes [23]. HBO has a well-documented healing effect [24] that makes it a useful therapy for diabetic wounds or compromised flaps and grafts [23]. In fact, plasmatic oxygen works as an angiogenic stimulus, influencing the formation of new blood vessels from local endothelial cells and stimulating the recruitment and differentiation of circulating stem/progenitor cells (SPCs) [24]). Such effect may contribute to reestablish the circulation of the damaged cochlea which is believed to be unpaired in SSHL, primarily or secondarily, due to compression caused by the inflammatory edema. Furthermore HBO has an anti-inflammatory power, mediated by a decreased production of interleukins (IL)-1, -1B, -6, cyclooxygenase, prostaglandin E-2 [19, 25] and an overproduction of anti-inflammatory cytokine IL-10.
HBO can be administered soon after the onset of SSHL as a primary treatment [26], alone or in association with pharmaceutical treatment [15], or as a secondary treatment [27]. However, HBO administered as a primary treatment, with no combination with other drugs, seems to be less effective than systemic corticosteroids [15]. For this reason, the initial treatment of choice for SSHL is usually based on systemic corticosteroids. When there is no response or when recovery is unsatisfactory, HBO, IT steroids, or other forms of “salvage therapy” may be offered. Several studies report that when HBO is administered as a rescue therapy significant improvement of hearing thresholds can be obtained [19, 26–29]. A recent study where “salvage” HBO was compared to “salvage” IT steroids shows that there were no significant differences between the two treatments [30]. IT steroids are cheaper and can be administered directly in the hospital, with a saving of time. However, some patients have significant ear pain during treatment and choose to drop the treatment. On the other hand, HBO can cause claustrophobia and ear pain as well, especially in those patients who have equalization problems due to poor Eustachian tube function. In our hospital, we do not have experience in performing IT injections and we have to refer patients to other centers.
The effect of spontaneous recovery that has been reported to be ranging from 3 to 60 % [31] and is possible within an average of 4 months after the treatment [32].could significantly impact the outcome measurements in HBO salvage treatment. There are few studies using a control group to evaluate the effect of spontaneous recovery. Ohno [33] carried out a retrospective case–control study on patients treated with HBO as a salvage ≥4 weeks after onset of ISSNHL and found non-significant difference in hearing improvement compared to patients treated with systemic corticosteroids, vitamins and adenosine triphosphate treated within 4 weeks after onset of ISSNHL. Even if cases of patients successfully treated with HBO have been reported 3 months after the onset of deafness [26], recent studies show that the administration of treatment after 30 days does not lead to significant hearing improvement [19, 33, 34]. One month, therefore, seems to be a more reasonable cut-off to obtain significant recovery and for this reason in our study we included only patients treated within 1 month of onset of SSHL.
Since the first studies on the use of HBO to treat SSHL, it has consistently been demonstrated that the effectiveness of HBO is time-dependent and decreases with increasing delay in administration [26]. In our study as well, we found a negative association between recovery and days after onset.
Due to the diversity of possible causes and heterogeneous patient population with SSHL, it becomes necessary to tailor treatment to each patient. To do this we sought to identify how the presenting degree of initial hearing loss could influence the final outcome. Patients with initial profound hearing loss have been reported to have a better outcome, in terms of absolute hearing gain [29] and also in terms of recovery [17]. We were not surprised then too seeing a negative association between recovery and having a mild hearing loss. Most patients with profound deafness choose to be further treated with HBO (7 patients in the study group vs. 2 patients in the control group had profound deafness). Even if the differences between the control group and the study group were not statistically significant in terms of initial hearing loss, we can assume that patients with worse hearing are more prone to accept the expenses related to the therapy. The fact that we found that patients with worse hearing had the greater degree of improvement may have biased the results toward more benefit in the HBOT group. We can also hypothesize that patients with worse initial degree of hearing loss may also be affected by a form of SSHL, which respond better to hyperbaric oxygen. We used stratification to see if the effect of HBO was modified by the initial presentation. The OR for recovery and PTA gain were similar in the two groups (profound and severe vs. moderate and mild hearing loss), suggesting that there was no effect modification. Also previous studies [19, 29, 35] report that HBOT is more effective in patients with worse initial hearing level, whereas Cvorovic et al. [30] showed, in a retrospective series of 541 patients treated with steroids and carbogen, that the severity of initial hearing loss is a negative prognostic factor.
Older age may represent a risk factor for microvascular pathologies [36] and ischemia, which generally negatively influence recovery, but it may also be related to a greater improvement in those patients who receive HBO. In fact, other studies [19, 34] found that older patients respond better to HBO. Being male was positively associated with HBO in the profound and severe hearing loss stratum, and also in one of the multivariable models. We could not explain these findings, which may be due to chance, or indicate the presence of effect modification or confounding. In fact, when we measured the association between HBO and recovery stratified by sex, we noticed that OR were higher in the female stratum, which may indicate that the effect of HBO is modified by sex.
During the HBO treatment, four patients had middle ear barotrauma and one patient suffered of confinement anxiety. Eustachian tube dysfunction is the most common complication of HBO as showed in previous studies [16] and in some cases it may require the positioning of ventilation tubes. In our study, we managed the middle ear barotrauma by slowing the compression speed and with application of topical decongestants.
This study is subject to a number of limitations. Firstly, there was no randomization and the control group was composed of patients who refused the treatment. A selection bias may have had an important influence, due to the fact that in our region, the use of HBO for disorders of the inner ear is not financed by the Health Ministry and patients have to cover entirely the expenses, that are approximately 800 € for 15 sessions. Moreover, socio-economic status may have an influence on the causes or predisposing factors of SSHHL. Secondly, simply measuring the hearing thresholds after the treatment showed us mainly absolute values of hearing gain that may not reflect a real improvement on patients’ quality of life. In particular, we did not investigate speech perception and the presence of concomitant symptoms such as tinnitus and feeling of pressure in the interested ear. Moreover, we did not submit our patients to any questionnaire, such as the short Form-36 Health Survey Update (SF-36) questionnaire, which can be used to evaluate the impact of selective standard therapy on quality of life [37]. Finally, the number of patients enrolled may have resulted in a loss of power, especially when stratification was used.
In conclusion, when primary steroid therapy fails there is not a definite and unique successful treatment regimen; however, further treatment should be offered to patients. This prospective non-randomized clinical study showed that hyperbaric oxygen therapy can lead to significant improvement of pure tone hearing thresholds in patients with SSHL who failed primary corticosteroid treatment and were within 4 weeks of the onset of deafness. During this period of time, the delay of treatment does not influence the outcome, allowing favorable results even after 10 days of onset.
We felt that a control group without any treatment at all was not ethical; therefore, we decided to carry out our study maintaining the oral steroids for both populations. Ideally, a randomized controlled study should include larger sample and a study group of patients receiving HBO with no personal charges. We recommend also that future research focuses on speech reception thresholds and quality of life assessment.
References
Byl FM Jr (1984) Sudden hearing loss: eight years’ experience and suggested prognostic table. Laryngoscope 94:647–661
Teranishi M, Katayama N, Uchida Y, Tominaga M, Nakashima T (2007) Thirty-year trends in sudden deafness from four nationwide epidemiological surveys in Japan. Acta Otolaryngol 127:1259–1265
Klemm E, Deutscher A, Mösges R (2009) A present investigation of the epidemiology in idiopathic sudden sensorineural hearing loss. Laryngorhinootologie 88:524–527
Mattox DE, Simmons FB (1977) Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol 86:463–480
Cadoni G, Fetoni AR, Agostino S, De Santis A, Manna R, Ottaviani F, Paludetti G (2002) Autoimmunity in sudden sensorineural hearing loss: possible role of anti-endothelial cell autoantibodies. Acta Otolaryngol Suppl 548:30–33
Quaranta N, Ramunni A, De Luca C, Brescia P, Dambra P, De Tullio G, Vacca A, Quaranta A (2011) Endothelial progenitor cells in sudden sensorineural hearing loss. Acta otolaryngol 131:347–350 e 4
Labus J, Breil J, Stutzer H, Michel O (2010) Meta-analysis for the effect of medical therapy vs. placebo on recovery of idiopathic sudden hearing loss. Laryngoscope 120:1863–1871
Hughes GB, Kinney SE, Barna BP, Calabrese LH (1984) Practical versus theoretical management of autoimmune inner ear disease. Laryngoscope 94:758–767
Wilson WR, Byl FM, Laird N (1980) The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol 106:772–776
Parnes LS, Sun AH, Freeman DJ (1999) Corticosteroid pharmacokinetics in the inner ear fluids: an animal study followed by clinical application. Laryngoscope 109:1–17
Wu HP, Chou YF, Yu SH, Wang CP, Hsu CJ, Chen PR (2011) Intratympanic steroid injections as a salvage treatment for sudden sensorineural hearing loss: a randomized, double-blind, placebo-controlled study. Otol Neurotol 32:774–779
Imsuwansri T, Poonsap P, Snidvongs K (2012) Hyperbaric oxygen therapy for sudden sensorineural hearing loss after failure from oral and intratympanic corticosteroid. Clin Exp Otorhinolaryngol 5(Suppl):S99–S102
Bianchin G, Russi G, Romano N et al (2010) Treatment with HELP- apheresis in patients suffering from sudden sensorineural hearing loss: a prospective, randomized, controlled study. Laryngoscope 120:800–807
Mazurek B, Haupt H, Georgiewa P, Klapp BF, Reisshauer A (2006) A model of peripherally developing hearing loss and tinnitus based on the role of hypoxia and ischemia. Med Hypotheses 67:892–899
Alimoglu Y, Inci E, Edizer DT, Ozdilek A, Aslan M (2011) Efficacy comparison of oral steroid, intratympanic steroid, hyperbaric oxygen and oral steroid + hyperbaric oxygen treatments in idiopathic sudden sensorineural hearing loss cases. Eur Arch Otorhinolaryngol 268:1735–1741
Fujimura T, Suzuki H, Shiomori T, Udaka T, Mori T (2007) Hyperbaric oxygen and steroid therapy for idiopathic sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol 264:861–866
Liu S-C, Kang B-H, Lee J-C, Lin YS, Huang KL, Liu DW, Su WF, Kao CH, Chu YH, Chen HC, Wang CH (2011) Comparison of therapeutic results in sudden sensorineural hearing loss with/without additional hyperbaric oxygen therapy: a retrospective review of 465 audiologically controlled cases. Clin Otolaryngol 36:121–128
Italian Society of Anesthesia, Analgesia, Resuscitation, Intensive Care (SIAARTI), Italian Society of Undersea and Hyperbaric Medicine (SIMSI), Private Hyperbaric Chambers National Association (ANCIP) Study Group (2007) Guidelines on the indications of hyperbaric oxygen therapy. Sudden deafness. Med Sub Iperb 26:29
Muzzi E, Zennaro B, Visentin R, Soldano F, Sacilotto C (2010) Hyperbaric oxygen therapy as salvage treatment for sudden sensorineural hearing loss: review of rationale and preliminary report. J Laryngol Otol 124:e2
Nagahara K, Fisch U, Yagi N (1983) Perilymph oxygenation in sudden and progressive sensorineural hearing loss. Acta Otolaryngol 96:57–68
Murphy-Lavoie H, Piper S, Moon RE, Legros T (2012) Hyperbaric oxygen therapy for idiopathic sudden sensorineural hearing loss. Undersea Hyperb Med: J Undersea Hyperb Med Soc 39(3):777–792
Boerema I, Meyne NG, Brummelkamp WH et al (1960) Life without blood: a study of the influence of high atmospheric pressure and hypothermia on dilution of the blood. J Cardiovasc Surg 1:133–146
Thom RS (2011) Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg 127(Suppl 1):131S–141S
Gallagher KA, Liu ZJ, Xiao M et al (2007) Diabetic impairments in NO-mediated endothelial progenitor cell mobilization and homing are reversed by hyperoxia and SDF-1 alpha. J Clin Invest 117:1249–1259
Rossignol DA (2007) Hyperbaric oxygen therapy might improve certain pathophysiological findings in autism. Med Hypotheses 68:1208–1227
Lamm K, Lamm H, Arnold W (1998) Effect of hyperbaric oxygen therapy in comparison to conventional or placebo therapy or no treatment in idiopathic sudden hearing loss, acoustic trauma, noise-induced hearing loss and tinnitus: a literature survey. Adv Otorhinolaryngol 54:86–99
Horn CE, Himel HN, Selesnick SH (2005) Hyperbaric oxygen therapy for sudden sensorineural hearing loss: a prospective trial of patients failing steroid and antiviral treatment. Otol Neurotol 26:882–889
Desloovere C, Knecht R, Germonpré P (2006) Hyperbaric oxygen therapy after failure of conventional therapy for sudden deafness. B-ENT 2:69–73
Körpinar S, Alkan Z, Yiğit O, Gör AP, Toklu AS, Cakir B, Soyuyüce OG, Ozkul H (2011) Factors influencing the outcome of idiopathic sudden sensorineural hearing loss treated with hyperbaric oxygen therapy. Eur Arch Otorhinolaryngol 268:41–47
Cvorovic L, Jovanovic MB, Milutinovic Z, Arsovic N, Djeric D (2013) Randomized prospective trial of hyperbaric oxygen therapy and intratympanic steroid injection as salvage treatment of sudden sensorineural hearing loss. Otol Neurotol 34:1021–1026
Rauch SD, Halpin CF, Antonelli PJ et al (2011) Oral vs intratympanic corticosteroid therapy for idiopathic sudden sensorineural hearing loss: a randomized trial. JAMA 25(305):2071–2079
Slattery WH, Fisher LM, Iqbal Z, Liu N (2005) Oral steroid regimens for idiopathic sudden sensorineural hearing loss. Otolaryngol Head Neck Surg 132:5–10
Ohno K, Noguchi Y, Kawashima Y, Yagishita K, Kitamura K (2010) Secondary hyperbaric oxygen therapy for idiopathic sudden sensorineural hearing loss in the subacute and chronic phases. J Med Dent Sci 57:127–132
Bennett MH, Kertesz T, Perleth M, Yeung P, Lehm JP (2012) Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus. Cochrane Database Syst Rev 10:CD004739
Topuz E, Yigit O, Cinar U et al (2004) Should hyperbaric oxygen be added to treatment in idiopathic sudden sensorineural hearing loss? Eur Arch Otorhinolaryngol 261:393–396
Aslan I, Oysu C, Veyseller B, Baserer N (2002) Does the addition of hyperbaric oxygen therapy to the conventional treatment modalities influence the outcome of sudden deafness? Otolaryngol Head Neck Surg 126:121–126
Mosges R, Koberlein J (2009) Rheopheresis for idiopathic sudden hearing loss: results from a large prospective, multicenter, randomized, controlled clinical trial. Eur Arch Otorhinolaryngol 266:943–953
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pezzoli, M., Magnano, M., Maffi, L. et al. Hyperbaric oxygen therapy as salvage treatment for sudden sensorineural hearing loss: a prospective controlled study. Eur Arch Otorhinolaryngol 272, 1659–1666 (2015). https://doi.org/10.1007/s00405-014-2948-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-2948-z