Abstract
Purpose
A first clinical evaluation of a new hand-driven hysteroscopic tissue removal device, Resectr™ 5fr, for office polypectomy without any anesthesia.
Methods
Women with at least one small endometrial polyp were eligible. Hysteroscopic polypectomy was performed using the Resectr™ 5fr in an office setting, without any anesthesia.
Results
One hundred and two hysteroscopic polypectomies were included in the analysis. The median installation time was 1.9 min (95% confidence interval (CI) 1.6–2.1). The median time to complete polyp removal was 1.2 min (95% CI 0.8–1.6). The median surgeon’s safety, practical, and comfort scores on a 5-point Likert scale were high (5 (5–5), 5 (4–5), and 5 (4–5), respectively). Women’s pain score was low (median 1 (0–3)), whereas the satisfaction rate was high (median 5 (5–5)), both on a 5-point Likert scale. There were two conversions (hysteroscopic scissors (n = 1), a new Resectr™ 5fr device (n = 1)). There was one incomplete procedure (tissue hardness).
Conclusion
Hysteroscopic removal of small polyps, using the \({Resectr}^{TM}\) 5fr in an office setting is feasible in terms of installation and resection time. Surgeon’s practical, comfort, and safety scores are high, whereas women report low pain scores and high satisfaction rates.
Trial registration
Dutch Clinical Trial Registry (NTR 7119, NL6923): https://www.trialregister.nl/trial/6923. Date of registration: 27/03/2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hysteroscopic polypectomy using the ResectrTM 5fr in an office setting without any anesthesia is feasible in terms of installation and resection time, surgeon’s convenience and patient’s satisfaction. |
Introduction
Endometrial polyps are focal outgrowths containing glands, stroma, and blood vessels [1]. The most prevalent symptom is abnormal uterine bleeding (AUB) occurring in up to 68% of cases [2]. Their presence has also been linked with female infertility [3]. Nevertheless, they can be asymptomatic [4]. Although endometrial polyps are benign, pre- and malignant transformation may occur in around 3.4% [5]. Hysteroscopic polypectomy is recommended in case of symptoms or in postmenopausal women [3, 6,7,8,9]. The management in asymptomatic premenopausal women is debatable [9,10,11].
Miniaturization of hysteroscopes and its instruments enabled hysteroscopic polypectomy to be performed in an office setting. The first instruments used for office hysteroscopic polypectomy were 5fr mechanical instruments (scissor and grasper), later expanded with 5fr bipolar instruments [12]. These are fragile and have a limited degree of movement. The main restriction is the ratio between the polyp size and the diameter of the internal cervical ostium, which is associated with additional maneuvers for tissue extraction, longer operating times, and higher pain scores [13,14,15]. Mechanical hysteroscopic tissue removal systems offer a solution by their simultaneous cutting and aspiration effect. Compared to 5fr bipolar instruments, a mechanical hysteroscopic tissue removal system is significantly faster, more acceptable, and successful [16, 17].
However, the development of devices continued and a small, hand-driven tissue removal system, \({Resectr}^{TM}\) 5fr. (1.66 mm) (Minerva Surgical, Santa Clara CA), which was CE marked in 2016 and FDA approved in 2020, was launched to perform office hysteroscopic polypectomy. Its benefits are that the electric-powered control unit is replaced by a simple hand grip, which simplifies the setup, and that it fits through a 5fr. working channel. The aim of the current trial was to perform a first clinical evaluation, in accordance with the IDEAL framework, of the device for office polypectomy.
Methods
This multicenter, prospective cohort study was conducted at the Catharina Hospital (Eindhoven, the Netherlands) and the Ghent University Hospital (Ghent, Belgium) from October 2018 until March 2021. The study was approved by the ethical committees of both centers and it was registered at the Dutch Clinical Trial Registry (NL6923). Written informed consent was obtained from all women.
Women were eligible to participate when they had at least one small (mean diameter ≤ 8 mm) endometrial polyp, scheduled for hysteroscopic removal. Diagnosis was made by transvaginal ultrasound, saline infusion sonography (SIS) and/or diagnostic hysteroscopy. Exclusion criteria were endometrial polyps with a mean diameter larger than 8 mm, evidence of malignancy, untreated cervical stenosis, or the presence of a contraindication for operative hysteroscopy.
Hysteroscopic polypectomy was performed in an office setting without any anesthesia. The procedure was done immediately after diagnosis (‘see and treat’) or scheduled according to local circumstances and patient’s preference. Women were allowed to take oral analgesia according to local practices (no standard protocol at the Ghent University Hospital, non-steroidal anti-inflammatory drug (NSAID) (Naproxen® 500 mg) the night before the procedure at the Catharina Hospital). The vaginoscopic approach was used without cervical preparation. Normal saline, warmed to 37.0 °C, was used as distention medium and delivered by a pressure bag or the ENDOFLOW®II Warming, Irrigation and Suction system (Rocamed). No antibiotic prophylaxis was administered.
Polyp removal was performed using the \({Resectr}^{TM}\) 5fr., a new hand-driven tissue removal device, consisting of a 35 cm long cannula and, a 5 mm working window, and an internal rotating blade in an outer tube (Fig. 1). The device was introduced into the uterine cavity through the 5fr. working channel of pre-existing small diameter hysteroscope (≤ 15fr, ≤ 5 mm). The hand activation of the \({Resectr}^{TM}\) 5fr. replaces the electric-powered control unit in the existing motor-driven devices. Each squeeze in the handpiece initiates six turning movements of the inner blade (3 rotations clockwise, followed by 3 rotations counterclockwise). During each turn, the inner blade can cut tissue. The ENDOMAT® SELECT (Karl Storz, Tuttlingen, Germany; maximum flow setting of 300 mL/min), activated by a foot pedal, was used for controlled suction of the resected tissue, which is aspirated through the hollow lumen of the tissue removal device, collected in a pouch and available for pathology analysis. When the rotating inner blade and the ENDOMAT® SELECT are not activated, the window opening of the \({Resectr}^{TM}\) 5fr. is always closed to prevent fluid loss and uterine cavity collapse.
The procedures were done by four experienced hysteroscopic surgeons after in vitro training.
Women were scheduled for a postoperative visit (telephone or physical) 6 weeks after the operative hysteroscopy.
The primary outcomes are the installation and resection times. Installation time was defined as the time to set up the hysteroscopic instrumentation ready for use at the back table (assembling the hysteroscope by connecting camera light cable and irrigation system, connecting the ENDOMAT® SELECT tubing to the \({Resectr}^{TM}\) 5fr and insertion of the device in the 5fr working channel). Resection time was defined as the time from first instrument activation until complete removal of the largest polyp.
The secondary outcomes were the surgeon’s practical, comfort, and safety scores on a 5-point Likert scale, patient’s pain (after the procedure) and satisfaction scores (at 6-week follow-up) (5-point Likert scale), conversion rates (an interruption of the hysteroscopic procedure to switch to another procedure or another device to complete the surgery), completeness of removal (extraction of all polyp tissue from the uterine cavity), intra- and postoperative complications (including fluid deficit ≥ 2500 mL with clinical consequences, hemorrhage (> 500 mL), uterine perforation, infection), short-term effectiveness (persistence of symptoms at 6-week follow-up), postoperative availability of tissue for pathology analysis and pathology diagnosis.
The intended sample size was set at 100 procedures.
Statistical analyses
Data was collected and analyzed using the statistical program SPSS (version 27.0, IBM Corp., Armonk, NY). Continuous variables were summarized with descriptive statistics (mean and standard deviation for data normally distributed and median and interquartile range (IQR) otherwise). Categorical data was presented as frequency and percentage.
Kaplan–Meier estimates for time to installation and time to complete polyp removal were plotted with the log–log 95% confidence interval (CI). The median time to installation is the earliest time at which at least 50% of the installations were accomplished. The median time to complete polyp removal is the earliest time at which at least 50% of the polyps were completely removed. The value for the variable of interest is used regardless of whether or not the intercurrent event occurs (treatment policy strategy). Correlation between 2 variables was evaluated with Spearman’s correlation. Numerical data was analyzed using the Mann–Whitney U test and Kruskal–Wallis test to compare 2 or more than 2 groups. Categorical data was analyzed using the chi-square test. It concerns post hoc analyses that were not predefined. Level of significance was set at P < 0.05.
Results
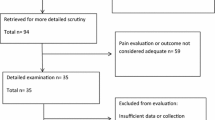
One hundred and twelve women were enrolled in the study (Fig. 2). Conscious sedation and general anesthesia were performed in one and five cases respectively, because of patient’s preference or a painful diagnostic hysteroscopy after inclusion. Finally, 102 hysteroscopic polypectomies, using the \({Resectr}^{TM}\) 5fr in an office setting without any anesthesia, were included in the analysis.
Patient demographics and polyp characteristics are shown in Tables 1 and 2, respectively. One woman had an ASA III score because of a previous kidney transplant.
Surgery data is summarized in Table 3. The time to installation curve and the time to complete polyp resection curve are shown in Figs. 3 and 4 respectively. The median installation time was 1.9 min (95% CI 1.6–2.1). The median time to complete polyp removal was 1.2 min (95% CI 0.8–1.6). There was no significant difference in resection times among the four surgeons (P = 0.21). The surgeon’s practical and comfort scores were negatively correlated with resection times (P < 0.001). Sixty-six percent of the women took pain medication within a time frame from the night before until the morning of the procedure (paracetamol 500 mg (n = 2), paracetamol 1000 mg (n = 9), paracetamol + codeine (n = 1), paracetamol + NSAID (n = 2), and NSAID (n = 53)). Pain scores were overall very low, and women who took pain medication reported significantly lower pain scores (P = 0.009). A significant correlation between patients pain score and resection time could not be found (P = 0.09).
One hysteroscopic procedure was discontinued because the polyp tissue located at the posterior wall was too hard, with the inability to remove the base. Tissue hardness suggested the presence of a myoma. The resection time was 7.4 min with a fluid deficit of 300 mL. The woman was rescheduled for a hysteroscopic polypectomy using the resectoscope in an inpatient setting. This procedure was uneventful and pathology analysis confirmed the presence of a polyp. In two cases, the \({Resectr}^{TM}\) device became nonfunctional. In one case, the hand piece became unusable and the device was converted to hysteroscopic scissors to completely remove a polyp located at the posterior wall. The resection time was 7.1 min. Fluid deficit was not recorded. Pathology analysis confirmed the presence of a polyp. In the other case, the \({Resectr}^{TM}\) device had a defective inner blade. With a new device, the polyp, located at the posterior wall, was removed completely without complications. The resection time was 5.4 min with a fluid deficit of 50 mL. Polyp tissue was confirmed on pathology analysis.
Tissue was not available for pathology analysis in one case because of a small amount of tissue, but non-malignant polyp tissue was already confirmed on biopsy during the diagnostic phase.
No intraoperative complications were recorded.
Postoperative data are shown in Table 4. Eleven percent still complained of blood loss and/or pain. New symptoms were reported in 3% (blood loss (n = 1), pain (n = 1), and dysmenorrhea (n = 1)). Polyps were confirmed in 88%.
One woman contacted her gynecologist earlier than the planned postoperative visit because of blood loss. The polyp was located at the posterior wall and resected in 0.9 min. An intrauterine device was placed at the time of the surgery, but it was expulsed after 1 month. This patient was already known with heavy menstrual bleeding. She was admitted for 2 nights and received packed cells because of a hemoglobin drop to 7.4 mg/dL. She was treated with NSAIDS, oral progestogens, and tranexamic acid, but eventually a hysterectomy was performed. Two women contacted their general practitioner before the planned postoperative visit (pyrosis (n = 1), tiredness (n = 1)).
Discussion
Hysteroscopic polypectomy in an office setting using a new hand-driven tissue removal device, \({Resectr}^{TM}\) 5fr, is feasible in terms of installation and resection time. To our knowledge, this is the first report on its clinical use.
Installation and resection times were short. The reported installation times associated with mechanical hysteroscopic tissue removal systems (median 5.2 min) and resectoscopic surgery (median 4.5 min) were longer [18]. This is explained by the simplified setup of the hand-driven tissue removal device. Our resection times were incomparable with those reported in literature using 5fr. mechanical instruments, 5fr. bipolar instruments, mechanical hysteroscopic tissue removal systems and resectoscopic surgery in an office setting, because of heterogeneity in time definitions, polyp sizes, and polyp numbers [13, 14, 16, 17, 19,20,21,22,23,24]. Our procedures were done by four experienced surgeons, with two surgeons performing more interventions. Still, there was no indication that resection times were different among the surgeons. It is already known that mechanical hysteroscopic tissue removal systems have a shorter learning curve compared to bipolar electrosurgery [17, 25].
The surgeon’s practical, comfort, and safety scores were high. These scores were not yet reported on before in an office setting. Van Dongen et al. reported surgeon and trainer convenience scores on a visual analog scale (VAS), which was in favor of the mechanical hysteroscopic tissue removal system compared to resectoscopic surgery [25]. Tsuchiya et al. reported surgeon convenience with a mechanical hysteroscopic tissue removal system and resectoscopic surgery in terms of maneuverability of the device, easiness of removal, and visibility on a VAS scale [26]. VAS scores were 7.7, 8.4, and 7.8 for the mechanical hysteroscopic tissue removal system and 7.2, 6.5, and 6.4 for resectoscopic surgery, respectively. Stoll et al. reported surgeon’s comfort scores on a VAS scale of 8.4 and 7.4 for the mechanical hysteroscopic tissue removal system and resectoscopic surgery, respectively [27].
Patients reported low pain scores and high satisfaction scores. The reported pain scores using 5r. mechanical instruments, 5fr. bipolar instruments, mechanical hysteroscopic tissue removal systems, and resectoscopic surgery in an office setting are heterogeneous in terms of measure point (during or after the procedure), measure scale (10 or 100 VAS scale), and analgesia use [16, 17, 20,21,22,23,24, 28,29,30]. The highest median score on a 10-point VAS scale was 3.6 using 5fr. mechanical instruments [21]. The highest median score on a 100-point VAS scale was 52.0 using 5fr bipolar instruments [16]. A Cochrane meta-analysis showed no good-quality evidence of a clinically meaningful difference in safety or effectiveness between different types of pain relief compared with each other, with placebo, or with no treatment in women undergoing a diagnostic hysteroscopy [31]. A more recent meta-analysis of pain relief during diagnostic and operative hysteroscopy recommended NSAIDs to reduce pain during and after the procedure [32]. However, a major limitation of this meta-analysis is the methodologic and clinical heterogeneity. Conflicting results exist whether mechanical polypectomy is associated with lower VAS scores than electrosurgical resection [16, 17, 20, 33]. The reported satisfaction rates for hysteroscopic polypectomy in an office setting were 92.5 on a 100-point VAS scale and 97.5% indicated that they were ‘very satisfied’ using a mechanical hysteroscopic tissue removal system [22, 24].
There were particularities in three cases. It is remarkable that in all cases the polyp was located posteriorly, whereas it is known that fundal polyps may be hard to reach. A difficult resection of hard tissue may suggest that the device is not suitable for myomectomy. Device deficiency may reflect its fragility as well as the unsuitability to resect harder tissue. Conversion rates regarding hysteroscopic polypectomy in an office setting were not yet reported before. The reported complete polyp resection rates using 5fr mechanical and 5fr bipolar instruments and mechanical hysteroscopic tissue removal systems ranged from 77% to 97.5% [16, 17, 24, 28]. The odds ratio (OR) for complete polyp resection was significantly higher using the mechanical hysteroscopic tissue removal system compared to 5fr bipolar instruments (OR 12.5 (1.5–100.6)) [16]. Most studies on hysteroscopic polypectomy in an office setting, using 5fr mechanical and 5fr bipolar instruments, mechanical hysteroscopic tissue removal systems, or resectoscopic surgery were without complications [19, 20, 23, 24, 34]. Reported complications are vasovagal response, vomiting, pain, and cervical tears [14, 16, 22, 28].
There was no tissue available to send for pathology analysis in one case. This was one of the first procedures. The ENDOMAT® SELECT tubing set is long and it should be flushed to remove the tissue, especially if it contains a small amount of tissue. This was therefore performed in all consecutive procedures. Tissue availability related to other hysteroscopic techniques was not yet reported on before.
Our study has some limitations. First, pain medication was not standardized and not blinded. This could have influenced our results (low pain scores, high satisfaction rates). Nevertheless, this corresponds with the reality in clinical practice. No procedure had to be discontinued because of pain. The pain medication that was taken is non-invasive and safe. Second, surgeon-reported outcomes may be subjective, but it was multicentric and different surgeons were involved. Third, we did not take the cost into account. Fourth, only smaller polyps were included. However, this size was chosen because it corresponds with the diameter of the internal cervical ostium which is within the feasible range of 5fr mechanical instruments. Lastly, we did not have a control group. Whether a randomized controlled trial (RCT) is worth the effort is, in accordance with the IDEAL framework, evaluated through this feasibility study.
Future research focusing on hysteroscopic polypectomy in an office setting should be conducted. The \({Resectr}^{TM}\) 5fr and 5fr. mechanical instruments should be compared in terms of clinical and cost-effectiveness. The maximum polyp size suitable for resection with the \({Resectr}^{TM}\) 5fr should be determined and subsequently a comparison with 5fr bipolar instruments should be done. In addition, other indications should be examined (targeted biopsy and retained products of conception).
In conclusion, hysteroscopic removal of polyps with mean diameter ≤ 8 mm, using the \({Resectr}^{TM}\) 5fr in an office setting, is feasible in terms of installation time and resection time. The surgeon’s practical, comfort, and safety scores are high, whereas women report low pain scores and high satisfaction rates. Future research should be conducted focusing on the comparison with other techniques and other indications.
Data availability
Data available on request due to privacy/ethical restrictions.
References
Clark TJ, Stevenson H (2017) Endometrial polyps and abnormal uterine bleeding (AUB-P): what is the relationship, how are they diagnosed and how are they treated? Best Pract Res 40:89–104
Golan A, Sagiv R, Berar M, Ginath S, Glezerman M (2001) Bipolar electrical energy in physiologic solution–a revolution in operative hysteroscopy. J Am Assoc Gynecol Laparosc 8(2):252–258
Bosteels J, van Wessel S, Weyers S, Broekman F, D’Hooghe T, Bongers M et al (2018) Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009461.pub4
Di Spiezio SA, Calagna G, Guida M, Perino A, Nappi C (2015) Hysteroscopy and treatment of uterine polyps. Best Pract Res Clin Obstet Gynaecol 29(7):908–919
Sasaki LMP, Andrade KRC, Figueiredo ACMG, da Wanderley MS, Pereira MG (2018) Factors associated with malignancy in hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol 25:777–785
John Jude A, Joseph A, Elizabeth B (2012) The management of endometrial polyps in the 21st century. Obstet Gynaecol 1:33–38
Nathani F, Clark TJ (2006) Uterine polypectomy in the management of abnormal uterine bleeding: a systematic review. J Minim Invasive Gynecol 13(4):260–268
Tanos V, Abigail Z (2019) Best practice & research clinical obstetrics and gynaecology uterine scar rupture–prediction, prevention, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol 59:115–131
Uglietti A, Buggio L, Farella M, Chiaffarino F, Dridi D, Vercellini P et al (2019) European journal of obstetrics & gynecology and reproductive biology the risk of malignancy in uterine polyps : a systematic review and. Eur J Obstet Gynecol 237:48–56
American Association of Gynecologic Laparoscopists (2012) AAGL practice report: practice guidelines for the diagnosis and management of endometrial polyps. J Minim Invasive Gynecol 19(1):3–10
Vitale SG, Haimovich S, Lagana AS, Alonso L, Di Spiezio SA, Carugno J (2021) Endometrial polyp. An evidence-based diagnosis and management guide. Eur J Obstet Gynecol Reprod Biol 260:70–77
Sardo ADS, Rudi C (2022) State-of-the-Art hysteroscopic approaches to pathologies of the genital tract. Endo-Press, Germany
Bettocchi S, Ceci O, Nappi L, Di Venere R, Masciopinto V, Pansini V et al (2004) Operative office hysteroscopy without anesthesia: analysis of 4863 cases performed with mechanical instruments. J Am Assoc Gynecol Laparosc 11(1):59–61
Litta P, Cosmi E, Saccardi C, Esposito C, Rui R, Ambrosini G (2008) Outpatient operative polypectomy using a 5 mm-hysteroscope without anaesthesia and/or analgesia: advantages and limits. Eur J Obstet Gynecol Reprod Biol 139(2):210–214
Gambadauro P, Martínez-Maestre MA, Torrejón R (2014) When is see-and-treat hysteroscopic polypectomy successful? Eur J Obstet Gynecol Reprod Biol 178:70–73
Smith PP, Middleton LJ, Connor M, Clark TJ (2014) Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol 123(4):745–751
Pampalona JR, Bastos MD, Moreno GM, Pust AB, Montesdeoca GE, Guerra Garcia A et al (2015) A comparison of hysteroscopic mechanical tissue removal with bipolar electrical resection for the management of endometrial polyps in an ambulatory care setting: preliminary results. J Minim Invasive Gynecol 22(3):440–445
Hamerlynck TWO, Schoot BC, Van Vliet HAAM, Weyers S (2015) Removal of endometrial polyps: hysteroscopic morcellation versus bipolar resectoscopy, a randomized trial. J Minim Invasive Gynecol 22(7):1237–1243
Bettocchi S, Ceci O, Di Venere R, Pansini MV, Pellegrino A, Marella F et al (2002) Advanced operative office hysteroscopy without anaesthesia: analysis of 501 cases treated with a 5 Fr. bipolar electrode. Hum Reprod 17(9):2435–2438
Garuti G, Centinaio G, Luerti M (2008) Outpatient hysteroscopic polypectomy in postmenopausal women: a comparison between mechanical and electrosurgical resection. J Minim Invasive Gynecol 15(5):595–600
Cicinelli E, Tinelli R, Loiudice L, Loiudice I, Quattromini P, Fusco A et al (2011) AlphaScope vs lens-based hysteroscope for office polypectomy without anesthesia: randomized controlled study. J Minim Invasive Gynecol 18(6):796–799
McIlwaine P, McElhinney B, Karthigasu KA, Hart R (2015) A prospective study of the use of the myosure resectoscope to manage endometrial polyps in an outpatient setting. Aust New Zeal J Obstet Gynaecol 55(5):482–486
Dealberti D, Riboni F, Cosma S, Pisani C, Montella F, Saitta S et al (2016) Feasibility and acceptability of office-based polypectomy with a 16f mini-resectoscope: a multicenter clinical study. J Minim Invasive Gynecol 23(3):418–424
Ceci O, Franchini M, Cannone R, Giarrè G, Bettocchi S, Fascilla FD et al (2019) Office treatment of large endometrial polyps using truclear 5C: feasibility and acceptability. J Obstet Gynaecol Res 45(3):626–633
van Dongen H, Emanuel MH, Wolterbeek R, Trimbos JB, Jansen FW (2008) Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol 15(4):466–471
Tsuchiya A, Komatsu Y, Matsuyama R, Tsuchiya H, Takemura Y, Nishii O (2018) Intraoperative and postoperative clinical evaluation of the hysteroscopic morcellator system for endometrial polypectomy: a prospective, randomized, single-blind, parallel group comparison study. Gynecol Minim Invasive Ther 7(1):16–21
Stoll F, Lecointre L, Meyer N, Faller E, Host A, Hummel M et al (2021) Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minim Invasive Gynecol 28(4):801–810
Garuti G, Cellani F, Colonnelli M, Grossi F, Luerti M (2004) Outpatient hysteroscopic polypectomy in 237 patients: feasibility of a one-stop “see-and-treat” procedure. J Am Assoc Gynecol Laparosc 11(4):500–504
Marsh FA, Rogerson LJ, Duffy SRG (2006) A randomised controlled trial comparing outpatient versus daycase endometrial polypectomy. BJOG An Int J Obstet Gynaecol 113(8):896–901
Gordon HG, Mooney S, Readman E (2020) Introduction of the MyoSureLITE in an established outpatient hysteroscopy clinic. Aust New Zeal J Obstet Gynaecol 60(5):784–789
Ahmad G, Saluja S, O’Flynn H, Sorrentino A, Leach D, Watson A (2017) Pain relief for outpatient hysteroscopy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007710.pub3
De SPM, Mahmud A, Smith PP, Clark TJ (2020) Analgesia for office hysteroscopy: a systematic review and meta-analysis. J Minim Invasive Gynecol 27(5):1034–1047
De Silva PM, Stevenson H, Smith PP, Clark TJ (2021) Pain and operative technologies used in office hysteroscopy: a systematic review of randomized controlled trials. J Minim Invasive Gynecol 28(10):1699–1711
Papalampros P, Gambadauro P, Papadopoulos N, Polyzos D, Chapman L, Magos A (2009) The mini-resectoscope: a new instrument for office hysteroscopic surgery. Acta Obstet Gynecol Scand 88(2):227–230
Acknowledgements
Unrestricted grant from Boston Scientific.
Funding
Unrestricted grant from Boston Scientific.
Author information
Authors and Affiliations
Contributions
Steffi: protocol development, data collection, data management, statistical analysis, data interpretation, manuscript writing, manuscript editing. Tjalina, Huib, Steven, Benedictus: protocol development, data collection, data interpretation, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Huib van Vliet and Benedictus Schoot report personal fees from Medtronic for lectures and consulting on hysteroscopic morcellation, outside the submitted work. Steffi van Wessel, Tjalina Hamerlynck and Steven Weyers have nothing to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Ghent University hospital (09/01/2018).
Consent to participants
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Wessel, S., Hamerlynck, T., van Vliet, H. et al. Clinical evaluation of a new hand-driven hysteroscopic tissue removal device, Resectr™ 5fr, for the resection of endometrial polyps in an office setting. Arch Gynecol Obstet 308, 893–900 (2023). https://doi.org/10.1007/s00404-023-06995-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06995-w