Abstract
Introduction and hypothesis
The objective of this trial was to evaluate whether avoiding episiotomy can decrease the risk of advanced perineal tears.
Material and methods
In this randomized (1:1) parallel-group superiority trial, primiparous women underwent randomization into standard care (155 cases) vs. no episiotomy (154 cases) groups. The primary endpoint was the incidence of advanced (3rd- and 4th-degree) perineal tears. Secondary outcomes included perineal integrity, suturing characteristics, second-stage duration, incidence of postpartum hemorrhage, neonatal variables, and various postpartum symptoms 2 days and 2 months after delivery.
Results
At prespecified 1-year interim analysis, the groups did not differ in terms of baseline demographic and obstetric characteristics. Six advanced perineal tears (3.9%) were diagnosed in the standard care group vs. two in no episiotomy group (1.3%), yielding a calculated odds ratio (OR) of 0.33 [95% confidence interval (CI) 0.06–1.65). Unexpectedly, rates of episiotomy performance also did not significantly vary between groups: 26.5% (41 cases) vs. 21.4% (33 cases), respectively, p = 0.35. No significant differences were noted in any secondary outcomes.
Conclusions
No difference in the rates of advanced perineal tears was found between groups; however, the main limitation of our study was unexpectedly high rates of episiotomy in the nonepisiotomy group. Thus, the main conclusion is that investigator monitoring and education should be continuously practiced throughout the trial duration, stressing the importance of adherence to the protocol.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Episiotomy is one of the most prevalent surgical interventions at the delivery room, ranging in frequency from <10 to 75% of vaginal births [1, 2]. Presumed benefits of this procedure include preventing advanced (3rd- and 4th-degree) perineal tears by using lateral or mediolateral incision types, easier suturing, decreased postpartum pelvic organ injury, and facilitation of labor in cases of fetal distress or shoulder dystocia [3]. However, cumulative evidence over recent decades strongly indicates the lack of episiotomy efficiency. Moreover, many studies indicate that episiotomy may exacerbate maternal morbidity in terms of postpartum bleeding and pain, urinary incontinence, and risk for severe perineal tears [4,5,6]. In 2009, Cochrane Collaboration meta-analysis of randomized controlled trials demonstrated that compared with routine episiotomy use, selective episiotomy significantly decreases the risk of advanced perineal tears [relative risk (RR) 0.67} and overall need for perineal suturing (RR 0.71) [7]. Later systematic reviews demonstrated no solid evidence for performing episiotomy in classical indications of vacuum extraction or for preventing shoulder dystocia [8, 9]. One of the most common reasons for performing an episiotomy is the indistinct indication of imminent tear [3]. Indeed, anal sphincter injury is one of the most devastating obstetric complications; however, the decision to perform episiotomy for preventing advanced tear is mostly based on previous experience of the attending obstetrician, such as characteristic perineal parameters, with lack of any scientific evidence supporting this management.
In accordance with Cochrane Collaboration meta-analysis, we hypothesized that avoiding episiotomy, compared with selective episiotomy use, may be related to decreased risk of advanced perineal tears, with no notable effect on other obstetric complications. Thus, the objective of our study was to compare maternal and neonatal outcomes between deliveries in which episiotomy was avoided and selective episiotomy during delivery. We here present results of a 1-year interim analysis.
Material and methods
This randomized (1:1) parallel-group superiority trial commenced on 31 May 2015 in Bnai-Zion Medical Center, Haifa, Israel. Trial design was established following consultations with certified epidemiologist with an extensive experience in clinical trials, in accordance with the Consolidated Standards of Reporting Trials (CONSORT) Guidelines for Reporting Parallel Group Randomized Trials [10]. The trial was registered at ClinicalTrials.gov, number NCT02356237. No changes to methods of determining outcomes were introduced after trial commencement. The research protocol was approved by the Institutional Review Board Ethics Committee for Human Subjects (protocol number 125-14BNZ, 18 January 2015), and all participants gave written informed consent.
Bnai-Zion Medical Center is one of the three major hospitals in Haifa and performs ~ 3000 annual deliveries, with a baseline episiotomy rate of 14.3%. Pregnant women were recruited during labor, at scheduling for induction of labor, or when attending for a routine follow-up examination during third trimester of pregnancy and intending to give birth at the participating hospital. Recruitment was performed by obstetric personnel registered as investigators in the Institutional Review Board Committee. We included women experiencing their first vaginal delivery (including trial of labor after cesarean section), with a singleton pregnancy of > 34 gestational weeks, vertex presentation, with no absolute contraindications for vaginal delivery. Parturients underwent randomization into one of two groups:
-
1.
Control group: in which the decision to perform episiotomy was based on routine delivery care (i.e., at the discretion of the attending caregiver).
-
2.
Study group: in which no episiotomy was performed. Deviation from protocol and episiotomy performance in this group were allowed only at the discretion of the obstetrician in charge of the delivery and only in cases of unequivocal benefit to the fetus (mainly at times of significant fetal distress).
Randomization sequencing was carried out using computer software generating random numbers with a 1:1 allocation using random block sizes of six. Details of the series were unknown to any researcher enrolling and assessing participants or to the coordinator, and the allocation sequence was concealed by sequentially numbered, opaque, and sealed envelopes. The appropriately numbered envelope was attached to the participant’s portfolio during enrolment and opened only during the second stage of labor.
Mediolateral or lateral episiotomy (according to the accepted management in each medical center) was performed during the crowning stage. The incision was cut at an angle of 45–60° for 3–4 cm in length. Primary outcome was the incidence of advanced (3rd- and 4th-degree) perineal tears diagnosed by an attending midwife or obstetrician and confirmed by a senior obstetrician immediately after delivery. Secondary outcome measures were:
-
1st- and 2nd-degree perineal tears (episiotomy was considered as a 2nd-degree tear)
-
Duration of the second stage
-
Frequency of postpartum hemorrhage (defined as subjective evaluation > 500 ml or with hemodynamic instability) during the first hour after the delivery
-
Neonatal 1- and 5-min Apgar scores
-
Cord blood pH at birth collected just after delivery (if taken)
-
Need for neonatal resuscitation from birth until 1 h after delivery
-
Frequency of admission to neonatal intensive care unit (NICU)
-
Shoulder dystocia (defined as a requirement of obstetrical maneuvers for shoulder delivery, or an interval longer than 60 s between delivery of the head to that of the shoulders)
-
Frequency and degree of perineal tears during vacuum delivery
-
Frequency of episiotomy
-
Characteristics of suturing procedure (duration of suturing, number of suture packs used, subjective grading of suturing difficulty, and need for extended suturing in the operation room)
-
Postpartum symptoms 2 days after delivery, including perineal pain evaluation using 11 points (0–10) verbal numeric scale (VNS), urinary retention (for > 6 h after delivery/urinary catheter extraction), perineal infection, perineal hematoma requiring surgical drainage, and symptoms of urinary/anal incontinence
-
Evaluation via phone call 2 months after the delivery using yes or no questions regarding symptoms of urinary/anal incontinence, perineal complications (infection or dehiscence of perineal scar), timing of resumption of sexual activity, perineal pain, and dyspareunia evaluation using the 11-point (0–10) VNS
-
Evaluation via phone call 1 year after delivery by using questionnaires: the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) [11] and the Pelvic Floor Distress Inventory-20 (PFDI-20) [12]. This parameter was not included in this paper, since the relevant data will be available for analysis in June 2017.
Statistical analysis
Initial sample size calculation was performed by a certified statistician with an extensive experience in clinical trials. Based on the assumption that the worldwide rate of advanced perineal tears in the control group is 1.6% (according to the latest data reported at the annual Israeli Maternal and Fetal Medicine Society meeting in November 2014), we calculated a sample size of 14,842 patients to give 80% power, with a two-sided type 1 error of 5% for detecting a 0.67% reduction of RR between study and control groups (based on the above-mentioned Cochrane Collaboration analysis demonstrating RR of 0.67 with selective vs. routine episiotomy use) [7]. To recruit this number of patients, at least a 4-year inclusion period was anticipated. A year after trial initiation, an interim analysis was planned to calculate the up-to-date rate of advanced perineal tears. We planned to recalculate the sample size based on this rate. In case of statistically significant difference in the primary outcome measure (i.e., advanced perineal tears) with a confidence level of 0.003, discontinuation of the trial was to be considered due to demonstrated efficacy. Otherwise, the trial was planned to be continued, with required confidence level at the final statistical calculations of 0.049.
Our primary analysis was conducted using an intent-to-treat approach, and all participating women were included in the primary outcome analysis, including those who underwent episiotomy in the nonepisiotomy protocol. Categorical variables arepresented as numbers with percentages and were compared with the χ2 test using Fisher’s exact significance levels. Dichotomous data (with focus on advanced perineal tears) were extracted in 2 × 2 tables, and odds ratios (OR) with 95% confidence intervals (CI) were calculated. Continuous data are presented as mean ± standard deviation (SD) and analyzed using Student’s t tests. Ordinal variables arereported as median (25–75 percentile) and analyzed using Wilcoxon Mann–Whitney U test. In addition, as a noticeable rate of deviations from protocol was seen, we performed per-protocol analysis to examine the robustness of our primary estimates. Furthermore, subgroup analysis was performed for spontaneous vaginal births and vacuum extraction deliveries. Secondary outcome analysis was performed likewise. As the groups were comparable in terms of demographic and obstetric characteristics, logistic regression analyses were not performed.
Results
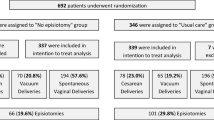
Between 31 May 2015 and 30 May 2016 (predefined period of the interim analysis), we randomly assigned 311 women for allocation into the no episiotomy or standard care group (Fig. 1). One patient in each group asked to be excluded before the allocation and were not included in the analysis.
Baseline demographic and clinical characteristics for each group are presented in Table 1. The groups did not differ in terms of maternal demographic and obstetric factors. In subgroup analysis for spontaneous vaginal birth and vacuum extractions (Supplementary Table 1), higher rates of oxytocin use in no episiotomy vacuum deliveries (87.9 vs. 53.8%, p = 0.0069) was noted.
The two main groups did not differ in terms of delivery outcomes (Fig. 1). Unexpectedly, episiotomy rates also did not significantly vary: 21.4% (33 cases) in no episiotomy vs. 26.5% (41 cases) in standard care (p = 0.35). Indications for the 33 episiotomy procedures in women allocated to no episiotomy care were fetal distress in ten cases, preventing advanced perineal tear in nine, vacuum delivery in seven, shortening second stage of labor in three, preventing shoulder dystocia due to macrosomic fetus in two, and one case excused by no room in perineum. Primary intention-to-treat analysis involved all patients randomly assigned, eliminating the two who asked to be excluded before allocation (Table 2). Compared with selective episiotomy, calculated OR for advanced perineal tears in the no episiotomy group was 0.33 (95% CI 0.06–1.65). In addition, per-protocol analysis was performed for 286 patients, excluding the 23 cases considered a deviation of protocol (all cases of episiotomy performed in the no episiotomy group, excluding the indication of fetal distress). According to per-protocol analysis, the no episiotomy group was associated with an OR of 0.19 (95% CI 0.02–1.60), compared with selective episiotomy approach.
No significant difference was noted in secondary outcomes related to perineal integrity or suturing characteristics (Table 3, Supplementary Tables 2 and 3). One exception was lower rates of episiotomy and a higher proportion of spontaneous perineal tears in the no episiotomy group by per-protocol analysis, with no effect on the rates of intact perineum or total rates of perineal tears by grades. A notable finding was higher rate of spontaneous anterior tears in no episiotomy vacuum deliveries: five of 16 (31.3%) vs. none of ten tears in the control group (p = 0.0488).
The only two additional secondary outcomes yielding statistical significance were shorter second stage in the no episiotomy group and lower rates of urinary retention 2 days after delivery in nonepisiotomy vacuum deliveries by per-protocol analysis (Table 4, Supplementary Table 4). No significant findings were demonstrated in other secondary outcomes.
Discussion
Several randomized controlled trials have explored the role of episiotomy during vaginal delivery [7]. Similarly to our study, most focused on advanced perineal tears as primary outcome. This parameter was chosen, since grades 3 and 4 perineal tears comprise one of the most severe obstetric complications, potentially leading to disabling urinary and anal symptoms [13, 14]. However, the protocol used in former investigations differed from that used in our study, as most studies compared outcomes of routine episiotomy (a prevailing practice at that time) to selective episiotomy use. The definition of routine varied from performing an episiotomy on all women to its use at the discretion of the attending obstetric personnel. Selective episiotomy was restricted mostly to cases of fetal distress and imminent perineal tear.
The largest of these trials, published by an Argentine Episiotomy Trial Collaborative Group in 1993, recruited 2606 women at first delivery [15]. The routine management group comprised 1298 women, with an 82.6% episiotomy rate. The remaining 1308 participants were the selective episiotomy group, in which the procedure was performed in 30.1% of cases. Severe perineal trauma was uncommon in both groups, slightly but nonsignificantly less frequent in the selective episiotomy group (1.2 vs 1.5%). Anterior perineal trauma was more common in the selective group, while posterior perineal surgical repair, perineal pain, healing complications, and dehiscence were all less frequent. In 2009, the Cochrane Collaboration meta-analysis was published, which examined the role of episiotomy in vaginal birth [7]. This review analyzed eight randomized controlled trials (including the abovementioned trial), encompassing 5541 women. In the routine episiotomy group, 75.2% of women underwent episiotomies versus 28.4% in the restrictive episiotomy group. Compared with routine use, restrictive episiotomy resulted in less severe perineal trauma (RR 0.67, 95% CI 0.49–0.91), less suturing (RR 0.71, 95% CI 0.61–0.81), and fewer healing complications (RR 0.69, 95% CI 0.56–0.85). Restrictive episiotomy was associated with more anterior perineal trauma (RR 1.84, 95% CI 1.61–2.10). There was no difference in dyspareunia, urinary incontinence, or several pain measures.
Following such evidence, rates of episiotomy have dramatically declined in most developed countries. Thus, the protocol of studies published several decades ago, comparing routine to selective episiotomy, might no longer be relevant. Regardless, since even limited practice of episiotomy might bear more complications than totally avoiding the procedure, new trials should focus on the comparison between these two practices. Several articles have been published in which the study group was defined as no episiotomy, similarly to our protocol [16,17,18]. However, those trials compared avoiding episiotomy to a group in which episiotomy was performed to all participants. We considered a such protocol quite unethical, since the majority of women obviously do not require episiotomy.
In light of the above, we sought to establish a trial thoroughly examining maternal and fetal complications between selective episiotomy practice and avoiding episiotomy. We found only one randomized controlled trial meeting these goals [19]. Published in 2017 by Amorim et al., the trial compared two groups: never perform episiotomy vs. selective episiotomy (i.e., in accordance with the healthcare professionals’ clinical judgment). Primary outcomes did not include advanced perineal tears but focused on numerous other variables, e.g., frequency of episiotomy, delivery duration, and frequency of spontaneous lacerations; 115 women were assigned to a nonepisiotomy protocol vs. 122 to selective episiotomy. There was no difference between groups with respect to maternal or perinatal outcomes, and episiotomy rate was similar (two in each group; ~ 1.7%). We therefore believed that a larger trial must be established focusing on advanced perineal tears as a primary outcome.
To our best knowledge, our study is the first randomized controlled trial comparing the effect of avoiding episiotomy on the rates of advanced perineal tears to selective episiotomy use, and no differences were found in advanced perineal tear rates between groups. However, no broad generalizations can be made based on our results, since the main limitation of our study—which in fact prompted us to publish the interim results—was that the rates of episiotomy in the nonepisiotomy group were almost similar to that in common practice. This was a surprising finding, since we performed several meetings with the destined investigators prior to trial commencement that included presentations of available evidence regarding episiotomy use, stressing that it has no definitely proven benefits and might even increase the complication rate. Therefore, a major concern was that episiotomy rates in the control group (the common practice) might decrease following these meetings, affecting the generalization of our conclusions. Thus, we were surprised to that not only did episiotomy rates not decline in the control group, inclusion of the participants in the nonepisiotomy group barely influenced the decision of obstetricians and midwives to perform episiotomy.
The phenomenon of noncompliance in episiotomy trials has been previously described [20]. During 1988–1990, a randomized controlled trial was conducted allocating pregnant women into two groups: try to avoid episiotomy (in which physicians were to use episiotomy only for fetal indications or anticipated severe tears) vs. control group (try to avoid a tear) [21]. Investigators noted that a third of physicians did not change their practice of using episiotomy, as required by the study protocol; instead, they used episiotomy ~ 90% of the time in both arms. Following these results, the authors developed a specific questionnaire for analyzing the original data according to the attending physicians’ beliefs about episiotomy [20]. This analysis demonstrated that physicians who viewed episiotomy more favorably more often diagnosed fetal distress in apparently normal labors and more often thought the perineum was unable to distend enough or was about to tear severely. The authors concluded that the noncompliant physicians were simply unable to change their behavior from their usual clinical practice, although they thought they would be able to.
Similar issues were noted in our trial, once again highlighting the difficulty of conducting trials designed to examine deviation from accepted practice. In view of better understanding the resistance to changing existing habits, we concluded that continuing investigator monitoring and education is crucial throughout the trial. Weekly reminders during staff meetings and periodic review and presentation of results concerning episiotomy use will be conducted to remind investigators of the importance of strict adherence to protocol.
Our study has several important qualities. It was meticulously planned according to the CONSORT guidelines following several discussions with an experienced epidemiologist. Significant fetal distress was chosen as a single criterion for deviation from protocol. During deliveries seriously endangering fetal well-being, any maneuver was allowed, even if unproven and potentially harmful to the mother. However, as fetal heart rate decelerations are much more frequent than monitor pointing at true fetal distress, we were concerned this statement would allow some accoucheurs to perform episiotomy sparingly and state that fetal distress was involved. Thus, we conditioned protocol deviation only at the discretion of the obstetrician in charge of the delivery and only in cases of unequivocal benefit to the fetus.
Our study assessed women planning their first vaginal delivery. This decision was based on the fact that both episiotomy and the frequency of advanced perineal tears are more frequent in such parturients than in multiparous women [22, 23] and the fact that recruiting both primiparous and multiparous women might compromise the quality of results, since by chance the ratio might significantly differ between groups, making conclusions less generalizable [18].
An additional finding of our trial was the unexpectedly high percentage of vacuum deliveries, allowing us to better analyze the outcomes of avoiding episiotomy in this specific group. Vacuum delivery has long constituted an indication for episiotomy [3]; however, a recent review reported that episiotomy in vacuum delivery does not appear to be of benefit and might even increase maternal morbidity [8]. In our trial, episiotomy was performed in 57.7% of the 26 cases in the standard care group vs. 39.4% of 33 cases in the avoidance of episiotomy group (or 13% of 23 per protocol cases). No statistically significant differences were found in any maternal or neonatal outcome between groups. However, two advanced perineal tears were diagnosed in the standard care group, with a 3.8% rate of intact perineum. No grade 3 or 4 tears were observed with avoidance of episiotomy, with a 12.1% rate of intact perineum (17.4% by per-protocol analysis). An increased rate of anterior spontaneous tears was noted in the no episiotomy group, in accordance with previous evidence [7]. Nevertheless, the overall rate of spontaneous tears and suturing characteristics did not differ between groups. Thus, we can assume that avoiding episiotomy is not related to an increased rate of adverse perinatal injuries and the trial can continue with the inclusion of vacuum deliveries. However, it is important to note that the study is not powered to detect group differences in vacuum delivery.
We cannot explain the shorter second stage in the no episiotomy group and assume it is an incidental finding. Lower rates of urinary retention 2 days after delivery in nonepisiotomy vacuum deliveries by per-protocol analysis can be explained by previous reports indicating episiotomy is a risk factor for urinary retention [24]. However, since this phenomenon was noted only in this limited subgroup analysis, this finding could also be incidental and must be examined in larger series.
Our trial has several important limitations, some of which related to the nature of data acquisition and analysis. Blinding of the investigators was not possible (of note, opening of the opaque sealed envelopes was performed only during the second stage of delivery in an effort to minimize the effect of the allocation method on the attitude of the attending caregiver). An additional drawback is the inclusion of two episiotomy types, lateral and mediolateral, the varying percentages of which could potentially affect outcomes; median episiotomy was not included, as it is not performed in our country. We could have restricted incisions to lateral or mediolateral only were concerned about noncompliance. Thus, we used the alternative control method of requesting a report on incision type and examining the proportions of lateral vs. mediolateral episiotomies between groups. Of note, no important differences in perineal outcomes were shown by the trials comparing lateral with mediolateral episiotomy [25, 26].
Rates of advanced perineal tears in the standard-care group were 3.87%, much higher than the 1.6% reported at the annual Israeli Maternal and Fetal Medicine Society meeting in November 2014. This finding can be explained by our inclusion of primiparous women only, i.e., participants with a risk factor for advanced tears [23]. In addition, underdiagnosis and underreporting of such tears was recognized long ago [27]. Strict evaluation of each case suspected of an advanced tear by a senior obstetrician and precise documentation of each case as part of the study protocol probably led to a more meticulous diagnosis and reporting of such tears.
Based on the updated 3.87% rate of advanced perineal tears, we calculated a sample size of 6006 patients to give 80% power with a two-sided type 1 error of 5% for detecting a 0.67% reduction in RR between groups [7]. At the current stage, additional centers are being recruited to participate in this multicenter trial.
In summary, despite its unproven benefits and possible harmful effects, episiotomy is still performed in one third of vaginal deliveries in primiparous women. Thus, we strongly believe that results of our trial might bear crucial implications to the existing practice. Monitoring and educating investigators should be continuously practiced throughout the trial duration, stressing the importance of adherence to protocol.
References
Seijmonsbergen-Schermers AE, Geerts CC, Prins M, van Diem MT, Klomp T, Lagro-Janssen AL, et al. The use of episiotomy in a low-risk population in the Netherlands: a secondary analysis. Birth. 2013;40(4):247–55.
Frass KA, Al-Harazi AH. Episiotomy is still performed routinely in Yemeni women. Saudi Med J. 2010;31(7):764–7.
Sagi-Dain L, Sagi S. Indications for episiotomy performance - a cross-sectional survey and review of the literature. J Obstet Gynaecol. 2016;36(3):361–5.
Driessen M, Bouvier-Colle MH, Dupont C, Khoshnood B, Rudigoz RC, Deneux-Tharaux C, et al. Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol. 2011;117(1):21–31.
Karacam Z, Ekmen H, Calisir H, Seker S. Prevalence of episiotomy in primiparas, related conditions, and effects of episiotomy on suture materials used, perineal pain, wound healing 3 weeks postpartum, in Turkey: a prospective follow-up study. Iranian J Nursing Midwifery Res. 2013;18(3):237–45.
Espuna-Pons M, Solans-Domenech M, Sanchez E. Pelvic floor research G. Double incontinence in a cohort of nulliparous pregnant women. Neurourol Urodyn. 2012;31(8):1236–41.
Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database of Syst Rev. 2009;1:CD000081.
Sagi-Dain L, Sagi S. Morbidity associated with episiotomy in vacuum delivery: a systematic review and meta-analysis. BJOG : Int J Obstet Gynaecol. 2015;122(8):1073–81.
Sagi-Dain L, Sagi S. The role of episiotomy in prevention and management of shoulder dystocia: a systematic review. Obstet Gynecol Surv. 2015;70(5):354–62.
Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG, Group C. Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA. 2012;308(24):2594–604.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ Prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):164–8. discussion 8
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13.
LaCross A, Groff M, Smaldone A. Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta-analysis. J Midwifery Womens Health. 2015;60(1):37–47.
Scheer I, Andrews V, Thakar R, Sultan AH. Urinary incontinence after obstetric anal sphincter injuries (OASIS)--is there a relationship? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(2):179–83.
Argentine Episiotomy Trial Collaborative Group. Routine vs selective episiotomy: a randomised controlled trial. Lancet. 1993;342(8886-8887):1517–8.
Islam A, Hanif A, Ehsan A, Arif S, Niazi SK, Niazi AK. Morbidity from episiotomy. JPMA J Pakistan Med Assoc. 2013;63(6):696–701.
Moini A, Yari RE, Eslami B. Episiotomy and third- and fourth-degree perineal tears in primiparous Iranian women. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2009;104(3):241–2.
Supadech KB C, Komolpis S, Panichkul S. Third and fourth degree Perineal lacerations of episiotomy versus nonepisiotomy in spontaneous vaginal deliveries at Phramongkutklao hospital. Thai J Obstet Gynaecol. 2008;16:199–20561. 167
Amorim MM, Coutinho IC, Melo I, Katz L. Selective episiotomy vs. implementation of a nonepisiotomy protocol: a randomized clinical trial. Reprod Health. 2017;14(1):55.
Klein MC, Kaczorowski J, Robbins JM, Gauthier RJ, Jorgensen SH, Joshi AK. Physicians' Beliefs and behaviour during a randomized controlled trial of episiotomy: consequences for women in their care. CMAJ : Canadian Med Assoc J = Journal de l'Association Medicale Canadienne. 1995;153(6):769–79.
Klein MC, Gauthier RJ, Jorgensen SH, Robbins JM, Kaczorowski J, Johnson B, et al. Does episiotomy prevent perineal trauma and pelvic floor relaxation? The Online journal of current clinical trials. 1992;Doc No 10:[6019 words; 65 paragraphs].
Raisanen S, Vehvilainen-Julkunen K, Heinonen S. Need for and consequences of episiotomy in vaginal birth: a critical approach. Midwifery. 2010;26(3):348–56.
Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth. 2013;13:59.
Mulder FE, Schoffelmeer MA, Hakvoort RA, Limpens J, Mol BW, van der Post JA, et al. Risk factors for postpartum urinary retention: a systematic review and meta-analysis. BJOG : Int J Obstet Gynaecol. 2012;119(12):1440–6.
Karbanova J, Rusavy Z, Betincova L, Jansova M, Parizek A, Kalis V. Clinical evaluation of peripartum outcomes of mediolateral versus lateral episiotomy. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2014;124(1):72–6.
Sagi-Dain L, Sagi S. The correct episiotomy: does it exist? A cross-sectional survey of four public Israeli hospitals and review of the literature. Int Urogynecol J. 2015;26(8):1213–9.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries--myth or reality? BJOG : Int J Obstet Gynaecol. 2006;113(2):195–200.
Acknowledgements
We are grateful to all participating patients, obstetricians, and midwives who made this research possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer/conflict of interests
None (for all authors).
Electronic supplementary material
Supplementary Table 1
(DOC 47 kb)
Supplementary Table 2
(DOC 31 kb)
Supplementary Table 3
(DOC 39 kb)
Supplementary Table 4
(DOC 64 kb)
Rights and permissions
About this article
Cite this article
Sagi-Dain, L., Bahous, R., Caspin, O. et al. No episiotomy versus selective lateral/mediolateral episiotomy (EPITRIAL): an interim analysis. Int Urogynecol J 29, 415–423 (2018). https://doi.org/10.1007/s00192-017-3480-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3480-7