Abstract
Purpose
Intrahepatic cholestasis of pregnancy and preeclampsia are two major pregnancy complications. We aimed to investigate the association between intrahepatic cholestasis of pregnancy (ICP) and preeclampsia.
Methods
Single-center retrospective study. Study group included 180 women (162 singletons and 18 twin gestations) who were diagnosed with ICP based on clinical presentation, elevated liver enzymes and bile acids. The reference group included 1618 women (1507 singletons and 111 twin gestations) who delivered during the study period, and were matched according to age, gravidity, parity and singleton or twin gestation.
Results
The incidence of ICP was 0.36%. The incidence of preeclampsia was higher in women with ICP compared to reference group (7.78% vs 2.41%, aOR, 3.74 95% CI 12.0–7.02, p < 0.0001), for either without—(3.89% vs 1.61%, aOR 2.83, 95% CI 1.23–6.5, p = 0.145) or with severe features (3.89% vs 0.80%, aOR 5.17 95% CI 2.14–12.50, p = 0.0003). For both singleton and twin pregnancies, overall preeclampsia rates were higher in the ICP group (5.56% vs 2.19%, aOR 2.91 95% CI 1.39–6.07 p = 0.0045; and 27.78% vs 5.41%, aOR 10.9 95% CI 2.16–47.19, p = 0.0033, respectively). Earlier diagnosis of ICP was associated with higher incidence of preeclampsia (31.1 ± 3.8 vs 34.86 ± 6.2 gestational weeks, p = 0.0259). The average time between ICP diagnosis and to the onset of preeclampsia was 29.7 ± 24 days.
Conclusion
ICP is associated with an increased risk for preeclampsia. We suggest intensified follow-up for preeclampsia in women with ICP, especially among those with early ICP presentation and twins’ gestations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrahepatic cholestasis of pregnancy (ICP) typically presents in the third trimester of pregnancy as pruritus, elevated liver enzymes and increased bile acids. The reported incidence varies between 0.3–5.6% in the Unites States, and 0.5–1.5% in Europe [1, 2].
The exact pathogenesis is unclear, although genetic, hormonal, immunological and environmental factors are assumed to be implicated [3,4,5,6]. High estrogen levels for example, which characterize the third trimester, as well as multiple gestations, were found to be associated with ICP [7]. The maternal prognosis is favorable, nevertheless the disease harbors increased fetal risk for preterm delivery, meconium-stained amniotic fluid and stillbirth [8, 9].
The association between ICP and preeclampsia was evaluated in several case reports [10, 11], retrospective cohorts [12,13,14] and a population-based cohort [15], some of which found positive association between the two conditions, however, robust data stills lacks, and clinically beneficial risk assessment and its timeframe are scarce. Moreover, preeclampsia is a heterogeneous disease, in severity (with or without severe features, HELLP syndrome and eclampsia), timing of appearance (early or late onset, at a cutoff of 34 gestational weeks) and associated maternal (single or multiple organs involvement) and fetal complications (with or without growth restriction). ICP is predominantly associated with milder and later preeclampsia, without growth restriction, as earlier preeclampsia, is not usually preceded by ICP.
The aim of this study was to evaluate whether ICP is associated with a higher risk to develop preeclampsia, and its exact subtypes, and if so, to evaluate that risk.
Materials and methods
We conducted a historical cohort study. Women diagnosed with ICP were compared to matched references without ICP. The rate of preeclampsia, as well as obstetrical outcomes, was compared between groups.
Study population
All women hospitalized between July 2012 and December 2017 in Rabin Medical Center (Petach-Tikva, Israel) with a diagnosis of ICP were included in the study group. We excluded women without a definitive diagnosis of ICP, missing information on pregnancy outcome, high order gestation (triplets and above) and women with preeclampsia onset preceding the diagnosis of ICP.
From the same database and time period, matched by maternal characteristics including age, gravidity, parity and singleton or twin gestation, women without ICP were allocated, if available, in a 10:1 ratio. Uncommon study group patient’s characteristics, such as extreme maternal age, were matched with less references; however, the minimal references for each ICP patient were two.
Data collection
Demographic, clinical, obstetrical and laboratory data were collected from computerized medical records and the hospital’s laboratory database. Collected data for each participant included maternal age, gravidity, parity, height, weight, previous cesarean deliveries, abortions, living children, mode of conception, comorbidities including pre- or gestational diabetes mellitus, chronic hypertension, inherited thrombophilia, systemic lupus erythematosus, anti-phospholipid syndrome and any other renal, liver or cardiac disease.
Clinical and laboratory parameters that were collected included blood pressure, platelet count, liver enzymes, urinary protein and total bile acids (DZ042A-K; Diazyme Lab, Poway, CA analyzed with an ADVIA 2400 Clinical Chemistry System, Siemens Healthcare, Erlangen, Germany); as well as the diagnoses of ICP and preeclampsia. Clinical and laboratory data was collected at time of hospital admission—for the study group, this was at their first attendance with ICP symptoms; for the reference group, this was at their first admission for any indication during the third trimester, or their admission for delivery in the absence of earlier admissions.
Obstetrical and neonatal data included mode of delivery and indication for cesarean delivery if performed, date and time of birth, gender, birthweight and birthweight percentile—which was calculated according to nationally accepted growth curves per gestational week and gender [16], presence of meconium-stained amniotic fluid, Apgar score at 1 and 5 min, arterial umbilical cord pH, neonatal intensive care (NICU) admission and perinatal mortality.
Definitions
Diagnosis of ICP was based on clinical presentation of typical pruritus involving palms and feet, accompanied by either elevated liver enzymes and/or elevated bile acid levels (> 10 µmol/L) in the absence of other possible etiologies [17].
Proteinuria was defined as either ≥ 300 mg/24 h urinary protein or ≥ 30 mg/dL in random urine sample. Preeclampsia was defined as blood pressure values of ≥ 140/90 mmHg accompanied by proteinuria, defined as above, initially diagnosed after 20 gestational weeks. Preeclampsia with severe features was defined as preeclampsia accompanied by one of the followings: headache, blurred vision or unexplained right upper quadrant epigastric pain, blood pressure ≥ 160/110 platelet count < 100,000 cells/µL, hepatic transaminase levels twice the upper normal, creatinine > 1.1 or twofold increase from baseline levels, pulmonary edema, or HELLP syndrome even in the absence of hypertension [18].
Our common practice, in line with accepted guidelines, is to induce labor at 37 gestational weeks if ICP was diagnosed before term, or at the time of diagnosis in term gestations. If labor was not immediately induced, women are treated with Ursodeoxycholic acid (UDCA) 600–1800 mg per day. Women are monitored, for a 24–72 h inpatient evaluation and later followed in an outpatient setting, according to clinical discretion, for disease manifestations and fetal wellbeing. During the study period, the follow-up protocol for women with ICP included weekly or bi-weekly NSTs, accompanied with blood pressure measurements, proteinuria assessment and laboratory examinations; as well as fetal weight estimations with Doppler added as necessary if growth restriction was suspected. Women with diagnosis of ICP and subsequently preeclampsia were managed according to accepted guidelines for preeclampsia, with delivery at diagnosis or up to 37 gestational weeks, according to severity. If blood pressure was repeatedly measured above 160/100, antihypertensive treatment was initiated with either hydralazine of labetalol, according the physician’s discretion.
Three types of cesarean deliveries were defined: elective cesarean delivery was defined if it was chosen for maternal or neonatal indications, without evidence for compromise of either one of them. If signs of maternal or fetal compromise were present, non-elective cesarean delivery was defined. If the decision to perform cesarean delivery was taken during active labor, we defined the cesarean delivery as intra-partum.
Inherited thrombophilia was defined if a woman was diagnosed with either homozygous or heterozygous mutation of any of the following: Factor V Leiden, Anti-thrombin III deficiency, Protein C deficiency, Protein S deficiency, prothrombin G20210A mutation.
Small for gestational age (SGA) newborn was defined as birthweight below the 10th percentile. Preterm delivery was defined as delivery < 37 gestational weeks.
Outcome measures
Primary outcome was defined as the development of preeclampsia and its severity, either with or without severe features and eclampsia. Secondary outcomes were gestational age at birth, mode of delivery, type of cesarean delivery (either elective, non-elective or intra-partum), presence of meconium-stained amniotic fluid, birthweight and birthweight percentile, SGA, 5-min Apgar score, umbilical artery cord pH, NICU admission and intrauterine fetal death.
Statistical analysis
Statistical analysis was performed using the SAS software (SAS Cooperation, Version 34.0, North Carolina, USA). Continuous variables were presented as mean and standard deviation, whereas categorical variables as count and percentages. Univariate analysis was used to determine the relationship between each explanatory variable and preeclampsia occurrence in both study and reference groups. Pearson χ2 test or Fisher exact, as appropriate, were used to compare between the study and reference groups with respect to categorical variables. Independent samples t test was used to compare the means of the two groups for continuous variables. ICP as an independent risk factor for preeclampsia was evaluated in a multivariate logistic regression analysis with the following confounders taken into account: maternal age, body mass index, parity, anti-phospholipid syndrome, inherited thrombophilia and chronic hypertension. All p values were determined with two-tailed tests. A probability value of < 0.05 was considered statistically significant.
Ethics
The study was approved by the local institutional review board (Approval no. RMC-314–17). Informed consent was waived due to the retrospective design of the study, as it included only data of human participant without intervention.
Results
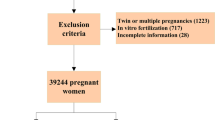
Out of a total of 49,406 deliveries in our medical center during the study period, 210 women with ICP were identified. Seventeen women were excluded, because ICP was suspected, but in retrospective case review, clinical presentation or laboratory results did not match the diagnosis. Ten women delivered outside of our medical center and were excluded due to missing delivery outcomes. One woman was excluded because of triplet gestation. Two women were excluded, because the diagnosis of preeclampsia preceded the diagnosis of ICP. Accordingly, 180 women were included in the study group—162 with singleton and 18 with twin gestation, as well as 1,618 women in the reference group—1507 with singleton and 111 with twin gestation. The incidence of ICP in our study population was 0.36%.
Demographics
Baseline obstetrical and demographic characteristics were similar between study and reference groups, except a slightly higher rate of previous cesarean deliveries in the reference group (0.3 ± 0.6 vs 0.2 ± 0.4, p = 0.002) (Table 1). Clinical and laboratory parameters from the time of first admission are presented in Table 2. Proteinuria rates, blood pressure and platelet count did not differ between the groups. Liver enzymes levels were markedly higher in the ICP group (aspartate aminotransferase 30.2 ± 31.7 vs 15.1 ± 16.5 IU/L, p < 0.0001; alanine transaminase 109.4 ± 135.1 vs 22.8 ± 50.5 IU/L, p < 0.0001).
Primary outcome
Overall rates of preeclampsia (7.78% vs 2.41%, p < 0.0001), either without severe features (3.89% vs 1.61%, p = 0.0238) or with severe features (3.89% vs 0.80%, p = 0.0004) were all significantly higher in the ICP group compared to the reference group, as was the rate of HELLP syndrome (1.69% vs 0.12%, p = 0.0082).
For both singleton and twin pregnancies, overall preeclampsia rates were higher in the ICP group (5.56% vs 2.19%, p = 0.0081; 27.78% vs 5.41%, p = 0.0042, respectively). However, in sub-analysis for subtype of preeclampsia according to severity, significantly higher rates were found only for mild preeclampsia in singletons and for severe preeclampsia in twin gestations (3.70% vs 1.46%, p = 0.0264; 22.22% vs 1.80%, p = 0.0021). Multivariate logistic regression analysis did not change level of significance any of the differences mentioned above (Table 3).
In another sub-analysis for preeclampsia timing, both early-onset preeclampsia, prior to 34 week gestation (2.22% vs 0.25%, p = 0.042) and late-onset preeclampsia (5.56% vs. 0.99%, p = 0.0001) were more prevalent in the study compared to the control group, although absolutely more women had late-onset preeclampsia.
The prevalence of the various preeclampsia subtypes—overall, severe, mild, HELLP syndrome, early- and late-Onset—in the study and control groups, are presented in Fig. 1.
Average time between ICP diagnoses to onset of preeclampsia was 29.7 ± 24 days.
Secondary outcomes
Other obstetrical and neonatal outcomes are presented in Table 4. Women in the study group delivered earlier (37.38 ± 1.3 vs 37.65 ± 1.2, p = 0.0048(, and preeclampsia ensued earlier (35.30 ± 2.5 vs. 35.9 ± 2.9, p = 0.007) but the difference for both was not clinically important. The preterm birth rate before 37 weeks did not differ between the groups; however, preterm birth rates before 34 weeks were significantly higher in the ICP group (2.78% vs 0.80%, p = 0.0276), but not when analyzed according to twin (1.67% vs. 0.37%, p = 0.0527) or singleton (1.11% vs. 0.43%, p = 0.2254) gestations.
There was no difference in the mode of delivery between the groups; however, in the ICP group, cesarean deliveries were less often performed electively and more were performed intra-partum (26.8%, 10.7% and 62.5% in ICP group, vs 50.9%, 8.4% and 40.1% in the reference group for elective, non-elective and intra-partum cesarean deliveries, respectively, p = 0.0024). Overall birthweight was significantly higher in the ICP group by birthweight percentiles (59.1 ± 23.2 vs 53.2 ± 23.6, p = 0.0028) but not in absolute terms (2914 ± 506 g vs 2894 ± 5050 g, p = 0.589). For singletons, it was significantly higher both absolutely and by percentiles, (3072 ± 370 g vs 2981 ± 459 g, p = 0.015; 60.7 ± 22.0 vs 53.0 ± 26.8, p = 0.0004). For twins, birthweight did not differ by either deviation (2207 ± 421 vs 2309 ± 401 g, p = 0.165; 51.9 ± 26.9 vs 54.2 ± 26.1, p = 0.62; for ICP and reference groups, respectively). SGA rate was higher in the reference group compared to the ICP group in the overall study population (6.82% vs 2.02%, p = 0.0052), among singletons (6.97% vs 1.85%, p = 0.007) but not for twins. Among singletons and twins the rates of SGA did not differ for those with vs. without preeclampsia (7.14% vs. 6.45%, p = 0.7501 and 4.76% vs. 5.44%, p = 1.000).
Women in the ICP group had higher rates of meconium-stained amniotic fluid, compared to women in the reference group (7.78% vs 3.89, p < 0.0001). There was no difference in the intrauterine fetal deaths rate between ICP and reference groups.
We further analyzed our population according to presence or absence of preeclampsia (Table 5). Women who eventually developed preeclampsia were diagnosed with ICP earlier at pregnancy (31.1 ± 3.8 vs 34.86 ± 6.2 gestational weeks, p = 0.0259). Bile acids level, liver enzymes and platelet count at first admission did not differ between patients who developed preeclampsia during pregnancy to those who did not.
Discussion
This was a retrospective analysis to examine the association between ICP and subsequent preeclampsia. Our main findings demonstrated (1) higher rate of preeclampsia in women who experienced ICP, both for singleton and twin gestations; (2) women who were diagnosed with ICP earlier in pregnancy had higher risk for developing preeclampsia.
The incidence of ICP in our population, 0.36%, is similar to reported rate among non-Latina in the USA [1], and close to the reported rate of ICP in a prior Israeli cohort, of 0.1% [12].
Our study is in line with previous reports, suggesting an association between ICP and preeclampsia [10,11,12,13,14,15]. Atabey et al. [10] reported of a woman who was diagnosed with ICP in the 29th gestational week, complicated with preeclampsia, followed by eclampsia, 7 weeks later. In another small case series of eight consecutive women with ICP, 25% were complicated with preeclampsia [11]. In a study of 99 women with ICP, who were diagnosed based on pruritus and elevated liver enzymes, in the absence of bile acid test availability, a three-time increased incidence of preeclampsia was found [13].
Raz et al. [12] retrospectively studied 54 singleton and 24 twin pregnancies with ICP, reporting higher incidence of preeclampsia compared to references without ICP (7.4% vs 1.5% for singletons, p < 0.05; 33.3% vs 6.2% for twins, p < 0.05). In their study, preeclampsia usually presented 2–4 weeks after the diagnosis of ICP; however, unlike our study, they were unable to demonstrate that women who presented with ICP earlier in pregnancy had higher incidence of preeclampsia. In contrast to their findings, we failed to establish a dose-dependent relationship between bile acid levels to the risk of preeclampsia. Another supporting evidence for this association is that higher median bile acid level was demonstrated among women diagnosed with preeclampsia, compared to references, 8% of which had markedly elevated bile acid levels, although none reported pruritus [19]. A population-based cohort with over 1.2 M singleton deliveries similarly detected 2.6 higher rate of preeclampsia among women who experienced ICP, compared to those who did not [10]. Marathe et al. demonstrated among 320 women diagnosed with ICP a 75-fold risk for preeclampsia compared to the general population [14].
Interestingly, higher rates of gestational diabetes mellitus were also noted among the ICP subgroup [15, 20], an association we did not detect. Of note, women in the ICP group were generally older and with higher rates of hypertension, all of which may account for the higher prevalence of GDM in Shemer et al. cohort [15].
We found that study group newborns were heavier, with lower rate of SGA even those diagnosed with preeclampsia. Similarly, Shemer et al. [15] demonstrated lower rates of SGA and higher rates of Large-for-gestational age in women with ICP, even after excluding gestational diabetes. Geenes et al. [21] found lower birthweight, associated with earlier delivery among ICP patients, while birthweight centiles were significantly higher and SGA rate lower.
Overall, this supports the fact that ICP is a risk factor mainly for late-onset preeclampsia, and not for early-onset preeclampsia and associated growth restriction.
There are several possible explanations for the demonstrated association between ICP and preeclampsia.
Firstly, ICP preeclampsia share similar risk factors, such as maternal age and multiple gestation, so specific maternal population may be at high risk for both conditions. Secondly, high bile acid levels were shown to induce vasoconstriction [22]. Increased capillary growth in terminal villi is a pathologic condition resulting from long-standing placental hypoperfusion or low-grade tissue hypoxemia [23]. Shemer et al. [24] found increased placental capillary growth and suggested it to be a response to low-grade hypoxia induced by increased maternal bile acid levels. This idea was further demonstrated by their finding of increased number of syncytial knots in ICP placentas, as was similarly reported for placentas of women with preeclampsia [25].
Molecular mechanisms may also link the pathogenesis of these conditions. A Disintegrin-like Metalloproteinase with ThromboSpondin motifs (ADAMTSs) are a secreted metalloproteinase family consisting on 19 members in humans, some of which have a role in implantation and placentation. Specifically, ADAMTS-12 levels were shown to be lower in patients with either ICP or preeclampsia. In addition, placental arylesterase, which balances oxidant and antioxidant activity, was significantly lower in both ICP and preeclampsia groups compared to references [26].
Changes in the expression of immunologic factors such as dendritic cells T17 and Treg, as well as pro-inflammatory factors IL-17 and IL-35 have all been associated with both preeclampsia and ICP [4,5,6]. As bile acids were found to cause changes in the immune system from a TH2-mediated response to TH1, they might have a main role in the pathologic ICP to preeclampsia course [3].
Genetic association may also have a role, with possible genetic linkage between chromosome region 2p13-p12, preeclampsia and obstetric cholestasis [27]. In addition, genetic transporter mutations, such as alterations in ABCB4, and ATP8B1 genes, were found to be involved in the pathogenesis of the familial forms of ICP (progressive familial intrahepatic cholestasis—PFIC; and benign recurrent intrahepatic cholestasis—BRIC). Other transporter gene mutations, like ABCB11, increase the susceptibility to ICP [3].
Strengths and limitations
The strengths of our study lie in it being a single-center study, with uniform clinical and laboratory evaluation approach, as well as management protocol. In addition, to the best of our knowledge, this is the largest non-population-based study demonstrating this important association. Our study is not without limitation, foremost, due to its retrospective design, with limited data available for some parameters, such as ethnicity and Doppler studies.
Conclusion
Our findings suggest an association between ICP and preeclampsia. This has clinical implications, which obligate close follow-up and surveillance for preeclampsia in women with ICP, especially among high-risk women who develop ICP early during pregnancy or with twins’ gestations. The exact and effective follow-up will have to be determined in future studies. Currently, we can at least recommend that heightened follow-up, according to local protocols should be adopted for women with ICP similar to any other at-risk subgroup, with a minimum of blood pressure and proteinuria surveillance.
References
Laifer SA, Stiller RJ, Siddiqui DS, Dunston-Boone G, Whetham JC (2001) Ursodeoxycholic acid for the treatment of intrahepatic cholestasis of pregnancy. J Matern Fetal Med 10(2):131–135
Lee RH, Goodwin TM, Greenspoon J, Incerpi M (2006) The prevalence of intrahepatic cholestasis of pregnancy in a primarily Latina Los Angeles population. J Perinatol 26(9):527–532
Larson SP, Kovilam O, Agrawal DK (2016) Immunological basis in the pathogenesis of intrahepatic cholestasis of pregnancy. Expert Rev Clin Immunol 12(1):39–48
Kong X, Kong Y, Zhang F, Wang T, Zhu X (2018) Expression and significance of dendritic cells and Th17/Treg in serum and placental tissues of patients with intrahepatic cholestasis of pregnancy. J Matern Neonatal Med 31:901–906
Yang X, Zhang J, Ding Y (2017) Association of microRNA-155, interleukin 17A, and proteinuria in preeclampsia. Medicine (United States) 96:1–8
Cao W, Wang X, Chen T, Xu W, Feng F, Zhao S, Wang Z, Hu Y, Xie B (2018) Maternal lipids, BMI and IL-17/IL-35 imbalance in concurrent gestational diabetes mellitus and preeclampsia. Exp Ther Med 16:427–435
Dixon PH, Williamson C (2016) The pathophysiology of intrahepatic cholestasis of pregnancy. Clin Res Hepatol Gastroenterol 40(2):141–153
Gonzalez MC, Reyes H, Arrese M, Figueroa D, Lorca B, Andresen M, Segovia N, Molina C, Arce S (1989) Intrahepatic cholestasis of pregnancy in twin pregnancies. J Hepatol 9(1):84–90
Geenes V, Williamson C (2009) Intrahepatic cholestasis of pregnancy. World J Gastroenterol 15(17):2049–2066
Atabey S, Duvan CI, Eren U, Turhan NO (2007) Intrahepatic cholestasis and eclampsia: a case report. Hypertens Pregnancy 26(4):363–369
Lo TK, Lau WL, Lam HS, Leung WC, Chin RK (2007) Obstetric cholestasis in Hong Kong—local experience with eight consecutive cases. Hong Kong Med J 13(5):387–391
Raz Y, Lavie A, Vered Y, Goldiner I, Skornick-Rapaport A, Landsberg Asher Y, Maslovitz S, Levin I, Lessing JB, Kuperminc MJ, Rimon E (2015) Severe intrahepatic cholestasis of pregnancy is a risk factor for preeclampsia in singleton and twin pregnancies. Am J Obstet Gynecol 213(3):395.e1–8
Baliutavičienė D, Zubruvienė N, Zalinkevičius R (2011) Pregnancy outcome in cases of intrahepatic cholestasis of pregnancy. Int J Gynaecol Obstet 112(3):250–251
Marathe JA, Lim WH, Metz MP, Scheil W, Dekker GA, Hague WM (2017) A retrospective cohort review of intrahepatic cholestasis of pregnancy in a South Australian population. Eur J Obstet Gynecol Reprod Biol 218:33–38
Shemer WE, Marschall HU, Ludvigsson JF, Stephansson O (2013) Intrahepatic cholestasis of pregnancy and associated adverse pregnancy and fetal outcomes: a 12-year population-based cohort study. BJOG 120(6):717–723
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES (2005) Birth weight standards in the live-born population in Israel. Isr Med Assoc J 7(5):311–314
Royal College of Obstetricians and Gynaecologists (2011) Obstetric Cholestasis Green-top Guideline No. 43. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_43.pdf. Accessed 22 Dec 2019
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy (2013) Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on hypertension in pregnancy. Obstet Gynecol 122(5):1122–1131
Goulis DG, Walker IA, de Swiet M, Redman CW, Williamson C (2004) Preeclampsia with abnormal liver function tests is associated with cholestasis in a subgroup of cases. Hypertens Pregnancy 23(1):19–27
Martineau M, Raker C, Powrie R, Williamson C (2014) Intrahepatic cholestasis of pregnancy is associated with an increased risk of gestational diabetes. Eur J Obstet Gynecol Reprod Biol 176:80–85
Geenes V, Chappell LC, Seed PT, Steer PJ, Knight M, Williamson C (2014) Association of severe intrahepatic cholestasis of pregnancy with adverse pregnancy outcomes: a prospective population-based case-control study. Hepatology 59(4):1482–1491
Sepúlveda WH, González C, Cruz MA, Rudolph MI (1991) Vasoconstrictive effect of bile acids on isolated human placental chorionic veins. Eur J Obstet Gynecol Reprod Biol 42(3):211–215
van Patot MC, Valdez M, Becky V, Cindrova-Davies T, Johns J, Zwerdling L, Jauniaux E, Burton GJ (2009) Impact of pregnancy at high altitude on placental morphology in non-native women with and without preeclampsia. Placenta 30(6):523–528
Shemer WE, Thorsell M, Östlund E, Blomgren B, Marschall HU (2012) Stereological assessment of placental morphology in intrahepatic cholestasis of pregnancy. Placenta 33(11):914–918
Heazell AE, Moll SJ, Jones CJ, Baker PN, Crocker IP (2007) Formation of syncytial knots is increased by hyperoxia, hypoxia and reactive oxygen species. Placenta 28(Suppl A):S33–S40
Oztas E, Ozler S, Ersoy AO, Erkenekli K, Sucak A, Ergin M, Uygur D, Danisman N (2016) Placental ADAMTS-12 levels in the pathogenesis of preeclampsia and intrahepatic cholestasis of pregnancy. Reprod Sci 23(4):475–481
Laasanen J, Hiltunen M, Romppanen EL, Punnonen K, Mannermaa A, Heinonen S (2003) Microsatellite marker association at chromosome region 2p13 in Finnish patients with preeclampsia and obstetric cholestasis suggests a common risk locus. Eur J Hum Genet 11(3):232–236
Funding
None received.
Author information
Authors and Affiliations
Contributions
MM: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. AS: data collection or management, data analysis, and manuscript writing/editing. EK: data collection or management, data analysis, and manuscript writing/editing. RB: data collection or management, data analysis, and manuscript writing/editing. OS-A: data collection or management, data analysis, and manuscript writing/editing. MB: protocol/project development, data analysis, and manuscript writing/editing. NA: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. EH: protocol/project development, data analysis, and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mor, M., Shmueli, A., Krispin, E. et al. Intrahepatic cholestasis of pregnancy as a risk factor for preeclampsia. Arch Gynecol Obstet 301, 655–664 (2020). https://doi.org/10.1007/s00404-020-05456-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05456-y