Abstract
Purpose
The aim of this study is to evaluate the sperm DNA fragmentation index (DFI) in oocyte donation cycles and correlate it with the sperm parameters, the male characteristics, the embryo quality and the outcome of intracytoplasmic sperm injection (ICSI).
Methods
A total of 150 couples participating in an oocyte donation program were included in the study. Sperm samples were assessed by conventional sperm analysis. DFI was evaluated using the Halosperm kit, a sperm chromatin dispersion test (SCD).
Results
The relations between DNA damage and epidemiological male factors (age, height, weight), standard semen parameters (concentration, total and forward motility, and morphology), and embryological and clinical parameters (fertilization rate, total blastocyst number, number of good quality blastocyst, clinical pregnancy) were analyzed. DFI was positively correlated with advanced male age (r = 0.23, p < 0.05) and negatively correlated with total sperm and forward motility (r = − 0.29, r = − 0.27, respectively; p < 0.05). DFI was not significantly correlated with pregnancy outcome in oocyte donation cycles (r = − 0.05, p > 0.05). When good quality blastocysts were chosen, a trend toward the development of good quality embryos was detected in the presence of a low DFI (r = − 0.20, p = 0.08).
Conclusions
DFI does not significantly affect the outcome of ICSI in oocyte donation cycles. Even in cases of advanced paternal age that a high DFI resulted sperm DNA fragmentation seems not to adversely affect the final outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, many studies have focused on the role of sperm nuclear-DNA integrity in male factor infertility [1]. Sperm DNA integrity is essential for accurate transmission of genetic information, and it could be affected by apoptosis, reactive oxygen species (ROS), ionizing radiation and abnormalities in chromatin packaging [2]. Conflicting data exist about the impact of paternal DNA damage on embryo quality and the rates of fertilization and pregnancy [3, 4]. Additionally, reports of an adverse effect of oxidative stress on the intracytoplasmic sperm injection (ICSI) procedure have been inconsistent [5]. Sperm freezing methods do not seem to compromise sperm DNA integrity. Although ultrastructural data have shown that cryopreservation increases the rate of nuclear vacuole formation in the motile sperm head [6] and cytoplasmic vacuolization in oocytes of stimulated cycles [7, 8], sperm DNA integrity depends on the cryoprotectants used in the medium [9]. It has been reported that spermatozoa with damaged DNA did not lose their fertilization capacity [5].
A variety of tests dedicated to the measurement of sperm DNA fragmentation (SDF test) has been developed over the last few years. The terminal deoxynucleotidyl transferases (TdT) dUTP nick-end labeling (TUNEL assay), the single cell gel electrophoresis assay (COMET assay), the DNA breakage detection-fluorescence in situ hybridization (DBD-FISH) technique, and the sperm chromatin structure assay (SCSA) [10] are examples of those that have been used as indicators of sperm DNA breaks. The sperm chromatin dispersion (SCD) technique is a sensitive assay (more sensitive than the SCSA procedure, considered the gold standard SDF analysis [11]), highly reproducible, and directly linked with sperm DNA fragmentation as it is related to induction of DNA decondensation [12]. The SCD test is based on the principle that spermatozoa with fragmented DNA fail to produce the characteristic halo of dispersed DNA loops that is observed in sperm without fragmented DNA following acid denaturation and removal of nuclear proteins [10]. The SCD test, unlike to other semiquantitative assays mentioned above, does not rely on either color or fluorescence intensity. Rather, the endpoint measured by the SCD test consists of determining the percentage of spermatozoa with non-dispersed or dispersed nuclei, which can be easily and reliably accomplished by the naked eye [13]. However, none of the current SDF tests has shown difference in predictive value between in vitro fertilization (IVF) and ICSI procedures or high capacity to predict a positive clinical outcome in context of medically assisted reproduction [14]. In addition, the measurements at the percentage of sperm DNA fragmentation index (DFI) do not contribute to alter patient diagnosis, therapy and/or prognosis [15]. Regarding ICSI, a sensitivity analysis showed no statistically significant difference in live birth rate between low and high DFI [16]. Until now, limited data exists to back that infertility in men affects the DNA integrity of semen samples, specifically whether any effects are clinically significant, relevant, or reproducible [17]. Therefore, the accuracy of these tests to predict IVF or ICSI outcomes is controversial and their routinely clinical use is not recommended [18].
A good quality oocyte can repair sperm DNA damage, and the DNA repair system depends on the oocyte's cytoplasmic and genomic quality [2, 19]. Consequently, paternally transmitted DNA aberrations of the embryo could possibly be avoided when the oocyte quality is high, as in young patients and oocyte donation cycles in which fertilized eggs originate from healthy women. In addition, it is well known that endogenous and exogenous DNA damage occurs once the oocyte is fertilized, while the fully functional DNA repair system of the oocyte may be capable of rectifying persisting unrepaired damage in both the maternal and paternal genome [20]. In this respect, in cases of female infertility due to age, with multiple pregnancy failures after repeated assisted reproductive treatment, and the absence of severe male infertility factors, an oocyte donation program could be a means to increase the rates of successful implantation and pregnancy by decreasing the risk of pregnancy loss and offspring with genetic defects of paternal origin [21]. Previous studies with oocyte donation cases have reported the effect of sperm DNA fragmentation on human gametes and embryo quality as well as on optimization of clinical outcomes [22, 23]. However, clinical reports in terms of DFI evaluation by SCD test in cases with donated oocytes and ICSI treatment are still limited.
This study aims to evaluate the impact of the sperm DNA fragmentation, as measured by the SCD test, on the outcome of ICSI in relation to sperm parameters, male epidemiological characteristics, and clinical outcomes in couples who used donor oocytes due to female infertility when their male partners were proven fertile.
Materials and methods
Study design
A prospective, observational, cohort study was performed between November 2013 and October 2014 at IAKENTRO Fertility Centre in Thessaloniki, Greece. The study was approved by the Institutional Review Board of IAKENTRO advanced medical center/ethics committee, in Thessaloniki at 2/9/2013, ref.number 9/2013, and informed consent was obtained from all patients. An initial number of 162 cases were selected for this study, of which 12 cases were excluded due to the exclusion criteria of oocyte donors (n = 7) or incomplete data of DFI measurements performed in the selected sperm samples (n = 5). Afterwards, one hundred fifty (n = 150) oocyte donors participated in our study. A single stimulation cycle was included for each donor. A detailed medical history of each donor was taken. The oocyte donors were ≤ 32 years old, had body mass indices < 30 kg/m2, regular menstrual cycles of 25–35 days, two normal ovaries based on transvaginal scan findings, no polycystic ovarian syndrome, no known endometriosis, no gynecological or medical disorders and agreed to donate their oocytes for treatment anonymously and altruistically. Oocyte donors were of known fertility and good ovarian response. A blood sample was collected for karyotyping and screening for previous viral infections (hepatitis B and C, human immunodeficiency virus, and syphilis) thalassemia, and cystic fibrosis. A single ovarian stimulation cycle attempt was performed for each donor. A representative image of donor retrieved oocyte is shown in Fig. 1a. Our study included patients with a minimum of eight mature oocytes, which is a basic requirement offered to recipient couples in our donation program. Consequently, after the retrieved oocytes were denuded, if a recipient ended up with ≤ 7 mature oocytes, these cycles were excluded from our analysis (n = 7).
A total of 150 recipients, matched with their donors (n = 150), were included in the study. All recipients were < 50 years old without history of endometriosis and this was their first oocyte donation cycle. The recipients and their partners underwent blood screening similar to the donors, while a hysterosalpingogram and a diagnostic hysteroscopy eliminated cases presenting hydrosalpinx or intrauterine related pathology. The recipients underwent a mock transfer in a cycle prior to their donation cycle and if any difficulty was encountered a cervical dilatation was performed.
Only cycles with freshly ejaculated spermatozoa were included in the study. Semen samples were obtained from male partners of couples who underwent ICSI for an infertility treatment with donated oocytes. The male partners had no form of severe male infertility indications and cases of unexplained infertility were not included in the study. The SDF test was performed in 162 cases and 12 cases were excluded due to lower than expected (less than 8) donated oocytes (n = 7) or incomplete data (n = 5). Cases which did not fulfill the above inclusion criteria were also excluded.
Semen samples were fresh and collected by masturbation into non-toxic sterile plastic jars after 3 days of sexual abstinence. The 150 collected samples were allowed to liquefy for 15–30 min at room temperature (24 °C) and were evaluated according to the WHO criteria (World Health Organization, 5th edition). The DFI measurements were performed on raw semen samples; therefore, the following parameters were assayed directly from the semen samples prior to density gradient centrifugation. Sperm samples were analyzed according to the following basic parameters: (i) quantity (ii) concentration (iii) motility, (iv) high motility, and (v) morphology using a light microscope (Nikon E 200, Japan). Sperm morphology was assessed according to Kruger’s strict criteria after Papanicolaou staining. Sperm concentration was assessed using a Makler counting chamber (Bruckberg, Germany) with the use of a sperm counter. Sperm motility was classified as grade A, B or C and at least 500 spermatozoa were scored with a 40 × objective. Total motility was calculated as the total of motility rates A and B, while motility grade A was considered as forward.
Stimulation protocol and recipient preparation
Ovarian stimulation was performed on donors with a fixed day-6 gonadotropin-releasing hormone (GnRH) antagonist protocol [24]. The recipients underwent endometrial preparation as previously described elsewhere [25]. Ovarian function was first down-regulated in the luteal phase with a single-dose of GnRH-agonist depot (Arvekap, 3.75 mg) beginning on day 21 of the previous cycle. One day after the commencement of the donor's next menstrual cycle, the recipients were instructed to begin taking estradiol valerate (Cyclacur or Progynova) at 2 mg/days for the first 4 days, 4 mg/days for days 5–8, and 6 mg/days until the pregnancy test. The afternoon of oocyte donation collection, the recipients were administered 200 mg of progesterone (Utrogestan) intravaginally; this continued as 200 mg, three times a day, until a fetal heartbeat was observed by ultrasound. Recipients without menstruation followed the same protocol without the GnRH agonist. Endometrial development was evaluated by ultrasound scan; the endometrium was considered adequately prepared for embryo transfer when the endometrial thickness was > 9 mm. Two embryos were transferred into each recipient.
Sperm preparation for ICSI
After liquefaction and semen analysis, spermatozoa were prepared using density gradient centrifugation (90% and 50%) with sperm dual gradient media (Isolate, Irvine Scientific). After the two layers were prepared in a conical centrifuge tube, 2 ml of the liquefied sperm semen was dispensed onto the upper layer (50%) and were centrifuged for 20 min at 300 g. Then, the layers were removed, and the sperm pellet was transferred into a new sterile tube to be washed. For the washing 3 ml of sperm washing medium (Irvine Scientific) was added, the pellet was resuspended and centrifuged at 300 g for 10 min, and the supernatant was removed. The washing step was performed twice. Qualified spermatozoa were selected from the precipitate. According to the concentration and motility after preparation, the samples were used for ICSI, where a single spermatozoon that appeared to be morphologically normal was selected.
Assessment of sperm DNA fragmentation index (DFI)
DFI was determined by the SCD technique, using the Halosperm kit G2 (Halotech DNA SL). Sperm samples raw (not centrifuged or washed) from each patient were diluted to a maximum concentration of 1 × 106/ml in phosphate-buffered saline (PBS). Aliquots of low-melting point agarose gel in microcentrifuge tubes were provided with the kit (Halosperm, INDAS Biotech, Madrid, Spain). Microcentrifuge tubes containing 100 μl of agarose were immersed in a distilled water bath at 90–100 °C for 5 min to melt the agarose and then for 5 min at 37 °C. After 5 min of incubation for temperature equilibration at 37 °C, 50 μl of sperm samples diluted in PBS were added to the microcentrifuge tubes and mixed gently. A 10 μl drop of this mixture was placed on a precoated slide provided by the kit and covered with a 22 × 22 mm coverslip. The covered slides were maintained in a refrigerator at 4 °C for 5 min to solidify the agarose and to produce a microgel with embedded spermatozoa. Then, the coverslips were removed gently and the precoated slides were placed horizontally for a 7-min incubation in acid solution previously prepared by mixing 80 μl of HCL into 10 ml of distilled water for 20 min. Then, the slides were incubated in lysis solution provided by kit. After rinsing with distilled water for 5 min, the slides were air-dried in room temperature, dehydrated in increasing concentrations of ethanol (20%, 70%, and 100%) for 2 min and then air-dried. For staining, the slides immersed in staining solution A (SSA) and staining solution B (SSB) that provided by the kit, for 6 min each. The slides were allowed to dry at room temperature and either observed in a bright-field microscope or stored at 4 °C.
One thousand (1000) spermatozoa per sample were scored under the 100 × objective of the microscope. Spermatozoa were classified according to the size of the halo that encircled their heads. Spermatozoa with large halos (thicknesses that were similar to or larger than the length of the smallest diameter of the core) and spermatozoa with medium sized halos (thickness greater than 1/3 of the smallest diameter of the core and less than the smallest diameter of the core) were considered as non-fragmented-DNA spermatozoa, while those with no halos at all or halos appearing degraded were considered as DNA-fragmented spermatozoa (Fig. 1b) [11].
A threshold value of 25% DNA fragmentation was used to determine if SCD test was predictive in ICSI outcome. This cut-off value was proposed because a higher infertility rate has been found in patients with > 25.5% Halosperm-positive spermatozoa compared with those with less than 25.5% DNA fragmentation [26].
Statistical analysis
Numeric variables were expressed as a mean ± SD, while categorical variables were expressed as percentages (%). The normality of the distribution was controlled for all numerical data with the Kolmogorov–Smirnov test, as previously described [27]. The independent-samples t test was used to compare non-parametric data, while the dependent-samples t test was used for parametric data. Fisher’s exact test was used to compare categorical data. Linear regression model was used to correlate DFI with various epidemiological, clinical and laboratory outcomes. Statistical significance was defined at p < 0.05. The Statistical Package for the Social Sciences (SPSS) 17.0 was used to perform statistical analysis.
Results
A total of 150 sperm samples were provided by 150 males for analysis. The men’s age ranged from 32 to 58 years (mean 43.4 ± 5.5 years), height from 165 to 188 cm (mean 176.9 ± 5.4 cm), and weight from 52 to 130 kg (mean 82 ± 12.3 kg) (Table 1). Moreover, the mean number of previously unsuccessful efforts of assisted reproductive technology (ART) treatments was 0.52, between 0 and 2 efforts.
The mean and range of the considered parameters were (i) quantity: 3.58 ml ( ± 1.1) between 1.5 ml and 6 ml (ii) concentration: 49.5 × 106 ( ± 31.8) between 1 × 106 and 120 × 106 (iii) motility %: 54.9% ( ± 19.2), between 12 and 90% (iv) forward motility %: 32.6% ( ± 17.3), between 1 and 80% (v) morphology %: 18.4% ( ± 7.3) morphologically normal spermatozoa, between 1 and 30% (Table 2). The mean total number of available blastocysts/case was 4.9 (range 1–10), while the mean number of good quality blastocysts was 2.7 (range 0–7). The mean number of oocytes obtained per case was 9.76, the mean fertilization rate was 71.4% ( ± 18.7), and the mean positive pregnancy outcome was 60.3% (Table 3).
The correlation of sperm DNA fragmentation index with male epidemiological characteristics is shown in Table 1. DFI was positively correlated with male age (r = 0.23; p = 0.0046). On the contrary, no significant correlation was observed between DFI and height or weight.
Table 2 shows the correlation of DFI with standard semen parameters. DFI was significantly reversely correlated with sperm general motility and type A motility (r = − 0.29, r = − 0.27, respectively; p < 0.05). However, there were no statistically significant differences between DFI and sperm concentration or sperm morphology (r = 0.01 and r = − 0.07; p = 0.012 and p = 0.019 respectively).
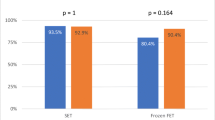
Table 3 presents the correlation of DFI with clinical and laboratory outcomes. DFI was not significantly correlated with the oocyte fertilization rate, total number of blastocysts, or pregnancy outcome in couples with donated oocytes. Furthermore, although elevated DFI presented a trend towards association with good embryo quality, the correlation was not statistically significant (r = − 0.20, p = 0.08). Finally, when using a threshold of 25%, no effect of DNA fragmentation was detected on pregnancy outcome (Table 4).
Discussion
High DFI, which is generated by defects in chromatin remodeling during spermiogenesis or due to apoptosis during meiosis I [28], is a modern aspect of the so-called ‘male factor' that causes infertility. Conventional semen analysis provides a limited prediction of male fertility potential and does not always ensure the correct diagnosis of male infertility. Nevertheless, the DFI could provide extra information concerning the quality of a semen sample. This prospective, observational study was designed to evaluate whether the assessment of sperm nuclear-DNA integrity has a predictive value for the clinical outcome in the oocyte donation cycle and whether it is correlated with semen parameters. To this end, we measured the DFI of sperm samples from couples undergoing oocyte donation cycles directly prior to density gradient centrifugation, and correlated it with epidemiological characteristics of male partners, semen parameters and clinical outcomes.
In the present study we investigated the connection between DNA fragmentation damage and general male characteristics, and we found that neither height nor weight affected the DFI. These results are in consistent with previous reports [29, 30], even though some studies support the opposite conclusion, in particular in cases of overweight and obese males including more data on the lifestyle of individuals and relative statistical models [31, 32]. On the other hand, this study strengthens the correlation between advanced paternal age and sperm DNA damage, something that has been reported previously [33, 34]. Similarly, it has been reported that advanced male age increases sperm DNA damage in association with single-stranded DNA [35] and decreases the ability of spermatozoa to fertilize an oocyte [36]. A recent study [37] reported that advanced paternal age negatively affects the clinical outcome in IVF couples. Based on our results, we propose that DNA fragmentation damage in older men could be the pathway that leads to this insufficiency.
Analyzing the impact of classical semen parameters on the DFI, we found that neither sperm concentration nor sperm morphology were correlated with the DFI score. In contrast to our results, other studies on infertile men have shown a statistically significant association between low sperm concentration and a high DFI [38, 39]. Moreover, it has been proposed that the selection of morphologically normal spermatozoa during ICSI could increase the chance of preserving sperm DNA integrity [40].
On the contrary, we observed a significant correlation between low sperm motility (forward and total) and DNA damage. Even though some studies agree with our data [41, 42], others show no connection between sperm motility and DNA fragmentation, not even when this factor is enhanced by the method of density gradient centrifugation [43, 44]. Yilmaz et al. [45], using the Halosperm test, compared sperm groups of low (DFI < 30%) and high (DFI > 30%) DNA fragmentation and reported that in untreated sperm the sperm concentration was lower and in treated sperm the sperm motility declined in the high DNA fragmentation group (DFI > 30%).
Concerning the biological and clinical outcome of our study, we report that in oocyte donation cycles increased DFI has no effect on the fertilization rate nor on embryo quality. It is interesting to point out that we observed a trend toward higher quality blastocysts when DFI was lower. Our data agree with reports by Larson-Cook et al., and Morris et al. [46, 47], and oppose those of Høst et al., Muriel et al., and Zhylkova et al. [48,49,50], that examined the DFI effect by evaluating either ICSI or IVF with various male infertility factors and not exclusively fresh sperm. Our contradictory results could be due to the use of ICSI process with donor oocytes and sperm of males with no severe infertility factors that may have less impact on successful pronuclear stage development during fertilization or competent embryos.
The lack of effect of DFI on the fertilization rate may be explained by the fact that sperm DNA does not participate in the fertilization process since spermatozoa with fragmented DNA can successfully fertilize oocytes [51]. The effect of DNA fragmentation on embryo development is revealed later, on day 3 (at the four- to eight-cell stage), when the paternal genome is activated [52]. As a result, the development of the fertilized oocyte usually stops, or there is possible development of an abnormal embryo [53]. Fatehi et al. [54] reported that oocytes fertilized by spermatozoa containing DNA damage showed impaired embryo development after the second division, and only scattered formed blastocysts were observed. Oocytes are capable of repairing sperm DNA fragmentation up to a certain point and the amount of damage correction is higher in good quality oocytes [55]. Therefore, we can attribute the fact that an elevated DFI did not affect embryo development in our study to the use of good quality donated oocytes, which were sufficiently capable of repairing DNA damage.
Several previous studies reported that patients with higher DFIs seem to have lower rates of successful pregnancy [56, 57]. On the contrary, our results showed that pregnancy outcome is not affected by increased DFI, in agreement with the studies of Esbert et al. [23] and Gandini et al. [58]. No statistically significant differences were found in DNA fragmentation percentages between cases with pregnant and non-pregnant women. Notably, using a 25% threshold of DFI we observed a trend toward a lower pregnancy rate when DFI exceeded this value; however, this difference was not statistically significant. The above lack of correlation between DFI and pregnancy outcome might be due to the standard practice of selecting the best quality embryos for transfer or that ICSI process increases the possibility to select a normal spermatozoon. Either the sufficiency of ICSI or the selection of exclusively competent blastocysts possibly able to repair sperm DNA damage could be reasons to our contradictory results with the above studies that support an effect of increased DFI on pregnancy outcome. Both the good embryo development and the good pregnancy rates we observed could be attribute to elimination of DFI-affected sperm during preparation and sperm selection for insemination, resulting in mostly non-fragmented spermatozoa being chosen for ICSI.
Even in oocyte donation cases, we noticed that the presence of high levels of DNA damage found in some semen samples associated with normal semen parameters, according to the WHO criteria, gave clinical pregnancies and vice versa. Therefore, in terms of reducing the possible effect of paternal DNA damage in couples undergoing an oocyte donation program with no severe male infertility factor, sperm DNA fragmentation analysis may not be a useful tool for evaluation of semen samples, before their use for ICSI and for providing an accurate prediction of clinical outcome.
One of the limitations of the current study is the low number of cases with donated oocytes, plus the lack of a follow-up observation regarding the rates of ongoing pregnancy, pregnancy loss and life-birth that could be analyzed. Moreover, the evaluation of DFI in raw or treated (centrifuged, washed) sperm is still a matter of debate [59]. In our study, we measured the DFI in raw sperm so as to avoid generating damaging forces caused by centrifugation and to achieve higher specificity and positive predictive value in our results than with centrifuged sperm as reported in previous studies [60, 61]. However, some studies do not support the use of raw sperm for measuring the DFI [62, 63]. Therefore, further research, including more cases and DFI measurement in both treated and untreated sperm is required to substantiate our findings. In addition to the above limitations, it could not be avoided that the current SDF tests do not directly measure DNA breaks but rather assess the propensity to sperm DNA damage in response to chemical treatment [64]. Considering this, even if the intact chromatin is not necessary for fertilization during ICSI as we mention, it might affect embryo development, thus reflecting life delivery and abortion rates. In fact, it was found that the parameters of SDF tests may not related to fertilization rates, embryo quality, and pregnancy rates in IVF and ICSI, but might be associate with spontaneous abortion rates [65]. In this context, further case-dependent research and consensus regarding the methodology for DNA damage evaluation by targeting the type of DNA defects and the utility of these tests to clinical practice is needed. However, choosing to perform the study on oocyte donation cycles has the advantage of eliminating female factor infertility, avoiding thus any confusion and statistical bias that could be faced when analyzing our data related to male factor infertility.
In conclusion, DFI is not significantly correlated with embryological and clinical outcomes in cycles performed with donated oocytes. The good clinical rates of pregnancy and embryo quality that seem to be independent of DFI could be due to the possible selection of normal sperm for ICSI and to the use of oocytes from young and healthy donors. Sperm motility and advanced male age are significantly associated with DFI, although no statistically significant effect on either other semen parameters or epidemiological characteristics, seems to be present. The evaluation of patients' sperm prior to ART by DFI measurement is not essential for oocyte donation cycles.
References
Schulte RT, Ohl DA, Sigman M, Smith GD (2010) Sperm DNA damage in male infertility: etiologies, assays, and outcomes. J Assist Reprod Genet 27:3–12. https://doi.org/10.1007/s10815-009-9359-x
Sakkas D, Alvarez JG (2010) Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril 93:1027–1036. https://doi.org/10.1016/j.fertnstert.2009.10.046
Avendaño C, Franchi A, Duran H, Oehninger S (2010) DNA fragmentation of normal spermatozoa negatively impacts embryo quality and intracytoplasmic sperm injection outcome. Fertil Steril 94:549–557. https://doi.org/10.1016/j.fertnstert.2009.02.050
Li Z, Wang L, Cai J, Huang H (2006) Correlation of sperm DNA damage with IVF and ICSI outcomes: a systematic review and meta-analysis. J Assist Reprod Genet 23:367–376. https://doi.org/10.1007/s10815-006-9066-9
Aitken RJ, Gordon E, Harkiss D, Twigg JP, Milne P, Jennings Z, Irvine DS (1998) Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod 59:1037–1046
Taherzadeh S, Khalili MA, Agha-Rahimi A, Anbari F, Ghazali S, Macchiarelli G (2017) Vitrification increased vacuolization of human spermatozoa: application of MSOME technology. J Reprod Infertil 18:225–230
Nottola SA, Albani E, Coticchio G, Palmerini MG, Lorenzo C, Scaravelli G, Borini A, Levi-Setti PE, Macchiarelli G (2016) Freeze/thaw stress induces organelle remodeling and membrane recycling in cryopreserved human mature oocytes. J Assist Reprod Genet 33:1559–1570. https://doi.org/10.1007/s10815-016-0798-x
Palmerini MG, Antinori M, Maione M, Cerusico F, Versaci C, Nottola SA, Macchiarelli G, Khalili MA, Antinori S (2014) Ultrastructure of immature and mature human oocytes after cryotop vitrification. J Reprod Dev 60:411–420. https://doi.org/10.1262/jrd.2014-027
Agha-Rahimi A, Khalili MA, Nottola SA, Miglietta S, Moradi A (2016) Cryoprotectant-free vitrification of human spermatozoa in new artificial seminal fluid. Andrology 4:1037–1044. https://doi.org/10.1111/andr.12212
Chohan KR, Griffin JT, Lafromboise M, Jonge CJ, Carrell DT (2006) Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl 27:53–59. https://doi.org/10.2164/jandrol.05068
Fernández JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, Enciso M, LaFromboise M, De Jonge C (2005) Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril 84:833–842. https://doi.org/10.1016/j.fertnstert.2004.11.089
Ribas-Maynou J, García-Peiró A, Fernández-Encinas A, Abad C, Amengual MJ, Prada E, Navarro J, Benet J (2013) Comprehensive analysis of sperm DNA fragmentation by five different assays: TUNEL assay, SCSA, SCD test and alkaline and neutral Comet assay. Andrology 1:715–722. https://doi.org/10.1111/j.2047-2927.2013.00111.x
Fernández JL, Muriel L, Rivero MT, Goyanes V, Vazquez R, Alvarez JG (2003) The sperm chromatin dispersion test: a simple method for the determination of sperm DNA fragmentation. J Androl 24:59–66. https://doi.org/10.1002/j.1939-4640.2003.tb02641.x
Cissen M, Wely MV, Scholten I, Mansell S, Bruin JP, Mol BW, Braat D, Repping S, Hamer G (2016) Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: a systematic review and meta-analysis. PLoS ONE 11:e0165125. https://doi.org/10.1371/journal.pone.0165125
Kirkman-Brown JC, De Jonge C (2017) Sperm DNA fragmentation in miscarriage—a promising diagnostic, or a test too far? Reprod Biomed Online 34:3–4. https://doi.org/10.1016/j.rbmo.2016.12.002
Osman A, Alsomait H, Seshadri S, El-Toukhy T, Khalaf Y (2015) The effect of sperm DNA fragmentation on live birth rate after IVF or ICSI: a systematic review and meta-analysis. Reprod Biomed Online 30:120–127. https://doi.org/10.1016/j.rbmo.2014.10.018
Ioannou D, Tempest HG (2018) Does genome organization matter in spermatozoa? A refined hypothesis to awaken the silent vessel. Syst Biol Reprod Med 64:518–534. https://doi.org/10.1080/19396368.2017.1421278
Practice Committee of the American Society for Reproductive Medicine (2013) The clinical utility of sperm DNA integrity testing: a guideline. Fertil Steril 99:673–677. https://doi.org/10.1016/j.fertnstert.2012.12.049
Ménézo Y, Dale B, Cohen M (2010) DNA damage and repair in human oocytes and embryos: a review. Zygote 18:357–365. https://doi.org/10.1017/S0967199410000286
Vazharova R, Kremensky I (2016) Individual capacity for DNA repair and maintenance of genomic integrity: a fertile ground for studies in the field of assisted reproduction. Biotechnol Biotechnol Equip 30:419–433
Marchetti F, Essers J, Kanaar R, Wyrobek AJ (2007) Disruption of maternal DNA repair increases sperm-derived chromosomal aberrations. Proc Natl Acad Sci USA 104:17725–17729. https://doi.org/10.1073/pnas.0705257104
Gat I, Li N, Yasovich N, Antes R, Kuznyetsov V, Zohni K, Weizman NF, Librach C (2018) Sperm DNA fragmentation index does not correlate with blastocyst euploidy rate in egg donor cycles. Gynecol Endocrinol 34:212–216. https://doi.org/10.1080/09513590.2017.1379500
Esbert M, Pacheco A, Vidal F, Florensa M, Riqueros M, Ballesteros A, Garrido N, Calderón G (2011) Impact of sperm DNA fragmentation on the outcome of IVF with own or donated oocytes. Reprod Biomed Online 23:704–710. https://doi.org/10.1016/j.rbmo.2011.07.010
Prapas N, Prapas Y, Panagiotidis Y, Prapa S, Vanderzwalmen P, Schoysman R, Makedos G (2005) GnRH agonist versus GnRH antagonist in oocyte donation cycles: a prospective randomized study. Hum Reprod 20:1516–1520. https://doi.org/10.1093/humrep/deh832
Prapas N, Tavaniotou A, Panagiotidis Y, Prapa S, Kasapi E, Goudakou M, Papatheodorou A, Prapas Y (2009) GnRH antagonists and endometrial receptivity in oocyte recipients: a prospective randomized trial. Reprod Biomed Online 18:276-281. https://www.rbmonline.com/Article/3602
López G, Lafuente R, Checa MA, Carreras R, Brassesco M (2013) Diagnostic value of sperm DNA fragmentation and sperm high-magnification for predicting outcome of assisted reproduction treatment. Asian J Androl 15:790–794. https://doi.org/10.1038/aja.2013.81
Petousis S, Prapas Y, Papatheodorou A, Margioula-Siarkou C, Papatzikas G, Panagiotidis Y, Karkanaki A, Ravanos K, Prapas N (2018) Fluorescence in situ hybridisation sperm examination is significantly impaired in all categories of male infertility. Andrologia 50:e12847. https://doi.org/10.1111/and.12847
Gorczyca W, Traganos F, Jesionowska H, Darzynkiewicz Z (1993) Presence of DNA strand breaks and increased sensitivity of DNA in situ to denaturation in abnormal human sperm cells: analogy to apoptosis of somatic cells. Exp Cell Res 207:202–205
Rybar R, Kopecka V, Prinosilova P, Markova P, Rubes J (2011) Male obesity and age in relationship to semen parameters and sperm chromatin integrity. Andrologia 43:286–291. https://doi.org/10.1111/j.1439-0272.2010.01057.x
Tunc O, Bakos HW, Tremellen K (2011) Impact of body mass index on seminal oxidative stress. Andrologia 43:121–128. https://doi.org/10.1111/j.1439-0272.2009.01032.x
Chavarro JE, Toth TL, Wright DL, Meeker JD, Hauser R (2010) Body mass index in relation to semen quality, sperm DNA integrity, and serum reproductive hormone levels among men attending an infertility clinic. Fertil Steril 93:2222–2231. https://doi.org/10.1016/j.fertnstert.2009.01.100
Fariello RM, Pariz JR, Spaine DM, Cedenho AP, Bertolla RP, Fraietta R (2012) Association between obesity and alteration of sperm DNA integrity and mitochondrial activity. B J U Int 110:863–867. https://doi.org/10.1111/j.1464-410X.2011.10813.x
Tandara M, Bajic A, Tandara L, Sunj M, Jurisic Z, Jukic M (2013) Correlation between proportions of sperm with DNA fragmentation assessed by Halosperm test and values of standard quality parameters of semen and possible impact on embryo quality. Zdrav Vestn 82:298–307
Vagnini L, Baruffi RLR, Mauri AL, Petersen CG, Massaro FC, Pontes A, Oliveira JB, Franco JG Jr (2007) The effects of male age on sperm DNA damage in an infertile population. Reprod Biomed Online 15:514–519
Schmid TE, Eskenazi B, Baumgartner A, Marchetti F, Young S, Weldon R, Anderson D, Wyrobek AJ (2006) The effects of male age on sperm DNA damage in healthy non-smokers. Hum Reprod 22:180–187. https://doi.org/10.1093/humrep/del338
Frattarelli JL, Miller KA, Miller BT, Elkind-Hirsch K, Scott RT (2008) Male age negatively impacts embryo development and reproductive outcome in donor oocyte assisted reproductive technology cycles. Fertil Steril 90:97–103. https://doi.org/10.1016/j.fertnstert.2007.06.009
Kaarouch I, Bouamoud N, Madkour A, Louanjli N, Saadani B, Assou S, Aboulmaouahib S, Amzazi S, Copin H, Benkhalifa M, Sefrioui O (2018) Paternal age: negative impact on sperm genome decays and IVF outcomes after 40 years. Mol Reprod Dev. https://doi.org/10.1002/mrd.22963
Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, Aitken R (2000) DNA integrity in human spermatozoa: relationships with semen quality. J Androl 21:33–44
Sheikh N, Amiri I, Farimani M, Najafi R, Hadeie J (2008) Correlation between sperm parameters and sperm DNA fragmentation in fertile and infertile men. Int J Reprod Biomed (Yazd) 6:13–18
Avendaño C, Oehninger S (2011) DNA fragmentation in morphologically normal spermatozoa: how much should we be concerned in the ICSI era? J Androl 32:356–363. https://doi.org/10.2164/jandrol.110.012005
Belloc S, Benkhalifa M, Cohen-Bacrie M, Dalleac A, Chahine H, Amar E, Zini A (2014) Which isolated sperm abnormality is most related to sperm DNA damage in men presenting for infertility evaluation. J Assist Reprod Genet 31:527–532. https://doi.org/10.1007/s10815-014-0194-3
Rafighdoost H, Farsi MM, Javadi M, Khafri S (2013) Relationship between sperm parameters and DNA fragmentation using a halosperm kit. Anat Sci J 10:79–86
Enciso M, Iglesias M, Galán I, Sarasa J, Gosálvez A, Gosálvez J (2011) The ability of sperm selection techniques to remove single-or double-strand DNA damage. Asian J Androl 13:764–768. https://doi.org/10.1038/aja.2011.46
Zini A, Sigman M (2009) Are tests of sperm DNA damage clinically useful? Pros and cons. J Androl 30:219–229. https://doi.org/10.2164/jandrol.108.006908
Yılmaz S, Zergeroğlu AD, Yılmaz E, Sofuoglu K, Delikara N, Kutlu P (2010) Effects of sperm DNA fragmentation on semen parameters and ICSI outcome determined by an improved SCD test, Halosperm. Int J Fertil Steril 4:73–78
Larson-Cook KL, Brannian JD, Hansen KA, Kasperson KM, Aamold ET, Evenson DP (2003) Relationship between the outcomes of assisted reproductive techniques and sperm DNA fragmentation as measured by the sperm chromatin structure assay. Fertil Steril 80:895–902. https://doi.org/10.1016/S0015-0282(03)01116-6
Morris ID, Ilott S, Dixon L, Brison DR (2002) The spectrum of DNA damage in human sperm assessed by single cell gel electrophoresis (Comet assay) and its relationship to fertilization and embryo development. Hum Reprod 17:990–998
Høst E, Lindenberg S, Smidt-Jensen S (2000) The role of DNA strand breaks in human spermatozoa used for IVF and ICSI. Acta Obstet Gynecol Scand 79:559–563. https://doi.org/10.1034/j.1600-0412.2000.079007559.x
Muriel L, Garrido N, Fernández JL, Remohí J, Pellicer A, de los Santos MJ, Meseguer M (2006) Value of the sperm deoxyribonucleic acid fragmentation level, as measured by the sperm chromatin dispersion test, in the outcome of in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril 85:371–383. https://doi.org/10.1016/j.fertnstert.2005.07.1327
Zhylkova I, Feskov O, Feskova I, Fedota O, Feskov V (2014) Sperm DNA fragmentation as a factor of male low reproductive function in IVF practice. Int J Biol 6:75–81
Twigg JP, Irvine DS, Aitken RJ (1998) Oxidative damage to DNA in human spermatozoa does not preclude pronucleus formation at intracytoplasmic sperm injection. Hum Reprod 13:1864–1871
Simon L, Murphy K, Shamsi MB, Liu L, Emery B, Aston KI, Hotaling J, Carrell DT (2014) Paternal influence of sperm DNA integrity on early embryonic development. Hum Reprod 29:2402–2412. https://doi.org/10.1093/humrep/deu228
Virro MR, Larson-Cook KL, Evenson DP (2004) Sperm chromatin structure assay (SCSA®) parameters are related to fertilization, blastocyst development, and ongoing pregnancy in in vitro fertilization and intracytoplasmic sperm injection cycles. Fertil Steril 81:1289–1295
Fatehi AN, Bevers MM, Schoevers E, Roelen BAJ, Colenbrander B, Gadella BM (2006) DNA damage in bovine sperm does not block fertilization and early embryonic development but induces apoptosis after the first cleavages. J Androl 27:176–188. https://doi.org/10.2164/jandrol.04152
Sakkas D, Urner F, Bianchi PG, Bizzaro D, Wagner I, Jaquenoud N, Manicardi G, Campana A (1996) Sperm chromatin anomalies can influence decondensation after intracytoplasmic sperm injection. Hum Reprod 11:837–843
Bungum M, Humaidan P, Spano M, Jepson K, Bungum L, Giwercman A (2004) The predictive value of sperm chromatin structure assay (SCSA) parameters for the outcome of intrauterine insemination, IVF and ICSI. Hum Reprod 19:1401–1408. https://doi.org/10.1093/humrep/deh280
Henkel R, Hajimohammad M, Stalf T, Hoogendijk C, Mehnert C, Menkveld R, Gips H, Schill WB, Kruger TF (2004) Influence of deoxyribonucleic acid damage on fertilization and pregnancy. Fertil Steril 81:965–972. https://doi.org/10.1016/j.fertnstert.2003.09.044
Gandini L, Lombardo F, Paoli D, Caruso F, Eleuteri P, Leter G, Ciriminna R, Culasso F, Dondero F, Lenzi A, Spanò M (2004) Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod 19:1409–1417. https://doi.org/10.1093/humrep/deh233
Borini A, Tarozzi N, Nadalini M (2017) Sperm DNA fragmentation testing in male infertility work-up: are we ready? Transl Androl Urol 6:S580–S582 https://doi.org/10.21037/tau.2017.03.81
Simon L, Lutton D, McManus J, Lewis SE (2011) Sperm DNA damage measured by the alkaline Comet assay as an independent predictor of male infertility and in vitro fertilization success. Fertil Steril 95:652–657. https://doi.org/10.1016/j.fertnstert.2010.08.019
Muratori M, Tarozzi N, Cambi M, Boni L, Iorio AL, Passaro C, Luppino B, Nadalini M, Marchiani S, Tamburrino L, Forti G, Maggi M, Baldi E, Borini A (2016) Variation of DNA fragmentation levels during density gradient sperm selection for assisted reproduction techniques: a possible new male predictive parameter of pregnancy? Medicine (Baltimore) 95:e3624. https://doi.org/10.1097/MD.0000000000003624
Jayaraman V, Upadhya D, Narayan PK, Adiga SK (2012) Sperm processing by swim-up and density gradient is effective in elimination of sperm with DNA damage. J Assist Reprod Genet 29:557–563. https://doi.org/10.1007/s10815-012-9742-x
Malvezzi H, Sharma R, Agarwal A, Abuzenadah AM, Abu-Elmagd M (2014) Sperm quality after density gradient centrifugation with three commercially available media: a controlled trial. Reprod Biol Endocrinol 12:121. https://doi.org/10.1186/1477-7827-12-121
Shafik A, Shafik AA, Shafik I, El Sibai O (2006) Molecular andrology as related to sperm DNA fragmentation/sperm chromatin biotechnology. Arch Androl 52:299–310. https://doi.org/10.1080/01485010600668363
Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, Hwu YM (2008) Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril 90:352–359. https://doi.org/10.1016/j.fertnstert.2007.06.018
Acknowledgements
Preliminary data regarding this study were presented as poster at the 10th European Congress of Andrology, October 2018 in Budapest, Hungary.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SA: Data collection or management, data analysis, manuscript writing. AP: Protocol/project development, data analysis, manuscript writing/editing. YPa: Protocol/project development, data analysis. SP: Data management, data analysis. NP: Data management, data analysis, manuscript editing. SAN: Data analysis, manuscript editing. MGP: Data collection or management. GM: Data analysis, manuscript editing. YPr: Protocol/project development, data management, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board of Iakentro Advanced Medical Center/ethics committee of Thessaloniki, Greece approved the study at 2/9/2013, Ref. Number 9/2013.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antonouli, S., Papatheodorou, A., Panagiotidis, Y. et al. The impact of sperm DNA fragmentation on ICSI outcome in cases of donated oocytes. Arch Gynecol Obstet 300, 207–215 (2019). https://doi.org/10.1007/s00404-019-05133-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05133-9