Abstract
Purpose
To evaluate if sperm DNA fragmentation (SDF) in the sample used for intracytoplasmic sperm injection (ICSI) impacts outcomes after euploid blastocyst transfer.
Methods
Prospective cohort study of couples undergoing IVF with preimplantation genetic testing for aneuploidy from December 2014–June 2017. Sperm collected on the day of ICSI was analyzed for SDF using the sperm chromatin structure assay (SCSA®). Semen analysis parameters, embryologic outcomes, and clinical outcomes after euploid blastocyst transfer were compared between groups with DNA fragmentation index (DFI) ≤ 15% and DFI > 15% using Mann–Whitney U, t tests, and generalized linear mixed effects models.
Results
Two hundred thirty-four patients were included. One hundred seventy-nine men had DFI ≤ 15% (low DFI group) and 55 men had DFI > 15% group (high DFI group). Total motile sperm and sperm concentration were significantly lower in the group with DFI > 15% vs. DFI ≤ 15%. There was no difference in fertilization (86.3 vs. 84.2%, adjusted OR (95% CI) 0.86 (0.63–1.18)), blastulation (49.5 vs. 48.8%, adjusted OR 1.02 (0.75–1.36)), or euploidy (55.7 vs. 52.1%, adjusted OR 0.96 (0.7–1.31)) between the low and high DFI groups, respectively. Clinical outcomes were similar between low and high DFI groups, including implantation rate (68.8 vs. 79.8%), ongoing pregnancy rate (65.9 vs. 72.6%), and miscarriage rate (4.2 vs. 8.8%), respectively.
Conclusion
Sperm DNA fragmentation on the day of ICSI is not associated with embryologic or clinical outcomes after euploid blastocyst transfer. Increasing levels of SDF are associated with low sperm concentration and total motile sperm count.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infertility is a common health concern and continues to be a growing problem as more men and women delay reproduction until later in life. Current data suggest that up to 15% of couples have trouble maintaining or achieving a pregnancy [1]. Among couples with fertility issues, 30–50% have some component of male factor associated with infertility, and as many as 10–20% have exclusively male factor as an identifiable cause [2, 3].
Despite the prevalence of male factor infertility, diagnostic options for these patients are inadequate to properly guide management. Currently, the gold standard for evaluation of male factor infertility is the semen analysis. While the semen analysis is useful for classifying patients as sub-fertile, indeterminate, or fertile, it lacks accurate diagnostic value in determining fecundity in patients with motile sperm [4, 5]. Furthermore, 15% of infertile males have normal semen parameters [6]. As a result, attempts to improve evaluation of semen quality in patients afflicted by male infertility have led to attempts to find other diagnostic options which are predictive of outcomes and may lead to additional treatment options.
Sperm DNA plays a critical role in the developing embryo and can be damaged prior to and during ejaculation. Such insults include over abundances of reactive oxygen species, varicocele, smoking, exposure to heavy metals, testicular heat, obesity, increasing paternal age, or testicular infections [7]. Sperm DNA fragmentation (SDF) has been associated with recurrent pregnancy loss and decreased live birth rates [7,8,9,10,11]. The sperm DNA fragmentation index (DFI) is a classification of the degree of DNA fragmentation. This is performed through the use of dyes or probes which can identify breaks in sperm DNA. Higher levels of SDF are more common in infertile men [12, 13]. Given these findings, sperm DFI has emerged as a means of analysis in some institutions as an additional assessment for predicting fecundity and guiding therapeutic management [11, 13].
Over the past two and a half decades, intracytoplasmic sperm injection (ICSI) has played a pivotal role in overcoming many complications presented by male factor infertility. Nonetheless, patients undergoing assisted reproductive measures with higher levels of sperm DFI, despite the use of ICSI, may still have poorer outcomes [11]. The exact reasoning for this remains unclear. There is also a well-documented association between recurrent early pregnancy loss and increasing sperm DFI [7,8,9,10]. It is postulated that there may be a genetic component that is responsible for these diminished results; however, it is yet to be determined if increasing DFI is directly correlated with embryonic aneuploidy.
There are limitations in existing literature on this topic. A majority of previous studies have evaluated SDF on a semen sample obtained prior to the IVF cycle. However, there is known intra-patient variability in SDF, and it has been demonstrated that both semen analysis parameters and SDF can significantly vary within the same male patient over time [14]. Therefore, the direct impact of SDF on IVF outcomes is most accurately assessed by evaluating SDF on the semen sample used for fertilization in that specific IVF cycle.
To our knowledge, no study to-date has accounted for embryonic aneuploidy when evaluating clinical outcomes in relation to SDF. Controlling for aneuploidy, which significantly impacts ongoing pregnancy and miscarriage rates, is imperative when attempting to focus on the impact of sperm DNA fragmentation on IVF outcomes. Furthermore, very few studies have evaluated the direct relationship between SDF and embryonic aneuploidy. The studies that have researched this question have examined particular subsets of patients, including patients with a history of recurrent pregnancy loss or those with advanced maternal age [15, 16]. Additionally, there were limitations in the genetic screening platform, as cleavage stage biopsy with fluorescence in situ hybridization (FISH) was used in these studies.
The primary objective of this study was to evaluate the impact of sperm DNA fragmentation in the semen sample used for ICSI on embryologic and clinical outcomes after euploid blastocyst transfer. Secondary endpoints included assessing for a correlation between SDF and embryonic aneuploidy, and evaluating for a relationship between SDF and semen analysis parameters.
Materials and methods
Study design and population
This is a prospective cohort study of couples undergoing IVF with ICSI and preimplantation genetic testing for aneuploidy (PGT-A) from December 2014 through June 2017. Patients were eligible to participate if this was their first cycle of IVF, PGT-A was planned, and female age was 35–40 years. This age was chosen in effort to focus on the specific relation between SDF and embryonic aneuploidy by minimizing the impact of oocyte-driven DNA repair, which is more or less likely at young and advanced maternal ages, respectively [17]. Exclusion criteria included a known genetic abnormality in either member of the couple, the use of cryopreserved, surgically obtained, or donor sperm, presence of a varicocele or communicating hydrosalpinx, or the use of an oocyte donor or gestational carrier. Institutional Review Board (IRB) approval was obtained through Copernicus Group IRB®.
Procedures
Females underwent ovarian stimulation with injectable gonadotropins using a gonadotropin releasing hormone (GnRH) agonist or antagonist protocol. When at least two follicles were ≥ 17 mm in size, final oocyte maturation was triggered with either a GnRH agonist or human chorionic gonadotropin. Transvaginal oocyte retrieval was performed 36 h later. The semen specimen was collected on the day of ICSI and semen analysis was performed. Semen samples meeting the minimum criteria of volume > 1 ml, concentration > 2 × 106/ml, and motility > 30% were included, and a 0.5-ml semen aliquot was isolated from the fresh semen specimen for SDF analysis. For samples not meeting minimum criteria (n = 37), the entire specimen was utilized for ICSI so as not to compromise clinical care. Isolated aliquots from study patients were frozen in liquid nitrogen and SDF was determined with the sperm chromatin structural assay (SCSA®) at SCSA® Diagnostics, Inc.
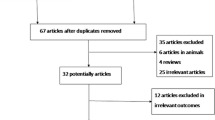
Mature oocytes were fertilized by ICSI and embryos underwent extended culture to the blastocyst stage. Trophectoderm biopsy was performed on suitable blastocysts for PGT-A utilizing quantitative real-time polymerase chain reaction (qPCR)-based screening for cases performed before July 2016 or next generation sequencing for all subsequent cases. Embryos with results consistent with segmental aneuploidy or mosaicism were designated aneuploid for purposes of the analysis. Euploid embryos were selected for embryo transfer. The majority of patients underwent a single embryo transfer in a subsequent frozen embryo transfer cycle (Fig. 1).
Analysis
Sperm DNA fragmentation was reported as the percentage of fragmented sperm DNA, known as the DNA fragmentation index (DFI). Patients were divided into two groups for analysis, DFI ≤ 15% and DFI > 15%. Demographic and semen analysis parameters were compared between the two groups using Mann–Whitney U and t tests, as appropriate. SDF was also evaluated in relation to semen analysis parameters from both the initial semen analysis prior to IVF as well as the semen sample used for ICSI.
Embryologic outcomes were analyzed using generalized linear mixed effects models and included rates of fertilization, blastulation, and aneuploidy. A random effects term was added to account for the repeated measures due to multiple oocytes from the same patient. Fertilization was defined as the number two pronuclear (2PN) embryos divided by the number of metaphase II oocytes (M2). Blastulation was defined as the number of blastocysts suitable for trophectoderm biopsy and cryopreservation divided by the number of 2PNs. Euploid rate was calculated as the number of euploid blastocysts divided by the number of blastocysts biopsied for PGT-A. Resulting odds ratios were adjusted for female age as generalized linear mixed effects models demonstrated that female age impacted both blastulation and aneuploidy rates.
Clinical outcomes included rates of implantation, miscarriage, and ongoing pregnancy. These clinical outcomes were compared between the two groups using Fisher’s exact test. The rates of single embryo transfer and frozen embryo transfer were also compared between the two DFI groups. Implantation was calculated as the number of gestational sacs divided by the number of embryos transferred. Miscarriage was calculated per clinical pregnancy (pregnancy loss after a gestational sac was visualized on ultrasound). Ongoing pregnancy was defined as the number of positive fetal heart rates at time of discharge at 8–9 weeks gestational age divided by the number of embryos transferred.
Results
Seven hundred twenty-seven patients were screened for participation in the study. Three hundred twenty-three patients met inclusion criteria and signed consents to participate. Of these patients, 89 were withdrawn (did not meet minimum sperm parameters on day of egg retrieval: 37; specimen not collected: 5; specimen compromised: 37; decided against PGT-A testing after enrollment: 2; canceled due to inadequate response: 2; spontaneous pregnancy: 1; changed mind: 5). Two hundred thirty-four patients who met inclusion criteria were included in the study.
Semen analysis parameters and embryologic outcomes
All 234 patients were included in the analysis of SDF in relation to semen analysis parameters (Table 1) and embryologic outcomes (Fig. 2). One hundred seventy-nine patients had DFI ≤ 15% (low DFI group) and 55 patients had DFI > 15% (high DFI group). There was no difference in female age between the two groups. The mean age of men in the high DFI group was older compared to the low DFI group (40.5 years vs. 38.3 years, respectively; p = 0.001). Total motile sperm and sperm concentration were significantly lower in the high DFI group versus the low DFI group, both on initial semen analysis obtained prior to IVF and on the semen sample used for ICSI (Table 1).
Clinical outcomes. One hundred eighty patients had an embryo transfer, 129 patients had a clinical pregnancy. Implantation, ongoing pregnancy, and miscarriage rates were similar between DFI groups (Fisher’s exact test, 2-sided). Data presented as mean; error bars = standard error. Implantation = # gestational sacs/# embryos transferred, ongoing pregnancy = # positive cardiac activity at discharge/# embryos transferred, miscarriage = # pregnancy loss/clinical pregnancy
Embryologic outcomes were evaluated both as unadjusted and adjusted odds ratios, as generalized linear mixed models indicated that female age impacted both blastulation and euploidy rates. After adjusting for female age, there was no significant difference in the odds of fertilization, blastulation, or euploidy between the low and high DFI groups (Table 2). Sperm DNA fragmentation does not appear to impact these embryologic outcomes after ICSI.
Clinical outcomes
One hundred eighty patients underwent euploid blastocyst transfer. Those not yet proceeding with embryo transfer most commonly had elected to pursue additional stimulation cycles for embryo accumulation or had no euploid embryos for transfer. Clinical outcome data are depicted in Fig. 2. There was no difference in rates of single embryo transfer (SET) (93.5% vs. 92.9%, p = 1) or frozen embryo transfer (80.4% vs. 90.4%, p = 0.164) between the low and high DFI groups, respectively (Fig. 1). One hundred twenty-nine patients achieved a clinical pregnancy (72%). There were no significant differences in implantation rate, miscarriage, or ongoing pregnancy between the two groups (Fig. 2).
Discussion
This prospective study demonstrates that sperm DNA fragmentation is inversely related to sperm motility and concentration. Increasing levels of DNA fragmentation are correlated with both low sperm concentration and total motile sperm count. These findings are consistent with previous literature that also suggests elevated levels of SDF are associated with abnormal semen analysis parameters [18, 19].
Sperm DNA fragmentation in the sample used for fertilization was not associated with embryologic outcomes, including fertilization, blastulation, and euploidy in this study. Notably, all patients in this study had fertilization with ICSI, since PGT-A was planned. There are data to suggest that elevated levels of sperm DNA fragmentation may negatively impact fertilization rates after conventional insemination [20]. It is possible that the process of ICSI circumvents any detriment that SDF has on fertilization. In this study population, there was no difference in blastulation or aneuploidy rates between the low and high DFI groups after ICSI.
In attempt to determine the specific impact of SDF on clinical outcomes, we controlled for embryonic aneuploidy in the evaluation of pregnancy and miscarriage rates as all patients underwent euploid blastocyst transfer. There was no impact of SDF on implantation, miscarriage, or ongoing pregnancy rates. The miscarriage rate after euploid blastocyst transfer were low in all study patients, and this low number of patients experiencing pregnancy loss may have limited the comparison of miscarriage rates between DFI groups. Other studies have also been limited in the analysis of miscarriage due to limited sample size, though trends towards a positive correlation between increasing SDF and miscarriage have been found [21]. It is possible that a larger cohort of study subjects would have resulted in observable differences in this clinical outcome.
This study has many strengths. Importantly, embryologic and clinical outcomes were evaluated based on levels of sperm DNA fragmentation in the semen sample used for fertilization. SDF in the sample used for ICSI may be more predictive of the actual effects of DNA fragmentation on IVF outcomes. One of the major limitations of previous studies is that SDF was measured on a semen sample obtained prior to the IVF cycle and then analyzed in relation to clinical outcomes after IVF at a later time. However, there is known intra-patient variability in SDF. In one such study, it was demonstrated that among men with high levels of SDF > 30%, only 63% of them had SDF in this range on successive testing, and the remaining 37% had SDF in the normal or intermediate range [14]. In this same study, a proportion of men who initially had low levels of SDF subsequently had DFI > 30% on repeat testing. These results indicate that it may be sub-optimal to associate IVF outcomes with SDF results obtained at an earlier time as there can be significant variability in SDF over time. Another notable strength of this study is that we controlled for embryonic aneuploidy in the evaluation of pregnancy outcomes. It is well-established that embryonic aneuploidy impacts pregnancy and miscarriage rates in both natural and assisted conceptions. Controlling for this significant confounder is therefore imperative when focusing on the direct impact of sperm DNA fragmentation on pregnancy outcomes after IVF. SDF was not associated with embryonic aneuploidy nor was it associated with clinical outcomes after euploid blastocyst transfer.
This study is not without limitations. All patients underwent fertilization with ICSI, which may limit the generalizability of the study results. While our data suggest that embryologic and clinical outcomes are not affected by SDF after ICSI, it is unclear if elevated SDF may have impacted these outcomes after conventional IVF [20]. Another important consideration is that patients were divided into groups using a DFI cut-off of 15%, which is considered to be intermediately elevated SDF. This cut-off was selected to optimize the number of patients in the normal DFI group and the elevated DFI group (which included DFI in the intermediate (DFI 16–25%) and high (DFI > 25%) ranges). There were only 19 patients with DFI > 25% in our study and 215 with DFI ≤ 25%. Separating patients into groups using a DFI cut-off of 25% would have limited the ability to analyze outcomes due to the low number of patients with DFI in the highest range. The low number of men with very high DFI may be due to the study design of excluding men with significant abnormalities on the semen analysis on the day of fertilization. In these instances, the entire sperm sample was used for fertilization, as it was important to the investigators that clinical care was not compromised in this study.
The results of this study evaluating IVF outcomes using a DFI cut-off of 15% are valuable. This separates patients into low (DFI ≤ 15%) and intermediate-high (DFI > 15%) SDF. There are data to suggest that DFI in both the intermediate and high ranges impact fertilization and live birth rates. In one such study, DFI > 10% was associated with decreased fertilization rates in IVF, and SDF > 20% decreased the odds of live birth [20]. In our study population, there does not appear to be a difference in embryologic or clinical outcomes between men with low SDF and those with intermediate to high levels of SDF.
In summary, this study demonstrates that sperm DNA fragmentation on the day of fertilization is not associated with fertilization, blastulation, aneuploidy, or pregnancy outcomes after euploid blastocyst transfer. Sperm DNA fragmentation does appear to be inversely correlated with semen analysis parameters. Increasing levels of sperm DNA fragmentation are associated with low sperm concentration and total motile sperm counts. Therefore, while SDF testing may be informative, it may not influence clinical decision making beyond what is determined from routine semen analysis, as men with low sperm concentration or motility are often advised to pursue ICSI based on semen analysis results alone. The results of this study suggest that men with sperm DNA fragmentation > 15% can expect equivalent IVF outcomes after ICSI and euploid embryo transfer compared to men with low levels of sperm DNA fragmentation.
References
Chandra A, Copen CE, Stephen EH. Infertility and impaired fecundity in the United States, 1982-2010: data from the National Survey of Family Growth. Natl Health Stat Rep. 2013;(67):1–18.
Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod. 1991;6(6):811–6.
Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur Urol. 2012;62(2):324–32.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. 2009. https://doi.org/10.1056/NEJMoa003005.
Esteves SC. Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int Braz J Urol. 2014;40(4):443–53.
Agarwal A, Allamaneni SS. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005;84(4):850–3.
Sakkas D. denny.sakkas@yale.edu, Division of Reproductive E, Infertility YUSoMNHC, Molecular Biometrics Inc NHC, Juan GA et al. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010;93(4):1027-36.
Tesarik J, Mendoza C, Greco E. Paternal effects acting during the first cell cycle of human preimplantation development after ICSI. Hum Reprod. 2002;17(1):184–9.
Kumar K, Deka D, Singh A, Mitra DK, Vanitha BR, Dada R. Predictive value of DNA integrity analysis in idiopathic recurrent pregnancy loss following spontaneous conception. J Assist Reprod Genet. 2012;29(9):861–7.
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2012;98(2):294–301.
Esteves SC, Roque M, Bradley CK, Garrido N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: systematic review and meta-analysis. Fertil Steril. 2017;108(3):456–67.
Bungum M. Sperm DNA integrity assessment: a new tool in diagnosis and treatment of fertility. Obstet Gynecol Int. 2011;2012:531042.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2006;22(1):174–9.
Erenpreiss J, Bungum M, Spano M, Elzanaty S, Orbidans J, Giwercman A. Intra-individual variation in sperm chromatin structure assay parameters in men from infertile couples: clinical implications. Hum Reprod. 2006;21(8):2061–4.
Bronet F, Martínez E, Gaytán M, Liñán A, Cernuda D, Ariza M, et al. Sperm DNA fragmentation index does not correlate with the sperm or embryo aneuploidy rate in recurrent miscarriage or implantation failure patients. Hum Reprod. 2012;27(7):1922–9.
Kaarouch I, Bouamoud N, Louanjli N, Madkour A, Copin H, Benkhalifa M, et al. Impact of sperm genome decay on Day-3 embryo chromosomal abnormalities from advanced-maternal-age patients. Mol Reprod Dev. 2015;82(10):809–19.
González-Marín C, Gosálvez J, Roy R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int J Mol Sci. 2012;13(11):14026–52.
Al Omrani B, Al Eisa N, Javed M, Al Ghedan M, Al Matrafi H, Al SH. Associations of sperm DNA fragmentation with lifestyle factors and semen parameters of Saudi men and its impact on ICSI outcome. Reprod Biol Endocrinol. 2018;16(1):49.
Belloc S, Benkhalifa M, Cohen-Bacrie M, Dalleac A, Amar E, Zini A. Sperm deoxyribonucleic acid damage in normozoospermic men is related to age and sperm progressive motility. Fertil Steril. 2014;101(6):1588–93.
Oleszczuk K, Giwercman A, Bungum M. Sperm chromatin structure assay in prediction of in vitro fertilization outcome. Andrology. 2016;4(2):290–6.
Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, Hwu YM. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90(2):352–9.
Funding
This research was supported by a grant from the Foundation for Embryonic Competence, Basking Ridge, New Jersey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional Review Board (IRB) approval was obtained through Copernicus Group IRB®.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Green, K.A., Patounakis, G., Dougherty, M.P. et al. Sperm DNA fragmentation on the day of fertilization is not associated with embryologic or clinical outcomes after IVF/ICSI. J Assist Reprod Genet 37, 71–76 (2020). https://doi.org/10.1007/s10815-019-01632-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01632-5