Abstract
Purpose
Studies on the influence of CO2 pneumoperitoneum on the abdominal cavity during robotic procedures are lacking. This is the first study to evaluate surgical field modifications related to CO2 pressure, during laparoscopic and robotic surgery.
Methods
Consecutive patients scheduled for laparoscopic or robotic hysterectomy were enrolled in the study. To evaluate the level of operative field visualization, a dedicated form has been designed based on the evaluation of four different areas: Douglas space, vesico-uterine fold and, bilaterally, the broad ligament. During the initial inspection, an assistant randomly set the CO2 pressure at 15, 10 and 5 mmHg, and the surgeon, not aware of the CO2 values, was asked to give an evaluation of the four areas for each set pressure.
Results
In laparoscopic group, CO2 pressure significantly influenced the surgical field visualization in all four areas analyzed. The surgeon had a good visualization only at 15 mmHg CO2 pressure; visualization decreased with a statistically significant difference from 15 to 5, 15–10 and 10–5 mmHg. In robotic group, influence of CO2 pressure on surgical areas visualization was not straightforward; operative field visualization remained stable at any pressure value with no significant difference.
Conclusions
Pneumoperitoneum pressure significantly affects the visualization of the abdomino-pelvic cavity in laparoscopic procedures. Otherwise, CO2 pressure does not affect the visualization of surgical field during robotic surgery. These findings are particularly significant especially at low CO2 pressure with potential implications on peritoneal environment and the subsequent post-operative patient recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robotic surgery is one of the most important innovations in the field of minimally invasive surgery: the data published to date demonstrate significant benefits of robotic surgery compared to traditional laparoscopy in terms of length of hospital stay, post-operative pain and recovery of normal physiological functions [1, 2]. The robotic surgical technique as the laparoscopic one, is based on the visualization of the abdominal organs by the distension of the peritoneal cavity through the use of carbon dioxide. However, studies on laparoscopy evidenced how intra-abdominal CO2 insufflation is cause of hemodynamic changes and metabolic effects, in particular insufflation pressure and duration of pneumoperitoneum lead to damage of the mesothelium and adhesions formation, with clinical subsequences [2]. In these cases and commonly, pneumoperitoneum is established at 10–15 mmHg CO2 [3]. Studies on the influence of CO2 pneumoperitoneum on the abdominal cavity during robotic procedures are lacking in particular there are no data on its effect on the surgical field visualization. We, therefore, aimed to evaluate surgical field modifications related to CO2 pressure, during laparoscopic and robotic surgery to compare those different techniques and highlight potential advantages of robotic surgery.
Materials and methods
This observational study was conducted at the Department of Gynecology at Campus Biomedico of Rome from July 2012 to October 2012. Patients scheduled for laparoscopic or robotic hysterectomy were enrolled consecutively. Inclusion criteria were: age 35–60 years, BMI 18–30 kg/m2. Exclusion criteria were: previous surgery, uterine size >12 gestational weeks. The institutional internal review board approval was obtained and all patients included signed an informed consent. Patients received a bowel preparation the day before surgery, with 90 mL of oral sodium phosphate (NaP), to empty the bowel and have a better operatory field view. Antibiotic prophylaxis was performed with cefazoline 2 gr IV, 30 min before surgery.
In both laparoscopic and robotic procedures primary trocar insertion was practiced through direct access technique. In all laparoscopic interventions we used a HD system (Karl Storz H3-Z Full HD Camera Head). In all robotic procedures the da Vinci Si Surgical System (Intuitive Surgical, Inc. Sunnyvale, CA) was used. A 10 mm HD laparoscopic system was used both for laparoscopic and robotic surgery.
To evaluate the level of operative field visualization, a dedicated form has been designed. It was based on the evaluation of four different areas that are mainly involved in the surgical steps of hysterectomy: Douglas space, vesico-uterine fold and, bilaterally, the access to the broad ligament.
All procedures were performed by the same experienced surgeon who judged the degree of visualization of the operative field: a 10-point VAS scale (ten, optimal visualization; zero, no visualization) was used. The maximal visualization was defined as the condition in which the surgeon was able to evaluate entirely the area considered. The evaluation of the surgical field visualization was performed before the placement of any instrument leaving, therefore, the decision on which kind of auxiliary port to use on the needs of the specific intervention.
During the initial inspection, an assistant randomly set the CO2 pressure at 15, 10 and 5 mmHg, and the surgeon, not aware of the CO2 values, was asked to give an evaluation of the four areas of the operative field for each set pressure.
A statistical analysis to compare results at different pressure values within each group has been performed; afterwards results of the two groups were compared. The Mann–Whitney test was used for nonparametric data. Statistical significance was set at a P value of 0.05.
Results
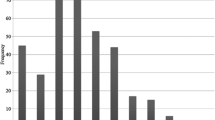
A total of 20 consecutive patients were enrolled in two groups, ten laparoscopic procedures and ten robotic procedures, respectively. Both groups were homogeneous, with no significant difference concerning age (44.2 ± 7.8 in laparoscopy vs. 46.2 ± 8.6 in robotic surgery, p = not significant), BMI (23.7 ± 4.7 in laparoscopy vs. 25.4 ± 4.1 in robotic group, p = not significant). In the laparoscopic group the mean of visualization score, in the four different areas evaluated, were: 9.3 at 15 mmHg; 6.2 at 10 mmHg; 3.4 at 5 mmHg. In robotic group, the mean visualization scores were: 9.4 at 15 mmHg; 8.9 at 10 mmHg; 7.8 at 5 mmHg (Figs. 1, 2).
In the laparoscopic group, the CO2 pressure significantly influenced the surgical field visualization in all four areas analyzed. The surgeon had a good visualization only at 15 mmHg CO2 pressure; visualization decreased with a statistically significant difference from 15 to 5 mmHg (p = 0.0079), 15–10 (p = 0.0211) and 10–5 mmHg (p = 0.0463) (Fig. 1).
In the robotic group, the influence of CO2 pneumoperitoneum pressure on surgical areas visualization was not straightforward; operative field display remained stable at any pressure value with no significant difference. Data at 15 mmHg and 10 mmHg CO2 were similar for all four surgical fields, and differences between pressure values were not statistically significant (p = 0.4585). Surprisingly no statistically significant difference in the visualization of the operative field was observed even at 5 mmHg comparing it either with 15 or 10 mmHg (p = 0.0742 and 0.2909, respectively) (Fig. 2).
The comparison between the level of visualization between the two surgical techniques showed a statistically significant difference in favor of robotic surgery at CO2 pressure values of 5 and 10 mmHg (p < 0.001 for both pressure levels) whereas at pressure values of 15 mmHg the perception of the display field was similar (p = 0.5743) (Fig. 3).
Comment
Robotic surgery is actually one of the fastest growing fields in minimally invasive surgery. In gynecology, robotic surgery is used for all actions executable in laparoscopy, from myomectomy to hysterectomy, from adnexal surgery to colposacropexy, till lymphadenectomy [4]. Although the pathophysiological basis is still not well known, the benefits of robotic surgery over laparoscopy in terms of post-operative recovery have been clinically demonstrated [1, 2]. In particular, it has been demonstrated a lower blood loss, less post-operative pain, faster functional recovery and fewer complications, compared to traditional laparoscopy [5, 6].
The two surgical procedures are technically very similar, both involving the use of the pneumoperitoneum to determine the distension of the abdominal cavity. Although these techniques are considered minimally invasive, the CO2 insufflation is responsible for modification at an ultrastructural level of mesothelial cells, resulting in mesothelial damage [7–9].
The gas flow, dry and with a lower temperature than body’s one (20 °C compared to body’s 36 °C), has an immediate effect on the peritoneal fluid viscosity increase and on the damage of the peritoneal cells, through the effect of evaporation and desiccation [10, 11]. Stress of peritoneal cells, both continuous and intermittent, is repetitive for the entire duration of the surgery, with a cumulative effect that results in a general impairment of the peritoneum [12]. The pneumoperitoneum causes also a transient hypercapnia and respiratory acidosis, which worsens with the use of an intra-abdominal pressure superior to 12–15 mmHg and of the Trendelenburg position [13]; the tissue oxygenation level is indeed an important determinant for adhesions formation, wound healing and tumor growth [14].
Based on the above consideration it is, therefore, fundamental for the surgeon to operate with the lowest intra-abdominal pressure value to reduce the impact of the CO2 pneumoperitoneum on the mesothelial microcirculation, and with the least amount of total CO2 flux to mitigate the cumulative peritoneal damage. The mesothelial damage, therefore, potentially influences the post-operative pain, functional recovery time and time duration of hospital stay.
To our knowledge this is the first study to examine differences between robotics and traditional laparoscopy in terms of visual operative field display in correlation to different intra-abdominal pressure values.
The study highlights that the values of intra-abdominal pressure used to obtain the pneumoperitoneum do not significantly affect the display of the abdomino-pelvic cavity in robotic surgery, differently from laparoscopic procedures. This finding is particularly significant especially at low CO2 pressure (5 mmHg) and it has considerable implications both in terms of intraoperative cardio-circulatory parameters and of peritoneal damage with consequent influence on the post-operative recovery.
Since da Vinci surgical system is equipped with stereoscopic endoscope with high definition image quality, to reduce the possibility that performance of the endoscopes is the main cause of the differences that observed, in all laparoscopic interventions we used a HD system. Considering the latest technological developments, it is common opinion to consider all the top level HD system (both robotic and laparoscopic) as capable of best images in relation of human eye capabilities. Furthermore, the evaluation of the visualization field was mainly based on quantitative (amount of visual space of the surgical field) more than qualitative patterns (image definition).
Some authors report the use of arbitrary CO2 pressures lower than 10 mmHg during robotic surgery, without highlighting the reasons or the importance, demonstrating that this phenomenon is currently being used by robotic surgery operators despite being little known and recently disclosed.
The data reported show that robotic surgery may potentially influence positively the peritoneal environment stress during surgical procedures, and this mechanism could justify the fast post-operative recovery in patients undergoing robotic surgery. The results obtained are likely to be reported to an effect of suspension exerted by the robotic arms on the abdominal wall. This effect is a peculiarity of robotic surgery, which is not present in laparoscopic surgery.
It is evident that high levels of CO2 pressure, required for the correct visualization of the surgical field during laparoscopic procedures, are not necessary during robotic procedures, allowing a proper pelvic structure’s visualization at pressure values as low as 5 mmHg.
Furthermore, considering that it is a pilot study, we have chosen to involve only one surgeon with a high experience in both laparoscopic and robotic procedures to reduce potential biases related to judgement of surgeons with different level of expertise between the two techniques. However, future studies including multiple centers and a higher number of patients are needed to confirm our results. Moreover, considering the results obtained in some studies which have demonstrated the differences between beginner and experienced surgeons in robotic surgery, such as the study by Pluchino et al. [15], it could be interesting to evaluate in future studies differences between skilled and not surgeons in both laparoscopy and robotic approach.
Moreover, as reported by Litta et al. [16], during laparoscopic intervention a safe and effective surgical technique is crucial. This the same even for robotic surgery and it includes even the CO2 pressure standardization according to surgical approach, because surgical technique may affect intraoperative need of pelvic visualization and consequently even the need of CO2 pressure.
In addition, it could be interesting to evaluate in future studies the influence of low CO2 pressure in peculiar cohort of women such as elderly patients affected by some comorbidities and obese women. In fact, as reported in the study by Ciavattini et al. [17], laparoscopic surgery appears feasible and safe in elderly patients regardless of increased comorbidity. Moreover, as reported in the study by Litta et al. [18], laparoscopic surgery is safe and feasible even in obese woman. Thus, in future studies it could be interesting to evaluate the effect of robotic surgery using low CO2 pressure in this peculiar cohort of patients.
Conclusion
The study highlights that the values of intra-abdominal pressure used to obtain the pneumoperitoneum do not significantly affect the display of the abdomino-pelvic cavity in robotic surgery, differently from laparoscopic procedures. This finding is particularly significant especially at low CO2 pressure (5 mmHg) and it has considerable implications both in terms of intraoperative cardio-circulatory parameters and of peritoneal damage with consequent influence on the post-operative recovery.
References
Volz J, Köster S, Weiss M, Schmidt R, Urbaschek R, Melchert F, Albrecht M (1996) Pathophysiologic features of a pneumoperitoneum at laparoscopy: a swine model. Am J Obstet Gynecol 174:132–140
Payne TN, Dauterive FR (2008) A comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in community practice. J Minim Invasive Gynecol. 15(3):286–291
Russell RC (1993) General surgery: biliary surgery. BMJ 307(6914):1266–1269
Bocca S, Stadtmauer L, Oehninger S (2007) Current status of robotically assisted laparoscopic surgery in reproductive medicine and gynaecology. Reprod Biomed Online 6:765–772
Sarlos D, Kots L, Stevanovic N, von Felten S, Schär G (2012) Robotic compared with conventional laparoscopic hysterectomy. Obstet Gynecol 120:604–611
Rosário MT, Ribeiro U Jr, Corbett CE, Ozaki AC, Bresciani CC, Zilberstein B, Gama-Rodrigues JJ (2006) Does CO2 pneumoperitoneum alter the ultra-structure of the mesothelium? J Surg Res 2:84–88
Walsh CA, Walsh SR, Tang TY, Slack M (2009) Total abdominal hysterectomy versus total laparoscopic hysterectomy for benign disease: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 144:3–7
Holmdahl L (2000) The plasmin system, a marker of the propensity to develop adhesions. In: DiZerega G et al (eds) Peritoneal surgery. Springer, New York, pp 117–131
Cevrioglu AS, Yilmaz S, Koken T, Tokyol C, Yilmazer M, Fenkci IV (2004) Comparison of the effects of low intra-abdominal pressure and ischaemic preconditioning on the generation of oxidative stress markers and inflammatory cytokines during laparoscopy in rats. Hum Reprod 9:2144–2151
Ott DE (2003) Desertification of the peritoneum by thin-film evaporation during laparoscopy. JSLS 7:189–195
Sammour T, Kahokehr A, Hill A (2008) Meta-analysis of the effect of warm humidified insufflation on pain after laparoscopy. Br J Surg 95:950–956
Matsuzaki S, Jardon K, Maleysson E, D’Arpiany F, Canis M, Botchorishvili R (2012) Impact of intraperitoneal pressure of a CO2 pneumoperitoneum on the surgical peritoneal environment. Hum Reprod 27:1613–1623
Binda M, Koninckx P (2009) Prevention of adhesions formation in a laparoscopic mouse model should combine local treatment with peritoneal cavity conditioning. Hum Reprod 24:1473–1479
Shashoua AR, Gill D, Locher SR (2009) Robotic-assisted total laparoscopic hysterectomy versus conventional total laparoscopic hysterectomy. JSLS 3:364–369
Pluchino N, Litta P, Freschi L, Russo M, Simi G, Santoro AN, Angioni S, Gadducci A, Cela V (2014) Comparison of the initial surgical experience with robotic and laparoscopic myomectomy. Int J Med Robot 10(2):208–212
Litta P, Saccardi C, Conte L, Florio P (2013) Reverse hysterectomy: another technique for performing a laparoscopic hysterectomy. J Minim Invasive Gynecol 20(5):631–636
Ciavattini A, Di Giuseppe J, Cecchi S, Tsiroglou D, Mancioli F, Stevenazzi G, Tranquilli AL, Litta P (2014) Gynecologic laparoscopy in patients aged 65 or more: feasibility and safety in the presence of increased comorbidity. Eur J Obstet Gynecol Reprod Biol 175:49–53
Litta P, Fabris AM, Breda E, Bartolucci C, Conte L, Saccardi C, Nappi L (2013) Laparoscopic surgical staging of endometrial cancer: does obesity influence feasibility and perioperative outcome? Eur J Gynaecol Oncol 34(3):231–233
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angioli, R., Terranova, C., Plotti, F. et al. Influence of pneumoperitoneum pressure on surgical field during robotic and laparoscopic surgery: a comparative study. Arch Gynecol Obstet 291, 865–868 (2015). https://doi.org/10.1007/s00404-014-3494-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3494-z