Abstract
Vitiligo is an acquired pigmentary skin disorder that currently lacks standardized treatment and validated biomarkers to objectively evaluate disease state or therapeutic response. Although prior studies have linked vitiligo autoimmunity with CXCL10/CXCL9-mediated recruitment of leukocytes to the skin, only limited clinical data are available regarding CXCL10 as vitiligo biomarker. To evaluate the utility of systemic CXCL10 as a predictor of disease progression and treatment response on a large cohort of vitiligo patients. CXCL10 levels in lesional, perilesional, and unaffected skin of vitiligo patient (n = 30) and in the serum (n = 51) were measured by quantitative ELISA. CXCL10 expression, recruitment of leukocytes, and inflammatory infiltrates were evaluated by histochemical (n = 32) and immunofluorescence (n = 10) staining. Rigorous cross-sectional and longitudinal biostatistical analysis were employed to correlate CXCL10 levels with disease variables, treatment response, and outcome. We demonstrated that elevated CXCL10 level (2 pg/mm2 and higher) in lesional skin correlates with increased leukocytic infiltrate, disease duration (< 2 year), and its higher level in the serum (50 pg/ml and higher). Changes in CXCL10 serum levels in patients treated with psoralen plus UVA (PUVA) phototherapy, narrowband UVB (NB-UVB) phototherapy, and systemic steroids (SS) correlated with changes in the intralesional CXCL10 levels in repigmented skin. NB-UVB and SS regimens provided most consistent CXCL10 mean change, suggesting that these regimens are most effective in harnessing CXCR3-mediated inflammatory response. Serum CXCL10 is a useful vitiligo biomarker, which predicts lesional skin leukocytic infiltration, and vitiligo treatment response and outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitiligo is an acquired pigmentary disorder characterized by depigmented or hypo-pigmented patches of the skin and mucous membranes [16]. Although not life threatening, vitiligo often diminishes patients’ quality of life [26]. The etiopathogenesis of vitiligo involves interplay of multiple genetic and environmental factors [14, 22] associated with various molecular mechanisms, including autoimmunity, that lead to destruction of the melanocytes [14]. Analysis of the cutaneous tissue in various autoimmune dermatological afflictions demonstrated an important role of the chemokines in the induction and maintenance of the immune responses. We and others recently demonstrated that CXCL12 and CCL5 may play a substantial role in autoimmune vitiligo [3, 28, 29]. One of the chemokines, CXCL10 (interferon-inducible protein 10 (IP-10)) [20] is considered a key mediator of the interferon (IFN) response and recruitment of CXCR3+ Th1 lymphocytes to sites of inflammation, which could be induced by IFN-α, IFN-β, IFN-γ, and LPS [18].
CXCL10 plays a role in different autoimmune diseases [17]. Elevated CXCL10 levels were associated with vitiligo progression and maintenance of T cell function in vitiligo animal models [27]. It was also reported that higher serum CXCL10 level could be associated with vitiligo activity [2]. However, its role as a reporter of vitiligo progression or as a predictor of treatment response is not fully elucidated. A variety of different non-surgical and surgical approaches are used in clinical practice to stabilize the disease and induce re-pigmentation [23, 24]. Most commonly used are systemic steroids (SS), PUVA, and NB-UVB phototherapy. Although several retrospective and prospective studies have attempted to identify optimal vitiligo treatment modalities, lack of objective evaluative markers besides re-pigmentation did not allow identification of a most effective regimen [4, 7, 36].
In the present study, we conducted cross-sectional and longitudinal analyses of serum and intracutaneous CXCL10 in non-segmental vitiligo patients to define its prognostic value in evaluating vitiligo progression and predicting treatment response.
Materials and methods
Study subjects and treatments
The study was conducted on 54 vitiligo patients (10–60 years old; 24 females, and 31 males) attending the Dermatology clinic, Minia University Hospital, Minia, Egypt; and 6 healthy control volunteers (18–45 years old; 3 females, and 3 males). The study excluded patients with underlying autoimmunity, as elevated CXCL10 serum levels were identified in patients with various autoimmune disorders, including thyroiditis [9]. To evaluate CXCL10 as a biomarker and predictor of vitiligo treatment, six patients were treated with PUVA, eight patients with NB-UVB, and seven with SS, as described previously [5, 13, 21]. All patients, guardians, and healthy volunteers received thorough counseling and provided informed consents. The ethical research committee of Minia University approved this study.
Evaluation of vitiligo stability.
To evaluate disease stability, we used a six-point scale VIDA score as follows:
-
+ 4: Activity of 6 weeks or less;
-
+ 3: Activity of 6 weeks to 3 months;
-
+ 2: Activity of 3–6 months;
-
+ 1: Activity of 6–12 months;
-
0: Stable at least for 1 year;
-
− 1: Stable at least for 1 year with spontaneous re-pigmentation.
For all cases, we considered those with scores ≤ + 1 as stable and those with more than + 1 as active.
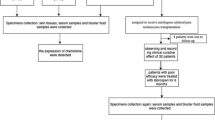
Samples collection and preparation
Whole blood (10 ml) from each patient and control was collected and processed to obtain serum according to a standard protocol [32]. Punch biopsies (3 mm) were obtained from each patient before and after treatment from the edge of the depigmented patch (lesional), nearby normal edge (perilesional) in sun-protected lesions. Acral biopsies were not collected. Unaffected skin samples were collected from sun-protected skin (e.g. buttocks). Control skin biopsies (3 mm) were collected from sun-protected areas. Biopsies were snap-frozen in liquid nitrogen. Each biopsy was cut in half; one half was homogenized in PathScan® Sandwich ELISA Lysis Buffer (Cell Signaling Technology Inc., USA) with Halt™ Protease and Phosphatase Inhibitors (Thermo Fisher Scientific Inc., USA); the other was used for histological and indirect immunofluorescence evaluations.
Enzyme-Linked Immunosorbent Assay (ELISA)
CXCL10 quantitation in skin and serum was done using human-specific CXCL10 ELISA kit (ab83700; Abcam, USA) as described by the manufacturer.
Immunofluorescence analysis
Indirect Immunofluorescence was used according to a standard protocol as described in our prior studies [28]. CXCL10 was detected with CXCL10-specific antibodies (ab9807, Abcam®, USA). CD45RO was detected with monoclonal antibodies (Dako, M0742).
Statistical analyses
Collected data were analyzed using SPSS (Version 15.0, SPSS Inc.; Chicago, IL, USA) and summarized as mean ± SD. Analysis was performed using Mann–Whitney U test, Wilcoxon Signed Ranks test, and one-way analysis of variance (ANOVA). Statistical significance for all results was defined as significant when p ≤ 0.05 and highly significant when p ≤ 0.01.
Biostatistical modeling
CXCL10 levels were analyzed using linear mixed effects (LME) models with random patient effects to allow for correlation between repeated measures (before and after treatment and/or multiple skin locations) from the same patient. Log transformation of the serum CXCL10 levels was used to satisfy the normal distribution assumptions of the model. The initial models included status (before vs. after treatment), duration (< 2 years vs. > 2 years), sex, age, and infiltration status (high, medium, low) as predictors with and without inclusion of serum CXCL10 in the model as a predictor. The final parsimonious model was obtained using backward elimination of insignificant predictors.
The receiver operating characteristic (ROC) curve analysis was performed to investigate whether the serum CXCL10 levels can differentiate between the stable and active disease.
Differences between treatment groups (NB-UVB, PUVA, and SS) were analyzed based on the changes from before to after treatment in log-transformed serum and skin CXCL10 levels using the ANOVA model and considering duration, sex, age, and infiltration status as predictors. The data were analyzed in R (R Core Team [2015]. R: A language and environment for statistical computing. Vienna, Austria. http://www.R-project.org).
Results
Cutaneous CXCL10 levels significantly correlated with the degree of leukocytic infiltrates in vitiligo lesional skin
Recent studies suggested that blister suction could be used to evaluate these chemokines and T cell infiltrates in vitiliginous skin [30]. To test whether such evaluation could be done using patient blood samples and to define CXCL10 as a predictor of vitiligo variables and response to treatment, we conducted cross-sectional and longitudinal studies on a large cohort of vitiligo patients. First, we assessed dermal inflammation and CXCL10 levels in biopsies collected from lesional, perilesional, and unaffected skin of 34 patients. Independent blind dematopathological evaluation of biopsy sections collected from lesional, perilesional, and unaffected skin detected high, medium, or low leukocytic infiltrates in all three locations in 14%, 20%, and 31% of patients, respectively (Fig. 1a, Fig. S1). In the remaining 35% of patients, substantially higher infiltrates were noted in lesional and perilesional skin as compared to unaffected skin (Fig. 1a). Samples with higher infiltrates were characterized by a higher CXCL10 expression at the basal layer of the epidermis (Fig. 1b) and a greater number of CD45RO+-activated T cells (Fig. 1c). Histological evaluation also consistently showed a higher degree of inflammation in the skin of early (< 2 years) vitiligo lesions (Fig. 1 d). Based on quantitative ELISA, the highest CXCL10 levels, ranging between 3.2 and 4.1 ng per ¼ of the 3 mm punch biopsy (1.7 mm2), were detected in lesional skin with the highest degree of infiltration. The lowest levels, ranging between 0.5 and 0.9 ng per 1.7 mm2, were in the unaffected skin. The differences in CXCL10 levels correlated significantly with the densities of inflammatory infiltrates and disease duration (< 2 years) (Fig. 2a, b). To evaluate CXCL10 as a predictor, we assessed association of its levels in different locations with multiple parameters (duration of the disease, age, sex, and infiltration status) using LME biostatistical modeling. This modeling confirmed that the mean lesional skin CXCL10 was higher in vitiligo patients by 2.0 (p < 0.001), as compared to controls. It was associated with high leukocytic infiltration by 0.98, as compared to medium (p < 0.001) and by 1.15 as compared to low infiltration (p < 0.001) (Table 1a). For perilesional skin, the lower CXCL10 was associated with low infiltration by 0.47 (p = 0.023) as compared to medium infiltration and by 0.49 (95% CI − 0.06, 1.03, p = 0.076) as compared to high infiltration. Association of the intracutaneous CXCL10 levels with patients’ age, sex, and disease duration was not significant (data not shown).
Analysis of the intracutaneous CXCL10 and inflammation. a Histochemical analysis (H&E staining) of the infiltration of the vitiligo lesional, perilesional, and remote skin showing presence of high, medium, and low inflammation in these locations. b Histochemical and indirect immunofluorescence (IF) analyses show lower CXCL10 levels in skin with lower inflammation and higher lesional and perilesional CXCL10 levels in the skin with higher inflammation. c Indirect immunofluorescence depicts higher vitiliginous skin infiltration with CD45RO activated T cells in regions with higher CXCL10 levels. (d) H&E staining illustrates higher infiltrate in the skin of early (< 2 year) vitiligo. In all IF panels, detected antigens are shown in respective colors. In a, b, d Scale bar—100 µm, in c 200 µm
Quantitative and biostatistical analyses of intracutaneous and systemic CXCL10. a–c ELISA-based quantitation of the intracutaneous (a, b) and systemic (b) CXCL10 shows correlation of the chemokine levels with (a) lesional, perilesional and remote locations as well as with inflammatory status (as indicated in the key) and with (b) disease duration and patient sex. c CXCL10 levels in the systemic compartment and their correlation with disease activity, duration, sex, and infiltrate (as indicated in the keys). d The trend lines for regressions of skin CXCL10 levels in three different locations (as indicated in the key) on serum CXCL10 levels corresponding to the estimates reported in Table S2. e Box-and-whisker plots illustrate differences in serum level by infiltration status (high (H), medium (M), low (L)) as reported in Table 1. f, g illustrate correlation of the CXCL10 serum levels with vitiligo stability. f ROC shows curve analysis for prediction of stable vs. active disease using the serum CXCL10 level; g Box-and-whisker plot show that range of serum CXCL10 levels in stable disease overlap with the range in active disease
Serum CXCL10 predicts its levels in lesional and perilesional skin
ELISA-based CXCL10 quantitation in a total of 51 vitiligo and 6 control samples showed an overall higher level of the chemokine in the serum of patients (89.2 pg/mL)Footnote 1 than in controls (35 pg/mL) (p = 0.003) (Fig. 2c) and in patients with active disease (97.7 pg/mL) than in patients with a stable disease (49.2 pg/mL). Patients with vitiligo lasting less than 2 years also had higher serum CXCL10 (106.2 pg/mL) than in patients with vitiligo for more than 2 years (77.2 pg/mL) (Fig. 2c). Some difference was also observed between male (75.5 pg/mL) and female (108.7 pg/mL) patients. CXCL10 serum levels in lesional skin were the highest (195 pg/ml) in patients with high leukocytic infiltrate (Fig. 2c). Correlation of serum CXCL10 with different disease variables using LME models validated serum CXCL10 as predictive of the lesional and perilesional levels of the chemokine (p < 0.001) (Table S2) and the density of the inflammatory infiltrates (Fig. 2e, Table 1b). Trend lines further demonstrated that serum CXCL10 is predictive of lesional and perilesional CXCL10 at 50 pg/ml and higher concentrations (Fig. 2d).
Correlation of serum CXCL10 with vitiligo activity (active vs. stable) showed that serum CXCL10 levels are lower by 0.45 (p = 0.019) in healthy volunteers as compared to patients with active disease, and are lower by 0.43 (p = 0.004) in patients with stable disease as compared to patients with active disease (Table 1b). Receiver operating characteristic (ROC) curve analysis estimated that area under the curve (AUC) was 0.69 (95% CI 0.56, 0.82) (Fig. 2f). A plotted range of serum CXCL10 showed substantial variations in the level of the chemokine in patients with active disease (Fig. 2g). No correlations between serum CXCL10 and patient’s sex, age, and disease duration were identified (data not shown).
Changes in serum CXCL10 reflect changes in lesional CXCL10 and inflammatory infiltrates and correlate with response of NB-UVB, PUVA and corticosteroid treatments
PUVA, NB-UVB, and SS are commonly used to treat vitiligo and induce re-pigmentation. Here, we evaluated whether these regimens alter intracutaneous and systemic CXCL10 levels by treating 21 non-segmental vitiligo (NSV) patients with PUVA, NB-UVB, and SS (oral prednisolone) as described previously [5, 13, 21]. All regimens showed clinical improvement after 3 months of therapy as defined by marginal re-pigmentation, patch circumference reduction, follicular re-pigmentation, or closure of small macules (Fig. S2). Immunofluorescence analysis of biopsies showed that all treatments led to substantial CXCL10 reduction in lesional and perilesional skin (Fig. 3a, b). No substantial changes in CXCL10 were observed in unaffected skin (Fig. 3b).
Analysis of the intracutaneous and serum CXCL10 before and after treatments. a Immunofluorescence analysis of CXCL10 expression in lesional, perilesional, and remote skin of vitiligo patients before and after 3 months of treatment with PUVA, NB-UVB, and SS (as indicated in the panel). Green – CXCL10; Blue – DAPI nuclear staining. Scale bar 200 µm. b Quantitation of CXCL10-associated fluorescence in lesional, perilesional and remote skin after PUVA, NB-UVB and SS treatments (as indicated). Data are presented as a mean grey value of five random field measurements ± SD. c Column plots illustrate ELISA-based quantitation showing reduced intracutaneous CXCL10 levels in lesional and perilesional skin after treatments and no change in CXCL10 levels in the remote skin of vitiligo patients, as indicated. Statistical significance (p value) is shown above the columns. d Column plots illustrate decreased CXCL10 levels in the serum of vitiligo patients after treatments (as indicated). On (b–d), data are presented as average CXCL10 concentration (pg/ml) ± SD. Statistical significance (p value) and treatments are shown on the plots. Status (before and after treatment) is depicted on the key
When CXCL10 levels were measured in lysates of 132 skin samples from 21 patients before and after treatment by quantitative ELISA, with samples from healthy volunteers as controls, there was no difference between patients’ remote skin and controls (p > 0.05) (Fig. 3c). All regimens led to a significant reduction of CXCL10 levels in lesional and perilesional skin (Fig. 3d). No significant differences between the means of intracutaneous CXCL10 levels were observed when treatment groups were compared to each other before and after treatments (Fig. 3c, Table S3); however, changes in the lesional CXCL10 after treatment correlated with reduction of serum CXCL10 (Fig. 3d; Table S4). The LME modeling confirmed that higher CXCL10 levels in lesional skin is associated with “before treatment” status as compared to “after treatment” (p < 0.001), and lower CXCL10 levels in perilesional skin were associated with “after treatment” status as compared to “before treatment” (p < 0.001) (Table 2a). Analysis of differences between treatment groups (NB-UVB, PUVA, and SS) showed that the highest mean change was associated with NB-UVB treatment (p = 0.032) as compared to PUVA, whereas SS treatment provided most consistent negative change in CXCL10 levels in lesional and perilesional skin. Other differences between treatment groups were not significant (Fig. 4a; Table 2b). The higher mean change in CXCL10 levels in lesional skin was also associated with change in the inflammatory infiltrates from high to low (Table 2c). Different treatments in perilesional skin evidenced no significant differences pre-to-post treatment (Fig. 4a; Table 2b).
Evaluation of changes in intracutaneous and serum CXCL10 after treatment. a Box-and-whisker plots illustrating changes in intracutaneous CXCL10 levels after NB-UVB, PUVA, and SS treatments, with whiskers indicating variability outside the upper and lower quartiles. Change in lesional, perilesional, and remote skin are evaluated separately. Dotted line corresponds to no change in CXCL10 levels. b Dot plot illustrating Pearson correlation between CXCL10 serum and skin levels in vitiligo patients before and after treatment, as indicated. Correlation was done separately for lesional, perilesional, and remote skin, as indicated in the key. c Box-and-whisker plots illustrating changes in serum CXCL10 levels (untransformed or log-transformed, as indicated) after NB-UVB, PUVA, and SS treatments. Data is presented as a mean change ± SD. Dotted line corresponds to no change in CXCL10 levels. d Box-and-whisker plots illustrating changes in re-pigmentation in differently treated patients (as indicated). Data is presented as an interquartile range (middle 50% of values) with the highest and lowest observations (whiskers)
Using Pearson correlation, initial biostatistical evaluation of serum and intracutaneous CXCL10 levels points to a positive association between serum and lesional/perilesional skin CXCL10 before and after treatment (Fig. 4b, Table S5). The differences between the NB-UVB, PUVA, and SS treatments were not significant for the changes in serum CXCL10 levels (log-transformed or not) from before to after treatment. The ranges of changes in serum CXCL10 levels largely overlapped for all treatment groups (Fig. 4c). Nevertheless, the higher mean change in serum CXCL10 levels was observed in patients treated with NB-UVB. Evaluation of skin re-pigmentation in differently treated patients confirmed that greatest re-pigmentation was observed in SS-treated patients, whereas the most consistent re-pigmentation was in patients treated with NB-UVB. PUVA therapy although providing up to 50% of re-pigmentation in some patient, was less effective (Fig. 4d). These findings are in agreement with treatment-dependent changes in serum CXCL10 levels (Fig. 4c). Collectively, these analyses demonstrated that all tested regimens led to re-pigmentation and reduction of the CXCL10 in lesional skin and serum. Biostatistical evaluation showed that changes in serum CXCL10 reflect changes in lesional CXCL10 and inflammatory infiltrates. More importantly, our data confirmed that serum CXCL10 could be used as a predictor of treatment response and outcome.
Discussion
To date, an accumulating body of evidence supports the role of Th1 cell system and chemokines in vitiligo progression. CXCR3 and its ligands, CXCL9 and CXCL10, were considered the most relevant chemotactic axes promoting migration of activated T cells [15, 19]. These chemokines were linked with progression of depigmentation in vitiligo mouse model [27, 33]. Using blister suction technique, recent studies on a small number of patients also showed that accumulation of CXCL9 in blister fluids correlates with CD8 T cell infiltrates [30].
Our study provides compelling evidence that serum CXCL10 at 50 pg/ml and higher levels is predictive of lesional CXCL10 and leukocytic infiltrates. These findings suggest that measuring blood CXCL10 level by ELISA can be used instead of blister suction-based evaluation in clinical settings. Although minimally invasive, blister suction introduces inflammatory response to mechanical damage and could lead to the recruitment of melanocyte-specific T cells and autoimmune reaction.
Assessment of vitiligo stability is critical for planning vitiligo treatment regimens. However, there is no consensus regarding serological, biochemical, and molecular parameters that define stability. A recent report suggested that systemic CXCL10 levels could distinguish between active and stable disease [2]. However, our data showing the intermediate value of the AUC and the overlap of the serum CXCL10 range in stable and active disease (Fig. 2e, f) suggest that the exact cutoff for serum CXCL10 levels could not be easily identified to differentiate well between stable and active vitiligo. Our findings agree with another recent study conducted on a very small cohort of patients [30]. The discrepancy in findings among studies may arise from differences in clinical evaluation of vitiligo stability and from greater variations in serum CXCL10 levels in patients with active disease. Taken together, our data suggest that substantially larger, multinational studies are required to determine the utility of serum CXCL10 or other chemokines (e.g. CXCL9) in defining vitiligo stability.
To date, vitiligo lacks universal treatment regimens. Of multiple treatments, PUVA, NB-UVB, and SS are most commonly used to induce re-pigmentation of the vitiliginous skin. The molecular mechanisms supporting therapeutic action of these treatments remain incompletely understood. Considering the important role of CXCL10 in T cell-mediated cutaneous autoimmunity in lichen sclerosus and vitiligo [27, 35], we suggest that re-pigmentation of vitiligo lesions could be associated with down-modulation of CXCL10. In support of this notion, prior studies showed somewhat reduced levels of CXCL10 in the serum of vitiligo patients after intramuscular diprospan/topical tacrolimus treatment [34]. In our randomized longitudinal study, all three tested regimens (PUVA, NB-UVB, SS) showed a substantial clinical response after 3 months of therapy and coincided with significant reduction of lesional and perilesional CXCL10 levels. Of multiple parameters used in LME models, including disease duration, sex, age, and infiltration, only status “before vs. after treatment” and infiltration were significantly associated with changes observed in the intracutaneous CXCL10. These findings clearly demonstrated that the therapeutic effect of PUVA, NB-UVB, SS is related to the reduction of lesional chemokine and that NB-UVB provided the highest and SS the most consistent change in the intracutaneous and systemic CXCL10 levels. Although in several cases, PUVA therapy effectively reduced lesional CXCL10, these findings suggest that NB-UVB and SS are more effective in harnessing detrimental CXCL10 effects.
The exact molecular mechanisms by which PUVA, NB-UVB, and SS alter CXCL10 levels are not well defined. CXCL10 transcription is known to be regulated by IFNγ, which induces transcription of downstream genes through activation of STAT-1 and NF-kB transcription factors [1, 25]. In some cells, elevated CXCL10 levels may, in turn, activate NF-kB and create an autonomous loop [12]. Because SS such as prednisone inhibit inflammation via inhibition of NF-κB activation [37], SS regimen likely downregulates intracutaneous CXCL10 via blocking of the NF-kB-mediated pathway. The mechanisms of PUVA and NB-UVB-mediated CXCL10 inhibition are less obvious. As UVB primarily affects epidermis and superficial dermis, whereas UVA affects deeper recesses of dermis, it is likely that different mediators could be involved in CXCL10 regulation. It is plausible that NB-UVB induces intracutaneous IL-10 in the upper layers of the skin [31], which subsequently inhibits NF-kB transcriptional activity [8] leading to down-modulation of CXCL10. This mechanism could explain a more consistent decrease of the cutaneous CXCL10 after NB-UVB as compared to PUVA (Fig. 2).
Prior studies demonstrated that CXCR3 receptor for CXCL10 is expressed on various leukocytes, including vitiligo-associated skin resident memory CD8+ CTL [6], circulating CD4+ and CD8+ T cells [34], and NK cells [10]. Considering these findings, our data suggest that therapeutic efficacy of tested regimens could result from CXCL10-dependent inhibition of leukocyte recruitment. Divergent roles of CXCR3 isoforms in non-leukocytic cells such as melanoma [11] and, possibly, melanocytes also suggest that PUVA, NB-UVB, and SS could affect other processes involved in re-pigmentation. Regardless of CXCL10 down-modulation and re-pigmentation mechanisms, our studies confirm that serum CXCL10 levels could serve as an objective tool to assess vitiligo treatment response and even predict the outcome.
Collectively, our comprehensive analysis and biostatistical modeling demonstrated that CXCL10 serum levels could predict CXCL10 levels in vitiligo lesional and perilesional skin and inflammatory infiltrates in the lesional skin; it further demonstrated that ELISA-based assessment of systemic CXCL10 could be implemented in clinical practice to assess objectively vitiligo treatment response and outcome.
Notes
Average concentrations are provided in parentheses.
References
Aaronson DS, Horvath CM (2002) A road map for those who don’t know JAK-STAT. Science 296:1653–1655. https://doi.org/10.1126/science.1071545
Abdallah M, El-Mofty M, Anbar T, Rasheed H, Esmat S, Al-Tawdy A, Fawzy MM, Abdel-Halim D, Hegazy R, Gawdat H, Bassiouny D, Ibrahim MA, Sany I, El-Bassiouny M, Khalil M, Abdel-Aziz A, El Maadawi ZM, Mostafa WZ (2018) CXCL-10 and Interleukin-6 are reliable serum markers for vitiligo activity: a multicenter cross-sectional study. Pigment Cell Melanoma Res 31:330–336. https://doi.org/10.1111/pcmr.12667
Alexeev V (2017) CXCL12 as a predictor of vitiligo activity and disease progression. J Invest Dermatol 137:1588–1590. https://doi.org/10.1016/j.jid.2017.03.020
Alhowaish AK, Dietrich N, Onder M, Fritz K (2013) Effectiveness of a 308-nm excimer laser in treatment of vitiligo: a review. Lasers Med Sci 28:1035–1041. https://doi.org/10.1007/s10103-012-1185-1
Anbar TS, Westerhof W, Abdel-Rahman AT, El-Khayyat MA (2006) Evaluation of the effects of NB-UVB in both segmental and non-segmental vitiligo affecting different body sites. Photodermatol Photoimmunol Photomed 22:157–163. https://doi.org/10.1111/j.1600-0781.2006.00222.x
Boniface K, Jacquemin C, Darrigade AS, Dessarthe B, Martins C, Boukhedouni N, Vernisse C, Grasseau A, Thiolat D, Rambert J, Lucchese F, Bertolotti A, Ezzedine K, Taieb A, Seneschal J (2018) Vitiligo Skin Is Imprinted with Resident Memory CD8 T Cells Expressing CXCR3. J Invest Dermatol 138:355–364. https://doi.org/10.1016/j.jid.2017.08.038
de Menezes AF, Oliveira de Carvalho F, Barreto RS, de Santana SB, Shanmugam S, Gurgel RQ, de Souza Araujo AA (2017) Pharmacologic treatment of vitiligo in children and adolescents: a systematic review. Pediatr Dermatol 34:13–24. https://doi.org/10.1111/pde.13024
Driessler F, Venstrom K, Sabat R, Asadullah K, Schottelius AJ (2004) Molecular mechanisms of interleukin-10-mediated inhibition of NF-kappaB activity: a role for p50. Clin Exp Immunol 135:64–73. https://doi.org/10.1111/j.1365-2249.2004.02342.x
Ferrari SM, Fallahi P, Santaguida G, Virili C, Ruffilli I, Ragusa F, Centanni M, Antonelli A (2017) Circulating CXCL10 is increased in non-segmental vitiligo, in presence or absence of autoimmune thyroiditis. Autoimmun Rev 16:946–950. https://doi.org/10.1016/j.autrev.2017.07.006
Halder RM, Walters CS, Johnson BA, Chakrabarti SG, Kenney JA Jr (1986) Aberrations in T lymphocytes and natural killer cells in vitiligo: a flow cytometric study. J Am Acad Dermatol 14:733–737. https://doi.org/10.1016/s0190-9622(86)70085-6
Jenkins MH, Brinckerhoff CE, Mullins DW (2015) CXCR3 signaling in BRAFWT melanoma increases IL-8 expression and tumorigenicity. PLoS ONE 10:e0121140. https://doi.org/10.1371/journal.pone.0121140
Jin WJ, Kim B, Kim D, Park Choo HY, Kim HH, Ha H, Lee ZH (2017) NF-kappaB signaling regulates cell-autonomous regulation of CXCL10 in breast cancer 4T1 cells. Exp Mol Med 49:e295. https://doi.org/10.1038/emm.2016.148
Kim SM, Lee HS, Hann SK (1999) The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patients. Int J Dermatol 38:546–550. https://doi.org/10.1046/j.1365-4362.1999.00623.x
Kundu RV, Mhlaba JM, Rangel SM, Le Poole IC (2018) The convergence theory for vitiligo: a reappraisal. Exp Dermatol. https://doi.org/10.1111/exd.13677
Lacotte S, Brun S, Muller S, Dumortier H (2009) CXCR3, inflammation, and autoimmune diseases. Ann N Y Acad Sci 1173:310–317. https://doi.org/10.1111/j.1749-6632.2009.04813.x
Le Poole C, Boissy RE (1997) Vitiligo. Semin Cutan Med Surg 16:3–14. https://doi.org/10.1016/s1085-5629(97)80030-2
Lee EY, Lee ZH, Song YW (2009) CXCL10 and autoimmune diseases. Autoimmun Rev 8:379–383. https://doi.org/10.1016/j.autrev.2008.12.002
Loetscher M, Loetscher P, Brass N, Meese E, Moser B (1998) Lymphocyte-specific chemokine receptor CXCR3: regulation, chemokine binding and gene localization. Eur J Immunol 28:3696–3705. https://doi.org/10.1002/(sici)1521-4141(199811)28:11%3C3696::aid-immu3696%3E3.0.co;2-w
Lonsdorf AS, Hwang ST, Enk AH (2009) Chemokine receptors in T-cell-mediated diseases of the skin. J Invest Dermatol 129:2552–2566. https://doi.org/10.1038/jid.2009.122
Luster AD, Unkeless JC, Ravetch JV (1985) Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature 315:672–676. https://doi.org/10.1038/315672a0
Mofty ME, Zaher H, Esmat S, Youssef R, Shahin Z, Bassioni D, Enani GE (2001) PUVA and PUVB in vitiligo–are they equally effective? Photodermatol Photoimmunol Photomed 17:159–163. https://doi.org/10.1034/j.1600-0781.2001.170403.x
Mohammed GF, Gomaa AH, Al-Dhubaibi MS (2015) Highlights in pathogenesis of vitiligo. World J Clin Cases 3:221–230. https://doi.org/10.12998/wjcc.v3.i3.221
Nordlund JJ (2017) The Medical Treatment of Vitiligo: An Historical Review. Dermatol Clin 35:107–116. https://doi.org/10.1016/j.det.2016.11.001
Patel NS, Paghdal KV, Cohen GF (2012) Advanced treatment modalities for vitiligo. Dermatol Surg 38:381–391. https://doi.org/10.1111/j.1524-4725.2011.02234.x
Pfeffer LM (2011) The role of nuclear factor kappaB in the interferon response. J Interferon Cytokine Res 31:553–559. https://doi.org/10.1089/jir.2011.0028
Radtke MA, Schafer I, Gajur A, Langenbruch A, Augustin M (2009) Willingness-to-pay and quality of life in patients with vitiligo. Br J Dermatol 161:134–139. https://doi.org/10.1111/j.1365-2133.2009.09091.x
Rashighi M, Agarwal P, Richmond JM, Harris TH, Dresser K, Su MW, Zhou Y, Deng A, Hunter CA, Luster AD, Harris JE (2014) CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci Transl Med 6:223ra223. https://doi.org/10.1126/scitranslmed.3007811
Rezk AF, Kemp DM, El-Domyati M, El-Din WH, Lee JB, Uitto J, Igoucheva O, Alexeev V (2017) Misbalanced CXCL12 and CCL5 chemotactic signals in vitiligo onset and progression. J Invest Dermatol 137:1126–1134. https://doi.org/10.1016/j.jid.2016.12.028
Speeckaert R, Ongenae K, van Geel N (2017) Alterations of CXCL12 in serum of patients with vitiligo. J Invest Dermatol 137:1586–1588. https://doi.org/10.1016/j.jid.2017.02.012
Strassner JP, Rashighi M, Ahmed Refat M, Richmond JM, Harris JE (2017) Suction blistering the lesional skin of vitiligo patients reveals useful biomarkers of disease activity. J Am Acad Dermatol 76(847–855):e845. https://doi.org/10.1016/j.jaad.2016.12.021
Tembhre MK, Sharma VK, Sharma A, Chattopadhyay P, Gupta S (2013) T helper and regulatory T cell cytokine profile in active, stable and narrow band ultraviolet B treated generalized vitiligo. Int J Clin Chem 424:27–32. https://doi.org/10.1016/j.cca.2013.05.005
Tuck MK, Chan DW, Chia D, Godwin AK, Grizzle WE, Krueger KE, Rom W, Sanda M, Sorbara L, Stass S, Wang W, Brenner DE (2009) Standard operating procedures for serum and plasma collection: early detection research network consensus statement standard operating procedure integration working group. J Proteome Res 8:113–117. https://doi.org/10.1021/pr800545q
Van Raemdonck K, Van den Steen PE, Liekens S, Van Damme J, Struyf S (2015) CXCR3 ligands in disease and therapy. Cytokine Growth Factor Rev 26:311–327. https://doi.org/10.1016/j.cytogfr.2014.11.009
Wang XX, Wang QQ, Wu JQ, Jiang M, Chen L, Zhang CF, Xiang LH (2016) Increased expression of CXCR3 and its ligands in patients with vitiligo and CXCL10 as a potential clinical marker for vitiligo. Br J Dermatol 174:1318–1326. https://doi.org/10.1111/bjd.14416
Wenzel J, Wiechert A, Merkel C, Bieber T, Tuting T (2007) IP10/CXCL10 - CXCR3 interaction: a potential self-recruiting mechanism for cytotoxic lymphocytes in lichen sclerosus et atrophicus. Acta Derm Venereol 87:112–117. https://doi.org/10.2340/00015555-0194
Xiao BH, Wu Y, Sun Y, Chen HD, Gao XH (2015) Treatment of vitiligo with NB-UVB: a systematic review. J Dermatolog Treat 26:340–346. https://doi.org/10.3109/09546634.2014.952610
Yamamoto Y, Gaynor RB (2001) Therapeutic potential of inhibition of the NF-kappaB pathway in the treatment of inflammation and cancer. J Clin Investig 107:135–142. https://doi.org/10.1172/jci11914
Acknowledgements
These studies were supported in part by the Cultural and Educational Bureau of the Republic of Egypt and Egyptian Scholar Program for AFR and by the Jefferson Institute of Molecular Medicine, Department of Dermatology and Cutaneous Biology, Thomas Jefferson University for VA.
Funding
This work was supported in part by the Cultural and Educational Bureau of the Republic of Egypt for AFR and by the Jefferson Institute of Molecular Medicine, Thomas Jefferson University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
El-Domyati, M., El-Din, W.H., Rezk, A.F. et al. Systemic CXCL10 is a predictive biomarker of vitiligo lesional skin infiltration, PUVA, NB-UVB and corticosteroid treatment response and outcome. Arch Dermatol Res 314, 275–284 (2022). https://doi.org/10.1007/s00403-021-02228-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-021-02228-9