Abstract
Psoriasis is now recognized as an immune-mediated inflammatory dermatosis with increased risk for metabolic syndrome, its individual components, and cardiovascular disease. We quantitatively estimated malondialdehyde (MDA), lipoprotein-a (LP-a), lipoprotein ratios, comprehensive lipid tetrad index (CLTI), and atherogenic index (AI), and evaluated cardiovascular risk in 132 (M:F 94:38) patients with psoriasis aged 20–79 years with chronic plaque psoriasis and equal number of age and gender-matched controls. Lipoprotein ratios, CLTI and AI were calculated using standard formulae. Cardiovascular 10-year risk was graded by Framingham risk score (FRS) as low, intermediate and severe. Mild-to-moderate and severe psoriasis was present in 125 (94.7%), and 7 (5.3%) patients, respectively, and 19 (14.39%) patients had psoriatic arthritis. Statistically significant differences were noted for LDL, LDL/HDL, non-HDL/HDL, MDA, LP-a, AI and CLTI. There was a significantly positive correlation between PASI with LP-a (p = 0.003, r = 0.25) and AI (p = 0.012, r = 0.22). Serum levels of MDA correlated positively with LP-a (p < 0.001, r = 0.55), AI (p < 0.001, r = 0.51) and CLTI (p = 0.006, r = 0.24). FRS was low, intermediate and severe in 78%, 18.9%, and 3% patients compared to 85.6%, 13.6%, and 0.8% controls, respectively, and the difference was not statistically significant. Psoriasis appears to be an independent risk factor for elevated serum MDA, LP-a, CLTI and AI. However, whether they can be used as surrogate markers for enhanced cardiovascular risk in patients with psoriasis, remains conjectural.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genetic, metabolic and immunologic factors have been implicated frequently in etiopathogenesis of psoriasis. Immunologically mediated activation of T lymphocytes and their interaction with other inflammatory cells, cytokines, chemokines and growth factors is central to the inflammation in the dermal microenvironment while epidermal hyperproliferation occurs secondary to the inflammatory events that follow a Th1 type of immune response in psoriasis. This further strengthens our current thinking of psoriasis being an associate of systemic inflammation rather than an exclusive cutaneous disease sharing genetic pathways, common immune mechanisms, treatment-related toxicities, associated psychological stress, and a higher prevalence of cardiovascular risk. The chronic Th1 inflammation and elevated levels of inflammatory cells and several cytokines particularly TNF-α have been implicated for increased reactive oxygen species and oxidative stress and enhanced risk of developing other diseases such as obesity, metabolic syndrome, dyslipidemia, insulin resistance, endothelial dysfunction, formation of atherosclerotic plaque, and cardiovascular disease among psoriatics [7, 27, 36, 37].
Psoriasis is associated with an atherogenic lipid profile and significant lipid abnormalities have been noted even during 5 years preceding onset of psoriasis [1]. Male gender, smoking and moderate-to-high peripheral joint inflammation have been associated with high total cholesterol and triglyceride levels [23, 32]. However, these lipid abnormalities were independent of psoriasis severity and persisted despite tremendous improvement in PASI after ustekinumab therapy in a study [23]. The disturbances in lipid metabolism particularly low-density lipoprotein (LDL) oxidation induce monocyte infiltration and smooth muscle proliferation favoring atherosclerotic plaque formation and predispose to atherosclerosis [12]. On the other hand, HDL is involved in reverse cholesterol transport, inhibition of monocytic infiltration and thus suppression of atherogenicity. An imbalance between generation and removal of reactive oxygen species (ROS) produced from keratinocytes, reactive neutrophilic infiltrate and fibroblasts cause activation of neutrophils in early and active lesions of psoriasis. This further leads to their increased generation, causing self-perpetuating inflammation and oxidative stress that is responsible for TNF-α-induced signaling pathway activation and epidermal hyperproliferation [3, 14, 15]. Malondialdehyde (MDA) produced from ROS-induced oxidation of polyunsaturated fatty acids is an indirect marker of oxidative stress and lipid peroxidation, and increased levels have been observed in tissues, red blood cells and serum in psoriasis patients [5, 17, 20, 38]. Lipoprotein-a, a genetic variant of LDL with apolipoprotein B100 linked to apolipoprotein-a by a disulfide bond, is also susceptible to lipid peroxidation and is said to have both thrombogenic and atherogenic roles. It has evolved as a genetically linked risk factor in development of atherosclerotic plaque and cardiovascular disease particularly in atherosclerosis-prone population [6, 24]. Significantly raised levels of lipoprotein-a with or without high LDL:HDL ratio have been reported in diabetics as well as in psoriasis patients [10, 22, 26, 35]. However, lipid tetrad index, lipid pentad index and atherogenic index (AI), the recently described forms of lipid profile assessment, have emerged as novel and stronger predictors of coronary artery disease/cardiovascular risk compared to other risk factors and lipid parameters [8, 19, 29, 30, 34, 36]. Comprehensive lipid tetrad index (CLTI) magnifies the subtle abnormalities of the various atherogenic and anti-atherogenic lipoproteins, whereas AI is a good indicator of the balance of pro- and anti-inflammatory forces. We evaluated these markers of atherogenesis and cardiovascular disease in patients with psoriasis and controls.
Materials and methods
The study comprised 132 (males 94 and females 38) patients aged ≥ 20 years having chronic plaque psoriasis for at least 6 months at the time of presentation between April 2016 and March 2017. An equal number of age and gender-matched adult volunteers were enrolled as controls. The study was approved by Institutional Protocol Review Board and Ethics Committee (Rgn no ECR/490/Inst/HP/2013/RR-16).
Patients on any anti-psoriasis treatment were given a wash off period of 4 weeks prior to sampling. Only topical bland emollients and oral cetirizine (10 mg/day) were allowed. Patients with preexisting diabetes mellitus, hypertension, hepato-renal disease, obesity (body mass index > 30 kg/m2), collagen vascular disorders, malignancy, pregnant and lactating women and patients on systemic treatment with lipid-lowering drugs, retinoids, corticosteroids, or other immunomodulators were excluded from study. Demographic profile, personal and family history, medical history and clinical details of psoriasis and other systemic diseases were recorded after informed consent. The severity of psoriasis was assessed as mild-to-moderate (PASI ≤ 10) or severe (PASI > 10). Psoriatic arthritis was diagnosed as per the criteria given by Moll and Wright [13] and classified as distal interphalangeal joint arthritis, asymmetrical mono/oligoarthritis, symmetrical polyarthritis, axial arthritis, and arthritis mutilans. All the patients and controls were screened for obesity, diabetes mellitus, hypertension, dyslipidemia (metabolic syndrome), and cardiovascular disorders. They were subjected to measurement of height, weight, waist and hip ratio, body mass index (BMI = weight in kg/height in m2), blood pressure (supine), and electrocardiogram (ECG). Metabolic syndrome was diagnosed as per AHA/NHLBI definition 2005 and WHO-WPR 2000 criteria for Asians was used for defining obesity [11, 41]. Diabetes mellitus was diagnosed according to American Diabetes Association criteria [2]. Hypertension was defined as systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg when recorded on two occasions.
Blood samples (5 ml) were collected after overnight fasting between 0800 and 1000 h by antecubital venepuncture for biochemical analysis in institutional central research laboratory. Quantitative estimation for lipid profile was done using fully automated analyzer XL-300. Serum cholesterol and triglyceride levels were estimated using spectrophotometry. HDL and LDL cholesterol were estimated using immunoinhibition method. Quantitative estimation of serum malondialdehyde and serum lipoprotein-a was performed using double antibody sandwich enzyme-linked immunosorbent one-step process assay (ELISA) using ready to use in vitro kits as per manufacturer’s protocol (Shanghai Qayee Biotechnology Co., Ltd.). Lipoprotein ratios, CLTI and AI were computed using standard formulae.
Framingham risk (FR) score for cardiovascular risk assessment was calculated in all study subjects using standard formula [9, 40]. The FR score predicts a person’s chance of having a heart attack in the next 10 years. This tool is designed for adults aged 20 years and older who do not have heart disease or diabetes. Although not the ideal tool for calculating cardiovascular risk in Indians, it was used in the absence of similar or any other established standard scoring system for cardiovascular risk in the atherosclerosis.
Statistical analysis
Results obtained were tabulated and analyzed statistically. Statistical analysis was performed using IBM SPSS statistics version 17.0 (Armonk, NY: IBM Corp.). Baseline characteristics of cases and controls were analyzed using descriptive statistics. The normality of continuous data was assessed by the Kolmogorov–Smirnov test. The data were described as mean ± standard deviation or median ± inter-quartile range for parametric and non-parametric data, respectively. Comparison of the various parameters between cases and controls was done by independent Student’s t test and χ2 test for parametric data and Mann–Whitney U test for non-parametric data. The levels of the various biochemical parameters were correlated with psoriasis area severity index (PASI), using Spearman rank correlation. Analysis was carried out at 5% level of significance and p < 0.05 was considered as statistically significant.
Results
Table 1 depicts baseline clinicoepidemiologic features of patients and controls each comprising 132 (m:f = 2.5:1) individuals aged between 20 and 79 years. Mild-to-moderate and severe psoriasis was present in 125 (94.7%), and 7 (5.3%) patients, respectively. Psoriatic arthritis was present in 19 (14.39%) patients predominantly comprising asymmetric mono- or oligoarthritis variety noted in 10 patients. Seventy (53%) and 58 (43.9%) patients, respectively, were habitual smokers and alcohol consumers as compared to 33 (25%) and 15 (11.4%) controls and the difference was statistically significant (p < 0.001). BMI and waist:hip ratio of patients and controls showed no statistical significant difference. After investigations, one or more co-morbidities (diabetes mellitus, hypertension, obesity (BMI = 25–30 kg/m2), and metabolic syndrome) were detected in 57 (43.2%) patients and were significantly higher compared to 40 (30.3%) controls (Table 1).
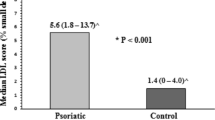
Lipid abnormalities were noted in 94 (71.2%) patients and 82 (62.1%) controls but the difference was not statistically significant except for number of patients with psoriasis and low serum HDL levels were significantly more than controls. The LDL, LDL/HDL ratio, non-HDL/HDL ratio, serum MDA and lipoprotein-a levels, CLTI, and AI were significantly higher in patients than controls (Table 2).
The 75 (56.8%) patients with psoriasis and 92 (69.7%) controls without any co-morbidity were statistically comparable in age, gender, BMI, waist:hip ratio, lipid profile including serum LDL, and Framingham risk score (Table 3). However, greater number of patients without co-morbidities had history of alcohol consumption and smoking, and showed significantly higher LDL/HDL ratio compared to controls. The serum MDA and lipoprotein-a levels, CLTI and AI were also significantly higher in patients than in controls without co-morbidities. However, these parameters did not significantly differ in patients and controls with and without co-morbidities (Table 4). Similarly, in both patients and controls with or without history of smoking and alcohol consumption these parameters were comparable statistically.
The 19 (14.4%) patients with psoriatic arthritis had significantly lower history of smoking (26.4% vs. 57.5%; p = 0.01), higher mean BMI (24.37 ± 3.76 vs. 22.47 ± 3.42; p = 0.03), and median MDA levels (39.5 ± 23.08 vs. 28.2 ± 19.4; p = 0.04) compared to 113 (85.6%) patients without arthritis (Table 4).
A positive correlation between serum MDA and lipoprotein-a levels, CLTI and AI was observed in all the 132 patients with or without co-morbidities as well as in 92 patients having no co-morbidities (Figs. 1, 2). Although disease severity (PASI score) correlated positively with lipoprotein-a and AI, correlation between disease severity and MDA levels and CLTI was not statistically significant in 132 psoriasis patients. However, disease severity in patients without co-morbidities showed no correlation with these parameters. A negative correlation between serum MDA and disease duration was also noted in all 132 patients but not in patients without co-morbidities.
A positive correlation between serum MDA levels and lipoprotein-a (p < 0.001, r = 0.546), CLTI (p = 0.006, r = 0.237) and AI (p < 0.001, r = 0.509) observed in patients with or without co-morbidities (N = 132) suggests that inflammation and oxidative stress are common factors responsible for this abnormality in psoriasis patients with or without co-morbidities. There is a negative correlation between MDA and disease duration (p = 0.019, r = − 0.237). (Spearman rank correlation analysis was carried out at 5% level of significance and p < 0.05 was considered significant. Malondialdehyde ranks lip-a ranks R2 linear = 0.298; malondialdehyde ranks AI ranks R2 linear = 0.299; malondialdehyde ranks CLTI ranks R2 linear = 0.056)
A positive correlation between serum MDA levels and lipoprotein-a (p < 0.001, r = 0.56), CLTI (p < 0.001, r = 0.402) and AI (p < 0.001, r = 0.592) was noted in patients without co-morbidities (N = 75) suggests that inflammatory process and oxidative stress of psoriasis are common factors responsible for this abnormality in psoriasis patients. (Spearman rank correlation analysis was carried out at 5% level of significance and p < 0.05 was considered significant. Malondialdehyde ranks lip-a ranks R2 linear = 0.03; malondialdehyde ranks AI ranks R2 linear = 0.362; malondialdehyde ranks CLTI ranks R2 linear = 0.162)
Twenty-nine (21.9%) patients with psoriasis had high and intermediate FR score compared to 19 (14.4%) controls but the difference was not statistically significant (Table 2). However, FR score (Table 4) was significantly higher in psoriasis patients who were smokers and in those with newly detected co-morbidities compared to non-smokers and who had no co-morbidities. Similarly, controls with history of smoking and alcohol consumption had higher Framingham risk score compared to those who did not smoke or consume alcohol.
Discussion
The overall clinicoepidemiologic features, habits of smoking and alcohol consumption, and increased presence of co-morbidities such as hypertension, obesity in our study subjects corroborates as described in the literature [18, 37, 39]. Psoriasis, an immune-mediated inflammatory dermatosis, is strongly associated with metabolic syndrome or its individual components. Although, exact pathophysiology of association between psoriasis and co-morbidities remains obscure, it has been frequently linked to abnormal lipid metabolism manifesting as elevated triglycerides, LDL and total cholesterol levels, and higher plasma lipid and lipoprotein levels in psoriasis patients than controls [21, 28, 36, 39]. Wakkee et al. [39] reported significantly deteriorated lipid profile with higher cholesterol, triglycerides, LDL, and HDL levels in patients with moderate-to-severe psoriasis while only HDL levels were significantly lower in less severe cases as compared to controls. These lipid abnormalities have been attributed to inflammation and elevated TNF-α levels, and increased oxidative stress [14, 15, 20]. Even though one or more lipid abnormalities were noted in our 71.2% psoriasis patients compared to 62.1% controls, the difference was not statistically significant except for number of patients with low levels of HDL, which is important in suppression of atherogenicity and resultant cardiovascular complications such as stroke or myocardial infarction.
Increased serum MDA is an indirect marker of oxidative stress/damage to polyunsaturated fatty acids and has been noted to increase significantly in individuals having hypertension, diabetes or in patients with psoriasis alone [5, 16, 17, 20, 24, 27, 31, 38]. All our 132 psoriasis patients had significantly higher serum MDA levels as compared to controls. The serum MDA levels were also significantly higher in 75 (56.8%) psoriasis patients without co-morbidities and 19 (14.4%) patients with arthritis compared to 92 (69.7%) controls without co-morbidities and 113 (85.6%) without arthritis, respectively. It appears that psoriasis and psoriatic arthritis-induced inflammation with or without co-morbidities itself is a risk factor for elevated MDA levels independent of other co-morbidities. This view is also strengthened from observation of serum MDA levels increasing proportionately to disease severity, arthritis and duration, and decreasing following remission and clinical improvement after treatment with infliximab or efalizumab attributable to decreased disease-associated inflammatory activity and oxidative stress [3, 4, 25, 36]. However, disease severity and duration do not appear to consistently influence tissue/serum MDA levels [33]. We also observed a negative and weak correlation (p = 0.019, r = − 0.237) between serum MDA levels and disease duration and no correlation with disease severity. This might be due to mild-to-moderate disease in majority of our patients, past remissions, and multiple treatments that could not be ascertained in most cases.
Increased lipoprotein-a levels impart an enhanced risk of coronary artery disease that increases many folds with concomitant presence of low HDL cholesterol, high total cholesterol and LDL, and high total cholesterol/HDL ratio [35]. With few exceptions, higher lipoprotein-a levels in psoriasis patients than controls have been observed [10, 22, 26, 36]. According to Ferretti et al. [10], higher levels of lipoprotein-a are more susceptible to lipoprotein peroxidation and oxidative stress damage reflecting that psoriasis is perhaps an independent risk factor for its increased levels, atherogenic and thrombogenic events and increased cardiovascular disease. Significantly higher levels of lipoprotein-a, non-HDL:HDL and LDL:HDL ratios were also seen in all our patients compared to controls. The levels of lipoprotein-a also correlated significantly with MDA levels (p < 0.001, r = 0.546) and PASI (p = 0.003, r = 0.25). Elevation of CLTI and lipoprotein-a is indicative of abnormal lipid metabolism and has been observed in patients of acute coronary syndrome and are considered strong predictors of risk for cardiovascular disease compared to individual lipid parameters or other risk factors [8, 30, 34, 36]. We observed significantly higher levels of CLTI and AI in all our psoriasis patients with and without co-morbidities. Similarly, a positive correlation between serum MDA levels and CLTI and AI was observed in all psoriasis patients with or without co-morbidities. However, there was no difference in serum MDA, lipoprotein-a levels, CLTI and AI in patients and controls with and without a history of smoking or alcohol intake. These findings suggest that psoriasis and associated inflammation and oxidative stress are perhaps independent risk factors for abnormally elevated indices, high atherogenic tendency and possibly increased cardiovascular disease. In contrast to higher Framingham risk score in psoriasis patients compared to controls noted by Sunitha et al. [36], we made no such observations in our study despite abnormal parameters of lipid metabolism and oxidative stress. However, smoking and/or alcohol consumption appear to increase it significantly in both patients and controls as compared to those who did not smoke or consume alcohol. Despite significantly higher Framingham risk score in our patients with co-morbidities, no difference in serum MDA and lipoprotein-a levels compared to those without co-morbidities suggests that presence of diabetes mellitus, hypertension, metabolic syndrome and obesity perhaps compound the risk for cardiovascular disease in psoriasis while serum MDA and lipoprotein-a levels alone may not be useful surrogate markers for assessing cardiovascular risk [36]. However, some influence of ethnicity, lifestyle, concurrent co-morbidities, psoriasis severity, and study methodology on our results cannot be ruled out. Cross-sectional nature of study, a small number of patients particularly with arthritis and their inconsistent distribution between different forms of psoriasis, and no follow-up for cardiovascular events or assessment of study parameters post-treatment/remission remains few limitations of the study. Malondialdehyde and other anti-oxidants in tissues, and other serum oxidant markers were not assessed and the Framingham risk score is not validated in Indian patients.
Conclusions
Psoriasis-associated inflammatory milieu and resultant oxidative stress is perhaps responsible for dyslipidemia, an increase in oxidant stress markers and lipid ratios which may indirectly predispose to development of atherosclerosis and cardiovascular disease. The disease severity and duration seem to have inconsistent influence on atherogenic/thrombogenic risk indicators, though they tend to correlate well amongst themselves. The possible effects of low disease severity, past treatments, multiple remissions and the presence of co-morbidities on our results cannot be ruled out. Even though FR score was increased in psoriasis patients with co-morbidities, it was not increased in psoriasis patients with elevated serum MDA, lipoprotein-a levels and lipid ratios compared to controls, making them not so useful markers of cardiovascular risk in psoriasis patients. Nevertheless, lifestyle modification, regular-screening psoriasis patients for early detection and management of co-morbidities and cardiovascular events, statins and anti-oxidant supplementation along with conventional psoriasis treatment may benefit them in the long term.
Abbreviations
- LDL:
-
Low-density lipoprotein
- LP-a:
-
Lipoprotein-a
- HDL:
-
High-density lipoprotein
- VLDL:
-
Very low-density lipoprotein
- MDA:
-
Malondialdehyde
- AI:
-
Atherogenic index
- CLTI:
-
Comprehensive lipid tetrad index
- BMI:
-
Body mass index
- FR:
-
Framingham risk
- PASI:
-
Psoriasis area severity index
- CRP:
-
C-reactive protein
- ROS:
-
Reactive oxygen species
References
Akkara Veetil BM, Matteson EL, Maradit-Kremers H, McEvoy MT, Crowson CS (2012) Trends in lipid profile in patients with psoriasis: a population based analysis. BMC Dermatol 12:20
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(suppl 1):S62–S69
Ashok V, Divya R, Karthikeyan K (2016) A study of correlation between serum malondialdehyde and the clinical severity of psoriasis. J Evid Based Med Healthc 3:1086–1088
Attwa E, Swelam E (2011) Relationship between smoking-induced oxidative stress and the clinical severity of psoriasis. J Eur Acad Dermatol Venereol 25:782–787
Baweja P, Agarwal BK, Sharma VK, Alex A (2013) Oxidant and antioxidant status in patients with psoriasis. Indian J Appl Pure Biol 28:143–148. http://biology-journal.org/journal.php?p=152
Burman A, Jain K, Gulati R, Chopra V, Agarwal DP, Vasisht S (2004) Lipoprotein(a) as a marker of coronary artery disease and its association with dietary fat. J Assoc Physicians India 52:99–102
Cozzani E, Rosa G, Burlando M, Parodi A (2018) Psoriasis as a cardiovascular risk factor: updates and algorithmic approach. G Ital Dermatol Venereol 153:659–665
Das B, Daga MK, Gupta SK (2007) Lipid Pentad Index: a novel bioindex for evaluation of lipid risk factors for atherosclerosis in young adolescents and children of premature coronary artery disease patients in India. Clin Biochem 40:18–24
National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) (2002) Third report of the National Cholesterol Education Program (NCEP). Circulation 106:3143–3421
Ferretti G, Bacchetti T, Campanati A, Simonetti O, Liberati G, Offidani A (2012) Correlation between lipoprotein(a) and lipid peroxidation in psoriasis: role of the enzyme paraoxonase-1. Br J Dermatol 166:204–207
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112:2735–2752
Gupta M, Chari S, Borkar M, Chandankhede M (2011) Dyslipidemia and oxidative stress in patients of psoriasis. Biomed Res 22:222–225. https://pdfs.semanticscholar.org/2165/a012a1fa7655954120f50be80b8e445e6040.pdf
Helliwell PS, Taylor WJ (2005) Classification and diagnostic criteria for psoriatic arthritis. Ann Rheum Dis 64:ii3–ii8
Jyothi RS, Govindswamy KS, Gurupadappa K (2011) Psoriasis: an oxidative stress condition. J Clin Diagn Res 5:252–253. http://www.jcdr.net/article_fulltext.asp?id=1247
Kadam DP, Suryakar AN, Ankush RD, Kadam CY, Deshpande KH (2010) Role of oxidative stress in various stages of psoriasis. Indian J Clin Biochem 25:388–392
Kumawat M, Sharma TK, Singh I, Singh N, Ghalaut VS, Vardey SK et al (2013) Antioxidant enzymes and lipid peroxidation in type 2 diabetes mellitus patients with and without nephropathy. N Am J Med Sci 5:213
Latha MM, Bhaskar MV, Preethi AS, Priyanka M, Srilakshmi P (2015) Status of serum lipids and oxidative stress in psoriatic cases. Int J Med Health Sci 4:337–340. http://www.ijmhs.net/articles/1436580
Loo SKF, Yeung KH, Ho KM, Loo KK (2010) Cardiovascular comorbidities in psoriasis. Hong Kong J Dermatol Venereol 18:72–81. http://medcomhk.com/hkdvb/pdf/2010v18n02-03.pdf
Morais CA, Oliveira SH, Lima LM (2013) Lipid tetrad index (LTI) and lipid pentad index (LPI) in healthy subjects. Arg Bras Cardiol 100:322–327
Nassiri S, Malekzad F, Sarlak M, Saeedi M, Hedayati M, Qaisari M (2009) Interplay among antioxidants and oxidants in psoriasis. Iranian J Dermatol 12:56–59. http://www.iranjd.ir/download.asp?code=IJD09124856
Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM (2006) Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol 55:829–835
Nemati H, Khodarahmi R, Rahmani A, Ebrahimi A, Amani M, Eftekhari K (2013) Serum lipid profile in psoriatic patients: correlation between vascular adhesion protein-1 and lipoprotein (a). Cell Biochem Funct 31:36–40
Ng CY, Tzeng I-S, Liu S-H, Chang Y-C, Huang Y-H (2018) Metabolic parameters in psoriatic patients treated with interleukin-12/23 blockade (ustekinumab). J Dermatol 45:309–313
Nordestgaard BG, Chapman MJ, Ray K, Borén J, Andreotti F, Watts GF et al (2010) Lipoprotein (a) as a cardiovascular risk factor: current status. Eur Heart J 31:2844–2853
Peluso I, Cavaliere A, Palmery M (2016) Plasma total antioxidant capacity and peroxidation biomarkers in psoriasis. J Biomed Sci 23:1–13
Pietrzak A, Kadzielewski J, Janowski K, Roliński J, Krasowska D, Chodorowska G et al (2009) Lipoprotein (a) in patients with psoriasis: associations with lipid profiles and disease severity. Int J Dermatol 48:379–387
Pietrzak A, Michalak-Stoma A, Chodorowska G, Sczpietowski JC (2010) Lipid disturbance in psoriasis: an update. Mediat Inflamm 2010:535612. https://doi.org/10.1155/2010/535612
Poudyal Y, Rajbhandari SL (2014) Lipid profile in psoriasis. J Univers Coll Med Sci 2:16–19
Rajappa M, Shridhar MG, Balachander J, Sethuraman KR (2006) Lipoprotein (a) and comprehensive lipid tetrad index as a marker of coronary artery disease in NIDDM patients in South India. Clin Chim Acta 372:70–75
Senthilkumari S, Sasivathanam N, Ramadevi M, Thangavelu K (2016) Is lipid tetrad index a promising atherogenic index in acute coronary syndrome? Int J Sci Study 4:73–77. https://www.ijss-sn.com/uploads/2/0/1/5/20153321/ijss_nov_oa16_-_2016.pdf
Shahzad F (2012) Malondialdehyde: an efficient marker of target organ dysfunction in hypertension. J Med Res Pract 1:76–79
Shrestha A, Bahce-Altuntas A, Mowrey W, Broder A (2016) Active peripheral inflammation is associated with pro-atherogenic lipid profile in psoriatic arthritis. Semin Arthritis Rheum 46:286–290
Sikar Aktürk A, Özdoğan HK, Bayramgürler D, Çekmen MB, Bilen N, Kiran R (2012) Nitric oxide and malondialdehyde levels in plasma and tissue of psoriasis patients. J Eur Acad Dermatol Venereol 26:833–837
Singh Y, Srivastava S, Ahmad S, Mishra SK, Shirazi N, Raja M et al (2010) Is lipid tetrad index the strongest predictor of premature coronary artery disease in North India? J India Acad Clin Med 11:175–179. http://medind.nic.in/jac/t10/i3/jact10i3p175.pdf
Singla S, Kaur K, Kaur G, Kaur H, Kaur J, Jaswal S (2009) Lipoprotein (a) in type 2 diabetes mellitus: relation to LDL:HDL ratio and glycemic control. Int J Diabetes Dev Ctries 29:80–84
Sunitha S, Rajappa M, Thappa DM, Chandrashekar L, Munisamy M, Revathy G et al (2015) Comprehensive lipid tetrad index, atherogenic index and lipid peroxidation: surrogate markers for increased cardiovascular risk in psoriasis. Indian J Dermatol Venereol Leprol 81:464–471
Thomas J, Kumar NA, Manoharon D, Cynthia S, Selva Prabhu SK, Ahmad NA (2009) A study of comorbid conditions in psoriasis. J Pak Assoc Dermatol 19:200–202. http://www.jpad.com.pk/index.php/jpad/article/view/544
Vanizor Kural B, Örem A, Çimşit G, Yandi YE, Calapoǧlu M (2003) Evaluation of the atherogenic tendency of lipids and lipoprotein content and their relationships with oxidant–antioxidant system in patients with psoriasis. Clin Chim Acta 328:71–82
Wakkee M, Thio H, Prens E, Sijbrands E, Neumann H (2007) Unfavorable cardiovascular risk profiles in untreated and treated psoriasis patients. Atherosclerosis 190:1–9
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97:1837–1847
World Health Organizations (2000) The Asia Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Sydney
Acknowledgements
Mr. Ramesh Chand Goel (MSc.), former Biostatistician, Post Graduate Institute of Medical Education and Research, Chandigarh (India), helped in statistical analysis of the data. His erudite association throughout the study is gratefully acknowledged. The authors also thank their patients/subjects who volunteered for the study.
Author information
Authors and Affiliations
Contributions
DW obtained compiled, analyzed all data and prepared the initial draft. VKM analyzed and interpreted data, drafted, and critically evaluated the manuscript for important intellectual content. RSY and SB provided intellectual help in investigative study and interpretation of biochemistry results. KSM, PSC, VS, AS, AS, and SC helped in obtaining, compiling and interpretation of data and literature search. All the authors were involved in the revision of the draft manuscript and have agreed to the final content.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no competing interest and, therefore, nothing else to declare, and have contributed significantly and take full responsibility for the manuscript. The authors of the paper are obliged to confirm that it has not been previously published. The study was not funded by any agency. The clinical data form part of the thesis submitted to Himachal Pradesh University, Shimla, (H.P.) for the degree of M.D. (DVL.).
Statement of ethics
The study was approved by Institutional Scientific Protocol Review Committee and Institutional Ethics Committee (Rgn no ECR/490/Inst/HP/2013/RR-16). Informed consent was obtained from all the patients for being enrolled in the study. All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wadhwa, D., Mahajan, V.K., Mehta, K.S. et al. Malondialdehyde, lipoprotein-a, lipoprotein ratios, comprehensive lipid tetrad index and atherogenic index as surrogate markers for cardiovascular disease in patients with psoriasis: a case–control study. Arch Dermatol Res 311, 287–297 (2019). https://doi.org/10.1007/s00403-019-01896-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-019-01896-y