Abstract
Introduction
Detailed postoperative rehabilitation protocols after hip arthroscopy for femoroacetabular impingement syndrome (FAIS) are still a matter of debate. Adjunctive hip bracing represents a promising tool to improve early patients’ mobilization. To present, the effect of hip brace therapy on postoperative functional outcomes and specific patient individual psychologic factors remains controversially discussed. Consequently, we aimed to report postoperative outcomes focusing on hip function, pain and kinesiophobia between braced and unbraced patients.
Materials and methods
A prospective, randomized-controlled trial was conducted, including patients undergoing hip arthroscopy for FAIS. After exclusion, a final study cohort of 36 patients in the intervention group (postoperative hip brace) and 36 patients in the control group (no hip brace) were compared for kinesiophobia (Tampa Scale of Kinesiophobia), pain (Visual analog scale) and joint function (International Hip Outcome Tool-12) within the first six postoperative months.
Results
Hip arthroscopy significantly improved all patient-reported outcomes in both groups. Intergroup analysis revealed significantly lower levels of kinesiophobia in braced patients at 6-months follow up (30.7 vs. 34.1, p = 0.04) while not negatively affecting pain and joint function. No intra- and postoperative complications occurred within both groups.
Conclusions
This study could demonstrate that bracing after hip arthroscopy can positively influence kinesiophobia, while the brace did not negatively impact postoperative pain and quality of life. Thus, hip bracing could be a viable assistive therapy in the postoperative rehabilitation phase after hip arthroscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip arthroscopy is a well-established procedure to treat intra- and extraarticular hip pathologies in a minimally invasive approach [1,2,3]. The increasing numbers of hip arthroscopies in femoroacetabular impingement syndrome (FAIS)—as a main cause of hip pain in young and active patients—underline its feasibility in this field of hip preserving surgery [4,5,6,7].
Besides continuous improvements in arthroscopic technology and technique, increasing attention has been paid to the individual factors that influence postoperative outcomes [8,9,10,11]. In this context, psychological distress connected to persisting pain and reduced mobility demonstrated a significant association with postoperative results in hip-preserving interventions [12,13,14,15]. For instance, a high level of postoperative pain can lead to excessive fear of physical activity, known as kinesiophobia [16]. Utilizing the Tampa Scale of Kinesiophobia (TSK) to objective this factor of psychological distress, a high level of kinesiophobia has already demonstrated its association with poor postoperative results across various orthopaedic interventions [17,18,19]. Thus, there is a clear need for evidence-based intraoperative and postoperative care to improve patient outcomes in this context [20].
In postoperative rehabilitation after hip arthroscopy a recent systematic review found, that hip bracing is a commonly used supportive intervention [21]. Benefits of an postoperative brace therapy are connected to the prevention of excessive joint motion and the offloading of the surrounding muscle, resulting in improved joint stability and the protection of the operative repaired tissue [22, 23]. Nevertheless, some surgeons recommend a postoperative brace therapy only in a few specific arthroscopic procedures [24]. Wearing a brace in patients with patellofemoral pain already demonstrated a positive impact on kinesiophobia, while there is paucity in literature regarding brace therapy after hip arthroscopy for FAIS [25].
It becomes clear, that prospective studies are needed to illuminate the effect of hip brace therapy on postoperative functional outcomes and specific patient individual psychologic factors to further improve rehabilitation protocols.
Therefore, the aims of this study were (1) to compare the postoperative kinesiophobia and pain level between an intervention (hip bracing) and a control (no hip bracing) group within the first six months longitudinally and (2) to report the patient-reported outcome using the iHot-12 score in the short-term follow-up. We hypothesized that the postoperative use of a hip brace leads to an improvement in the mentioned scores.
Patients and methods
Study design
Inclusion criteria consisted of clinical and radiological diagnosis of symptomatic FAIS, failure of conservative treatment, patient age > 18 years, and the capacity to provide informed permission. Hip dysplasia (lateral center–edge angle of Wiberg (LCEA) < 25°), osteoarthritis (Tönnis grade > 1), history of pediatric hip disorders, chronic pain syndrome, revision hip arthroscopy, and refusal to participate in this study were exclusion criteria. During the selected time period, 122 individuals underwent hip arthroscopy between December 2022 and December 2023. 50 patients were excluded from the analysis due to the aforementioned exclusion criteria, leaving 72 patients available for the study (Fig. 1).
The patients were randomly assigned into an intervention group (postoperative hip brace) and a control group (postoperative routine care without hip brace) resulting in a final study cohort of 36 patients in the study group and 36 patients in the control group. Five patients were lost to follow-up (intervention group: two, control group: three). All included patients completed a frequent clinical follow-up six weeks, three months and six months postoperatively.
Surgical technique and postoperative regime
Two fellowship-trained hip surgeons (A.Z., C.S) performed all procedures in the supine decubitus position using two to three standardized portals. A post-traction system was used for arthroscopy. During surgery the central and the periphery compartments were accessible. Acetabuloplasty, femoroplasty, and a combination procedure were used to treat pincer, cam, and mixed-type FAIS. If preservation of the labrum was feasible, a labrum repair was performed; otherwise, the labrum was reconstructed. Periportal capsulotomies were performed on each patient. An interportal capsulotomy was performed and later restored in the case of a significant cam morphology.
Postoperatively, a partial weight-bearing of 20 kg for 6 weeks was recommended. Hip flexion was limited to a maximum of 90° for 6 weeks. The intervention group was treated postoperatively by wearing an additional hip brace (HipoCross, Orthoservice AG, Switzerland) for six weeks, whereas the postoperative mobilization in the control group did not include wearing such a hip brace. Continuous passive motion was recommended for four hours daily to reduce intra-articular adhesion risk. A three-week course of oral nonsteroidal anti-inflammatory drugs achieved pharmaceutical prophylaxis of ossification.
Patient-reported outcomes and statistics
Preoperatively, 6 weeks, three months, and six months postoperatively, kinesiophobia was assessed using the Tampa Scale of Kinesiophobia (TSK), and the pain level was reported using a visual analog scale (VAS). Higher values indicated a higher level of kinesiophobia and pain.
The patients' quality of life was assessed using the International Hip Outcome Tool-12 (iHot-12) preoperatively and six months after hip arthroscopy.
The sample size was calculated to have a power of 0.80 (1-β). Thirty-two patients were required in each group. In consideration of a 10% loss, 36 patients were selected for each group, for a total of 72 patients. G*Power software was used to calculate the sample size (version 3.1.9.4).
Descriptive statistics were used to summarize the patient characteristics and outcomes. Patient-reported outcome data were reported as mean with standard deviation. Xlstat was utilized for statistical calculations (ADDINSOFT, Paris, France). Chi-Square and Fisher Exact tests were employed to compare categorical data. Continuous data were compared using a two-tailed t-test (assuming normally distributed data) and Wilcoxon rank-sum test (for non-normally distributed data). A p-value less than 0.05 was considered statistically significant.
Ethical considerations
All patients gave written informed consent prior to inclusion. Ethics approval (F-2022-112) was obtained from the local independent ethics committee according to the World Medical Association Declaration of Helsinki. The study was registered within the Federal Clinical Trials Registry (DRKS00030873).
Results
Patient demographics
The preoperative patient demographics are presented in Table 1. The mean age at the time of surgery was 37.5 years. 61% of patients were male; the mean body mass index (BMI) was 25.5 kg/m2. The intervention group included 59% male patients with a mean age of 36.6 years and a mean BMI of 23.5 kg/m2. Compared to this group, the control group included a higher percentage of male patients (78% vs. 59%) and showed a higher mean age (38.5 vs. 36.6 years) and mean BMI (25.6 vs. 23.5 kg/m2) at the time of hip arthroscopy.
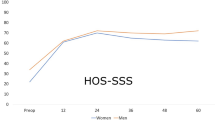
Tampa scale of kinesiophobia and visual analog scale for pain
Preoperatively, the mean TSK score showed no significant differences between the intervention and the control group (40.9 vs. 41.6, p = 0.86). Postoperatively, the TSK score declined continuously in both groups compared to the preoperative state (Table 2). The postoperative values were lower in the intervention group compared to controls at all postoperative follow-up time points, without reaching statistical significance six weeks (mean, 37.9 vs. 39.6, p = 0.38) and three months (mean, 34.8 vs. 36.7, p = 0.42) postoperatively.
At the latest follow-up, the mean TSK score was significantly lower in the intervention group (mean, 30.7 vs. 34.1, p = 0.04).
The preoperative pain level showed comparable values between both groups (mean, 6.4 vs. 6.1, p = 0.86). Hip arthroscopy led to a significant decline of pain in both groups with continuously decreasing values across the postoperative follow-up examinations. Comparing the postoperative pain levels between both groups, there were no significant differences (Table 3).
International hip outcome tool-12
Before hip arthroscopy, there were no significant differences comparing the mean iHot-12 scores between the intervention and the control group (41.9 vs. 42.9, p = 0.83). At the latest follow-up the iHot-12 had significantly improved within both groups (p < 0.001). Intergroup analysis showed no significant difference between the mean scores 6 months postoperatively (61.5 vs. 62.7, p = 0.49) (Table 4).
None of the patients experienced any postoperative complications, nor were any complications reported as a result of the brace. No patient was taking pain medication at the six-month follow-up.
Discussion
The main result of the study was, that wearing a hip brace after arthroscopy positively influenced kinesiophobia, while the brace did not negatively impact postoperative pain and quality of life. Thus, hip bracing could be a viable adjunctive therapy to improve patients´ mobility after hip arthroscopy.
Femoroacetabular impingement syndrome (FAIS) is a frequent cause of hip pain in young patients [7, 26]. Detailed rehabilitation protocols after hip arthroscopy for FAIS are not well established yet, even when hip braces are often utilized to assist mobilization after surgery [21, 27]. Based on the idea of tissue protection and muscle offloading, using a hip brace should normalize gait patterns while walking and reducing pain to improve early mobilization [22, 23, 28]. A recent study investigated the biomechanical effects of hip braces on patients after hip arthroscopic surgery for FAIS, finding that wearing a hip brace significantly reduced the peak hip flexion angle and the peak acceleration of the greater trochanter during standing-up and walking tasks at three weeks postoperatively. The authors suggested that hip braces may offer protective benefits for the repaired tissues during the early stages of postoperative recovery for patients undergoing arthroscopic FAI correction and labral preservation surgery [22].
In knee surgery, it has already been demonstrated beneficial impacts on postoperative outcomes. For instance, in patients with high levels of kinesiophobia, a functional brace therapy improved the functional outcome and kinesiophobia postoperatively [16, 29]. After hip arthroscopy, rehabilitation protocols utilizing a brace have poorly been studied and demonstrated conflicting results. Recently, Wentzel et al. studied 193 patients after hip arthroscopy for FAIS and found no significant differences between braced and unbraced patients regarding patient-reported outcomes and reoperation rates [30]. These results are in line with our findings. Nonetheless, factors like mental health or kinesophobia were not considered in the methods. A recently published study by Nasir et al. was able to demonstrate that poor physical function and high pain scores eight weeks after hip arthroscopy were associated with increased kinesiophobia [31]. We could demonstrate, that kinesiophobia was significantly reduced six months after hip arthroscopy in braced patients. A prospective cohort-study by Clapp et al. demonstrated a significant decline in kinesiophobia one year after hip arthroscopy for FAIS [32]. This finding is emphasized by our study, suggesting that a brace seems to enhance the improvement of kinesophobia. Consequently, using a brace after surgery could lead to an improvement in TSK scores when elevated TSK levels are observed before the operation.
Nevertheless, prospective, randomized-controlled trials are needed to enhance the level of evidence for detailed recommendations on postoperative rehabilitation [33, 34]. To date, there is one randomized-controlled trial being conducted (Clinical Trial NCT04599296) on postoperative hip bracing after arthroplasty, but its results are still pending. Therefore, our study represents the first randomized-controlled trial in this area reporting on patient-reported outcome as well as patient individual psychological factors.
While the present study reports beneficial effects of postoperative hip bracing in a prospective, monocenter series, several limitations of this study must be considered. The study included only patients receiving hip arthroscopy to treat FAIS and there could be an increased risk for selection and treatment bias caused by two surgeons in one high-volume center performing all surgeries in this study. Nevertheless, the prospective, randomized study design including a control group should be noted as a strength of this study. However, the study groups were not balanced by sex and the higher rate of male patients in the control group could have influenced the results. Even when sex-related differences in postoperative outcomes have already been reported for different orthopaedic procedures, randomized-controlled trials cannot guarantee sex-balanced study groups. Additionally, multi-center studies could be beneficial to improve the generalizability of the results. Last, the data were limited to a short-term follow-up period of six months. Thus, mid- and long-term outcomes have to be reported in future studies.
Besides all mentioned limitations, the present study demonstrates significant clinical improvement in postoperative patients´ mobilization utilizing a hip brace in a prospective, randomized-controlled trial. The results of this study enhance the understanding of postoperative patient´s care after hip arthroscopy for FAIS substantially. Further research is warranted to improve postoperative rehabilitation recommendations, particularly across variable indications in hip preservation by arthroscopy.
Conclusion
This study could demonstrate that bracing after hip arthroscopy can positively influence kinesiophobia, while the brace did not negatively impact postoperative pain and quality of life. Thus, hip bracing could be a viable assistive therapy in the postoperative rehabilitation phase after hip arthroscopy.
References
Domb BG et al (2018) Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med 46(2):305–313
Jimenez AE et al (2021) Achieving successful outcomes in high-level athletes with borderline hip dysplasia undergoing hip arthroscopy with capsular plication and labral preservation: a propensity-matched controlled study. Am J Sports Med 49(9):2447–2456
Menge TJ et al (2020) Hip arthroscopy for femoroacetabular impingement in adolescents: 10-year patient-reported outcomes. Am J Sports Med 49(1):76–81
Bozic KJ et al (2013) Trends in hip arthroscopy utilization in the United States. J Arthroplasty 28(8):140–143
Lee, M.S., et al., Patients undergoing primary hip arthroscopy report favorable outcomes at minimum 10 year follow-up: a systematic review. Arthroscopy: The J Arthrosc Related Surg 2023. 39(2): 459–475.
Domb BG et al (2023) Ten-year survivorship, outcomes, and sports participation in athletes after primary hip arthroscopy for femoroacetabular impingement syndrome. Am J Sports Med 51(9):2383–2395
Ganz R et al. (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthopaedics Related Res® 417: 112–120.
Jamil M et al (2018) Hip arthroscopy: indications, outcomes and complications. Int J Surg 54:341–344
Beck, E.C., et al. (2021) Gender and age-specific differences observed in rates of achieving meaningful clinical outcomes 5-years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy 37(8): 2488–2496. e1.
Parvaresh K et al (2021) The influence of body mass index on outcomes after hip arthroscopy for femoroacetabular impingement syndrome: five-year results in 140 patients. Am J Sports Med 49(1):90–96
Shankar DS et al (2024) Five-year outcomes of primary hip arthroscopy for femoroacetabular impingement syndrome among female patients: higher body mass index is associated with reduced clinically significant outcomes. Arthroscopy 40(3):732–741
Stone AV et al. (2019) Preoperative predictors of achieving clinically significant athletic functional status after hip arthroscopy for femoroacetabular impingement at minimum 2-year follow-up. Arthroscopy 35(11): 3049–3056. e1.
Fischer M et al (2023) Psychological factors as risk contributors for poor hip function after periacetabular osteotomy. J Clin Med 12(12):4008
Dick AG et al (2020) The impact of mental health disorders on outcomes following hip arthroscopy for femoroacetabular impingement syndrome: a systematic review. J Hip Preserv Surg 7(2):195–204
Bech NH et al (2021) The influence of pain catastrophizing and central sensitization on the reported pain after hip arthroscopy. Knee Surg Sports Traumatol Arthrosc 29(9):2837–2842
Leeuw M et al (2007) The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 30:77–94
Woby SR et al (2005) Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain 117(1–2):137–144
Brown OS et al (2020) The effects of kinesiophobia on outcome following total knee replacement: a systematic review. Arch Orthop Trauma Surg 140:2057–2070
Kemani MK et al (2020) Fear of movement is related to low back disability during a two-year period in patients who have undergone elective lumbar spine surgery. World Neurosurg 137:e416–e424
Lynch TS et al (2020) Best practice guidelines for hip arthroscopy in femoroacetabular impingement: results of a Delphi process. JAAOS-J Am Acad Orthopaedic Surgeons 28(2):81–89
Mavrommatis S et al. Postoperative brace use after hip arthroscopy: a systematic review. HSS Journal®, 2023: 15563316231190603.
Hirata K et al (2023) Biomechanical analysis of hip braces after hip arthroscopic surgery for femoroacetabular impingement syndrome: an observational study. Biomimetics 8(2):225
Domb BG, Sgroi TA, VanDevender JC (2016) Physical therapy protocol after hip arthroscopy: clinical guidelines supported by 2-year outcomes. Sports Health 8(4):347–354
Gupta A et al (2015) Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy 31(9):1722–1727
Priore LB et al (2020) Two weeks of wearing a knee brace compared with minimal intervention on kinesiophobia at 2 and 6 weeks in people with patellofemoral pain: a randomized controlled trial. Arch Phys Med Rehabil 101(4):613–623
Griffin DR et al (2016) The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 50(19):1169–1176
Stalzer S, Wahoff M, Scanlan M (2006) Rehabilitation following hip arthroscopy. Clin Sports Med 25(2):337–357
Cvetanovich GL et al (2017) Variability and comprehensiveness of North American online available physical therapy protocols following hip arthroscopy for femoroacetabular impingement and labral repair. Arthroscopy 33(11):1998–2005
Harput G et al (2016) External supports improve knee performance in anterior cruciate ligament reconstructed individuals with higher kinesiophobia levels. Knee 23(5):807–812
Wentzel D et al (2023) Benefits of a postoperative hip orthosis after routine arthroscopy of the hip: a retrospective cohort study. Orthop J Sports Med 11(11):23259671231212504
Nasir M, Scott EJ, Westermann RC (2023) Pain catastrophizing, kinesiophobia, stress, depression, and poor resiliency are associated with pain and dysfunction in the hip preservation population. Iowa Orthop J 43(2):125–132
Clapp IM et al (2020) What is the role of kinesiophobia and pain catastrophizing in outcomes after hip arthroscopy for femoroacetabular impingement syndrome? Arthrosc Sports Med Rehabil 2(2):e97–e104
Lim HC et al (2014) Randomised trial support for orthopaedic surgical procedures. PLoS ONE 9(6):e96745
Robinson A et al (2019) The challenges of translating the results of randomized controlled trials in orthopaedic surgery into clinical practice. The Bone & Joint Journal 101(2):121–123
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was funded by Orthoservice, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexander Zimmerer received consultant fees from Arthrex and Orthoservice. The other authors report no conflict of interest.
Ethical approval
This study was approved by IRB/Ethikkommission Landesärztekammer Baden-Württemberg, Germany.
Informed consent
All patients consented to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fischer, M., Nonnenmacher, L., Sobau, C. et al. Postoperative hip bracing reduces kinesiophobia in patients undergoing hip arthroscopy: a randomized-controlled trial. Arch Orthop Trauma Surg 144, 3205–3210 (2024). https://doi.org/10.1007/s00402-024-05437-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05437-9