Abstract
Purpose
This study aimed to investigate functional outcome and complications after primary and revision modular H-TKA using hybrid fixation with cementless stems.
Methods
Between 2015 and 2018, 48 patients with 50 implants were included after hybrid implantation of a single design H-TKA system using cementless osseointegrating stems and modular components. Complications and clinical outcome were analysed using Knee Society Score (KSS), the Western Ontario McMasters Universities Osteoarthritis Index (WOMAC) and the Short-Form Health Survey 12 (SF-12) score.
Results
Indications for implantation were aseptic revision (n = 29, 58%), primary TKA (n = 19, 38%) and two-stage septic revisions (n = 2, 4%). Complications were reported in 26% (n = 12), whereas complications associated with hybrid fixation occurred in 5 (10%) cases, with 2 (4%) requiring revision surgery for aseptic loosening and 3 (6%) treated with an adapted postoperative protocol for perioperative fractures. Implant survivorship was 84% after a mean follow-up of 54 months. Postoperative KSS significantly improved from 51.50 (12–100) to 78.36 (41–99; p < 0.001). The mean WOMAC score was 19.26 (0–55), SF-12 PCS was 41.56 points (22.67–57.66) and SF-12 MCS was 49.21 points (23.87–63.21).
Conclusion
Hybrid modular implantation in H-TKA provides satisfactory clinical and functional results in primary and revision TKA. Clinical outcomes significantly improve with reduced pain, increased mobility, and good-to-excellent functional scores after implantation. Whilst implant survival is comparable to previous studies and complications associated with hybrid fixation are low, general complication rates are comparably high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hinged total knee arthroplasty requires the use of highly constrained designs in cases of irreversible soft- or bone-tissue damage, which are frequently encountered in revision total knee arthroplasty (TKA). In the US, TKA revisions are predicted to increase by 601% in the 25 years from 2005 to 2030 [1]. The most common reasons for revision TKA are aseptic loosening, infection and implant failure [2, 3], all of which may result in major bone defects and soft tissue damage. Although constrained condylar implants provide promising long-term results [4], the use of hinged total knee prostheses is not limited to cases that have been inadequately treated with a semi-constrained prosthesis as diverging results have been published [5]. Hence, there is no international standard on implant choice and the development of hinged knee prostheses has rapidly advanced in the last 20 years [6]. Recently introduced improvements in implant design have resulted in implant survival rates (after a 10-year follow-up) of up to 90.2% for third-generation hinged TKA (H-TKA) [7]. Therefore, with improved long-term results and decreasing revision rates, the traditional existing limitations on the usage of hinged prostheses are diminishing [8, 9].
Prosthesis fixation presents a key challenge in the presence of bone defects. Modern systems for H-TKA offer modular augments to address bone defects. Additional metaphyseal fixation may be achieved using sleeves and cones, which are shown to be a reliable fixation method in cases of bone loss [10]. To ensure sufficient prosthesis–bone fixation, cemented implantation of pediculated implants is commonly used in H-TKA as they offer excellent results with low rates of micromotion and aseptic loosening. However, especially in primary H-TKA in younger patients, hybrid implantation using only cement coating of surfaces, and therefore relying on cementless zonal fixation, offers multiple benefits such as bone stock preservation and easier implant revision procedures [11]. The use of cementless press-fit stems can help with aligning the prosthesis and varus/valgus stability, given the intramedullary guidance and helps retaining the bone mineral density due to favourable stress loading [12]. Additional fixation and further improved offloading of stresses in the prosthesis bone interface can be achieved using porous osseointegrating stems, a unique characteristic of the implant used in this study. Drawbacks of cementless stems are potential risks of end of stem pain as well as potentially demanding revision procedures when working with strong fixation porous osseointegrating stems. To date, owing to the inhomogeneity in reported cases and heterogeneous results published, there is no superiority to either, cementless or cemented fixation technique [13].
With ongoing developments in implantation systems, the functional outcome and complication rates must be continuously analysed to assure safety and durability of available prostheses. Recent studies are providing increasing insights into the outcome and complications of H-TKA. However, owing to limited case numbers with a variety of manufacturers and models, and the constant modifications in implant design, it is almost impossible to compare outcomes of cemented and cementless H-TKA using a randomised control trial [11]. Therefore, case series from specialised arthroplasty centres remain of particular importance in implant surveillance.
The aim of this study was to investigate the functional outcome and complication rates after primary and revision arthroplasty using a hybrid modular, single design, rotating hinge implant. Fixation is achieved with porous, osseointegrating cementless stems in line with modular components such as augments and sleeves or cones. Additional data on the use of modular augmentation depending on pre-existing bone defects according to the Anderson Orthopaedic Research Institute (AORI) classification is provided. Furthermore, a literature review was performed, and results are compared to studies identified in the review. We hypothesise potentially increased rates of aseptic loosening and end of stem pain attributed to the use of cementless osseointegrating stems compared to previous studies.
Materials and methods
Patient characteristics
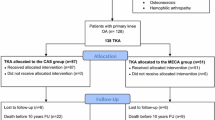
This study was a prospective monocentre trial. Patients were followed up and included in the study when a H-TKA had been performed. All patients fitted with the latest-generation MUTARS® GenuX® MK System (Implantcast GmbH, Buxtehude, Germany) between 2015 and 2018 were invited to participate in the study. Exclusion criteria were the use of H-TKA systems other than the specified model; and cemented stems. Hybrid implantation was defined as cemented implantation of the femoral and tibial components with cementless implantations of stems and modular components, if used, as intended by the manufacturer. A particular characteristic of the specified implant is a porous cementless stem designed to achieve osseointegration. Modular combinations of offsets, augments, sleeves and cones are possible. Patient allocation to the study is shown in the CONSORT flow diagram (Fig. 1). The study was approved by the institutional review board (IRB approval: 2018-A427-1). Informed consent was obtained from all participants.
Surgical procedure
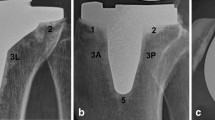
The study was performed at a primary academic referral centre for arthroplasty. Surgeries were performed by two independent and experienced, senior surgeons. The revision implant was pre-planned using preoperative planning software (mediCAD, Hectec, Altdorf, Germany). Fixation was achieved using cementless stem implants whenever possible. If cemented fixation was used, patients were excluded from the subsequent analysis. In case of bone defects, an optimal fit was ensured using spacers, cones and sleeves. The stems were implanted without cement after reaming in a press-fit technique, whereas the rear surfaces of the femur and tibial component itself are designed to be cemented in every case. In cases where cones were used, they were filled with polymethyl methacrylate (PMMA) bone cement on the inside with the porous surface on the outside implanted cementless. Sleeves were always implanted cementless. The implant is displayed in Fig. 2. All study participants received the mobile-bearing variant of the implant, allowing up to 20 degrees of rotation. Intraoperative local infiltration of analgesia (LIA) was used in all patients. Early mobilisation under full weight bearing was conducted in patients without intraoperative complications. Physiotherapeutic support was provided, and motorised knee movement rails (continuous passive motion [CPM]) were used during the hospital stay (Artromot, DJO, Germany). Full weight bearing and full range of motion were allowed in post-surgery, the target hospital stay was one week and this was followed by a 3-week rehabilitation programme, which is the standard procedure for TKA patients in this country.
Radiographic and photographic implant images. Postoperative X-rays after aseptic revision arthroplasty using the GenuX® MK System (Implantcast GmbH, Buxtehude, Germany) with a hybrid fixation showing (a) ap, (b) tangential patellar and (c) lateral view. d The implant in an exploded-view drawing showing the coupling and the coated tibial component as well as a tibial stem for cementless fixation. The implant is modular with optional stem offsets, augments, sleeves, cones, cemented vs. uncemented osteointegrated stems and fixed vs. mobile-bearing (MB) variants. In this cohort only cementless stems and MB variants are used
Outcome measures
Patient characteristics and comorbid conditions were collected. The Charlson Comorbidity Index was used to categorise the severity of comorbidity. Supplementary data on surgical indication, number of prior prostheses, incision–suture time and access to surgical site were obtained.
All postoperative complications were defined as being either major (surgical revision required) or minor (surgical revision not required). Surgical complications during treatment or within the first four weeks after discharge were classified according to the classification system by Goslings and Gouma[14].
Patient-reported outcome measures (PROMS) were taken pre- and postoperatively after a minimum follow-up of 12 months. Each patient was physically examined pre- and postoperatively. Clinically important differences in pain score were defined as a reduction of 1 point. In addition, participants completed a questionnaire in which they provided information about function and quality of life. The functional outcome was measured pre- and postoperatively using the Knee Society Score (KSS) with clinically relevant differences defined as 9 (knee score) and 10 (function score) points [15]. The Western Ontario McMasters Universities Osteoarthritis Index (WOMAC) and the Short-Form Health Survey 12 (SF-12) were only taken during follow-up.
Radiological images were collected from all patients pre- and postoperatively. The type of preoperative bone defect was graded using the AORI classification of bone defects in TKA [16].
To assess implant survival, additional patient surveys were conducted after a minimum follow-up of 48 months. Patients were screened for follow-up surgeries in our institution or questioned for external follow-up therapies regarding their TKA.
Literature review
A literature review was performed following the Cochrane Review Methods using the MEDLINE database (1 January 1980 to 20 December 2022). After the initial online search, relevant articles were manually selected. Selection criteria were primary studies reporting clinical and/or functional outcome after implementation of a H-TKA with additional reporting on cementless or hybrid implant fixation. Articles published in English language were selected. Search terms used in the title, abstract, MeSH, and keywords fields were (‘knee’ [MeSH] OR ‘knee joint’ [MeSH] OR ‘knee prosthesis’ [MeSH] OR ‘knee prosthesis’[tiab] OR ‘total knee arthroplasty’ [tiab]) AND (‘hinge’ [tiab] OR ‘rotating hinge’ [tiab] OR ‘RHK’ [tiab] OR ‘hinged prosthesis’ [tiab] OR ‘hinged implants’ [tiab] OR ‘revision knee arthroplasty’ [tiab] OR ‘revision total knee arthroplasty ‘ [tiab]) AND (‘cementless’ [tiab] OR ‘hybrid’ [tiab] OR ‘fixation’ [tiab]). After the initial online search, relevant articles and their bibliographies were manually reviewed.
Statistical analysis
The primary outcome of this study was the time until implant failure, defined as revision for any reason, such as aseptic loosening, septic revision, or implant exchange. The secondary outcome was defined as the functional outcome as described in the previous section. To assess improvement after implantation, the following null hypothesis was set: H0 There is no difference in pre- and postoperative outcomes scores. The D'Agostino–Pearson test was used to evaluate raw data for normality. We subsequently used the Wilcoxon signed-rank test and Student’s t-test to evaluate differences between the two groups. Analysis of variance (ANOVA) was used for the descriptive statistics of means. The level of statistical significance was set at p < 0.05. All tests were two-sided. SPSS, version 22.0 (IBM Inc., Armonk, NY, USA), was used for treatment comparisons.
Results
Patient demographics
A total of 126 patients underwent a H-TKA between 2015 and 2018. After excluding 56 patients receiving a different implant and 13 patients with cemented implants, 57 patients were included in the study allocation. Nine patients did not join the follow-up examination, but the remaining 48 patients with 50 GenuX implants agreed to participate in the study. Allocation and follow-up are shown in the standardised flow diagram (Fig. 1). Patient characteristics and the indication for surgery are shown in Table 1. The indication for surgery was most frequently aseptic or septic revision (n = 31; 62%), followed by primary TKA (n = 19; 38%).
Clinical outcomes (PROMS)
The mean KSS knee score significantly improved from 51.5 points preoperatively to 78.4 points postoperatively (p < 0.001), and the mean KSS function score increased from 57.7 points preoperatively to 69.2 points postoperatively (p = 0.019) (Table 2). There was a highly significant reduction between the preoperative and postoperative pain levels without weight-bearing (3.66 vs. 1.05, p < 0.001) and with weight bearing (6.12 vs. 3.05, p < 0.001). The postoperative walking distance compared with the preoperative walking distance improved significantly by 52% (p < 0.001). Preoperatively, 56.25% of the patients were able to walk more than 500 m, and postoperatively, this increased to 87.5%. Quality of Life (SF-12) and WOMAC scores were used only in postoperative follow-up. Detailed PROMS are shown in Table 3.
Radiographic analysis
At the time of primary follow-up, one unrevised component showed radiological signs of loosening (radiolucent lines). This prosthesis was removed due to aseptic loosening after 48 months. None of the prostheses showed a malrotation. The joint line of the implant was optimal in all unrevised knees. Postoperative leg axis valgus malalignment was observed in four patients, with three patients having pre-existing genu valgum. No other radiological complications were observed.
Modular augmentation for bone defects
Amongst the 50 implantations, femoral modular augments were used in 33 (66.0%) implants and tibial modular augments were used in 21 (42.0%) implants. In 96.0% of the implantations, femoral and tibial bone defects were present and classified as AORI 1 or higher. In the presence of more severe bone defects (AORI 2b or higher), a combination of augments was used (Table 4).
Implant survivorship
Overall survivorship was 90% after a mean follow-up of 21 months (range 12–36 months). At the latest follow-up evaluation with a mean follow-up period of 54 months (range 48–71 months), overall implant survivorship was 84%. Eight patients underwent a revision surgery with exchange or removal of the H-TKA implant (Table 5). The mean time until removal was 30 months (range 1–48 months), with one prosthesis being removed after 1 month owing to periprosthetic joint infection (PJI) with sepsis after a one-stage aseptic exchange. The most frequent reason for implant removal was PJI (n = 6, 12.0%). In four out of six cases with PJI, the indication for implantation was aseptic loosening or two-stage reimplantation after an infected TKA. One prosthesis had to be removed at 18 months post-surgery and another had to be removed at 48 months post-surgery due to aseptic loosening (4.0%). Implant survival is depicted in a standardised Kaplan–Meier graph (see Fig. 3).
Complications
Fixation-associated complications occurred in five implantations (10.0%). Intraoperative fractures were recorded in three cases (6.0%). In one case (2.0%), an intraoperative femoral fracture was detected during stem implantation and additional cable wires were used (Goslings and Gouma grade 1). In two patients (4.0%), postoperative tibial non-dislocated fractures were detected in routinely obtained postoperative X-rays; the patients subsequently underwent adapted postoperative treatment, including partial weight bearing, for several weeks (Goslings and Gouma grade 1). Two patients reported tibial stem pain after cementless implantation during clinical follow-up (6 weeks after discharge), with both patients reporting no symptoms during the latest follow-up.
Complications independent of the fixation method were reported in eight implantations (16.0%). Six (12.0%) of these complications resulted in implant removal, whereas the other two reported complications required different treatments. One patient-reported patellofemoral pain during follow-up examination (6 weeks after discharge), which was due to secondary patellofemoral arthrosis, and was treated with revision surgery for patellar resurfacing. The other patient had a superficial wound infection (CDC category A2) that required a debridement, antibiotics, and implant retention (DAIR) procedure (Goslins and Gouma grade 2).
Medical complications included catheter-associated urinary tract infection (n = 5, 10%; Goslings and Gouma grade 0) and deep vein thrombosis (n = 1, 2%; Goslings and Gouma grade 1). Catheter-associated urinary tract infection was not associated with superficial wound infection or septic loosening.
Complications within the first four weeks after discharge according to Goslings and Gouma occurred in n = 11 (22.0%) cases, graded zero in n = 5 cases, 1 in n = 4 cases, 2 in n = 1 case and 3 in n = 1 case (PJI).
Discussion
In this prospective monocentric study, a cohort of 48 patients with 50 implants was prospectively followed up according to the survivorship of the cementless stem guided TKA, specific complications and the patient’s functional outcome and quality of life. An implant survivorship of 84% after a mean follow-up of 54 months was recorded, which was congruent with a previous study examining the same implant design [17]. Complications that were directly connected to the cementless stem fixation occurred in 10% of the implantations, which is comparable to the published literature [17]. After implantation, significant improvements regarding KSS functional outcome scores were observed, and patients reported less pain as well as improvements in daily living measured by the WOMAC score.
In addition to the retrospective and prospective analysis, we conducted a literature review (Table 6) as our study does not provide a cemented control group. Nine studies were found that examined outcomes, complications and implant survival after (rotating) H-TKA [7, 8, 17,18,19,20,21,22,23]. However, only one study by Theil et al. examined the MUTARS GenuX (Implantcast, Germany) implant [17].
Overall complications
The overall complication rate was 26% (13/50). Only 10% (5/50) of implantations had complications that were directly associated with the fixation method, whereas other complications were observed in 16% (8/50) of the total implantations. These fixation-independent complications (n = 8, 16.0%) consisted of seven infections (14.0%). This rate seems high, but our study cohort did include two-stage septic and aseptic revision cases. In the studies identified in our literature review, the complication rates for PJI range from 2.4% in a single study [7] to 8–26.4% [8, 17, 19, 20]. The range of reported complication rates for PJI can be attributed to different indications within the analysed studies. Comparing the studies, a higher PJI rate is often associated with a study population that includes patients undergoing septic revision. This is consistent with previous literature [24], with PJI often reported as one of the most common causes of failure after H-TKA [25]. A meta-analysis by Onggo et al. recently concluded that fixation method is not a risk factor for PJI [26]. Complications with extensor mechanism failure (e.g. patellofemoral pain, quad/patellar tendon rupture) are not uncommon after H-TKA, with complication rates ranging from 1 to 6% [6, 19, 27, 28]. In our study population, one patient (2%) reported patellofemoral pain during follow-up and was treated with patellar resurfacing. Patellar resurfacing is a procedure that has been extensively studied and discussed but is still without uniform indication and therapy recommendations [29]. In general, in patients with multiple revisions before implantation or complex arthritis resulting in the selection of a H-TKA, soft tissue damage of the extensor mechanism and patellar damage are more common and a complication rate of 2% can be considered low.
Complications associated with cementless stem fixation
Although complications have been reported in 26% of implantations, fixation-associated complications only occurred after five (10%) implantations, with two patients (n = 2, 4%) requiring revision surgery. Intraoperative tibial (n = 2) and femoral (n = 1) fractures may be attributed to hybrid implementation as previously reported [30]. The periprosthetic fracture rate of 6% in our study is consistent with previous publications reporting periprosthetic fracture rates from 1 to 10% [17, 27, 31]. However, adapted partial weight-bearing was sufficient in two (4.0%) of the cases in this study and only the third case (n = 1, 2.0%) required additional cable wires during implantation.
The only study investigating the same implant as our study was by Theil et al. and reported a correlation of aseptic loosening to fixation method (hybrid 14% versus cemented 0%; p = 0.06) [17]. Guttowski et al. recently published a biomechanical in vitro study showing that cones and cementless stems provide good stability in the presence of large bone defects, concluding that the bone quality should determine fixation method [32]. A general approach to use cementless stem fixation in the presence of good bone quality in combination with augments to achieve sufficient fixation in at least two zones seems most appropriate. Cement removal is often associated with a major loss in bone stock and the risk of iatrogenic fractures, especially in young patients undergoing complex primary TKA as well as in cases with high re-revision rates [33]. Furthermore, a recent study by Hipfl et al. demonstrated significantly higher re-infection rates and more severe bone loss in cemented septic revision compared with cementless septic revision [34], supporting the use of cementless implants, especially in the light of previously discussed higher infection rates. Nevertheless, a consensus on the fixation method regarding implant survival, revision rates and clinical outcome is yet to be found.
Two patients in our cohort reported tibial stem pain after cementless stem implantation. A recently published retrospective cohort study found no differences in tibial pain at the end of the stem in cementless and cemented revision TKA (p = 1.0) [35], although the analysed implants differ from those in this study. During the first follow-up in our study, one incidence of radiolucent lines was observed with no clinical symptoms of loosening. As previously reported, radiolucent lines without loosening may be attributed to sufficient zonal fixation [36], which can be achieved utilising cones or sleeves in cases with bone defects. In our study, the implant had to be removed after 48 months due to aseptic loosening. We therefore recommend close radiographic monitoring and clinical follow-ups in cases with radiolucent lines.
Implant survival
Overall implant survival in our study was 90.0% with a mean follow-up of 21 months and a minimum follow-up of 12 months, and 84% with a mean follow-up of 54 months and a minimum follow-up of 48 months. Compared with the studies identified in our literature review, the only study using the same implant reported an implant survival rate of 91.3% after 2 years and 69.7% after 5 years [17]. When the studies that utilised other implant designs were included in the comparison, survival rates of 69.7% to 94% were reported after a 60-month follow-up (Table 6). Whilst Theil et al. observed a trend of improved survival in fully cemented implants [17], Hu et al. reported higher survival rates with cementless implantation compared with cemented implantation for a different implant (5-year follow-up: 94% versus 75%, respectively) [20]. Therefore, the hybrid implantation used in our study yields comparable implant survival rates after a 4-year follow-up [17, 19,20,21]. In our study, most implants had to be removed due to septic loosening or PJI and complications leading to implant removal associated with fixation method are low.
Functional outcome and quality of life
This is the first study to report clinical and functional outcomes after cementless fixation of this single implant design, providing pre- and postoperative functional patient evaluations. We reported significant improvements of the KSS knee and function scores, and these improvements are higher than previously reported minimal clinically important difference of 7.2 for KSS knee and 6.3–9.7 for KSS function scores [15]. Our results are comparable with previously published results [8, 18]. Range of motion (ROM) improved from 93.65 to 98.33 degrees, which is comparable to that in a study by Heesterbeek et al. using the Legion Revision TKA (Smith & Nephew, USA) [18]. In their study with 32 patients, Heesterbeek et al. concluded that there was no difference in clinical scores between fixation techniques after a 2-year follow-up [18]. The mean postoperative WOMAC score was 19.26 (range 0–55) in our study, which is well within reported outcomes after modern primary TKA using a lower constrained prosthesis (e.g. cruciate-retaining or posterior-stabilised) [37]. Mean postoperative SF-12 PCS and MCS scores were 41.56 and 49.21, respectively, comparable to scores for primary TKA in a population < 65 years (SF-12-PCS 39.1–82.6 and SF-12-MCS 44.5–74.6) [38].
As previously stated, Theil et al. [17] are the only authors who have examined the same implant design as that used in this study. Although the focus of their study was implant survival, Theil et al. did evaluate functional outcome postoperatively with a mean WOMAC of 127 (n = 71), but the score calculation is unclear and comparison with our study is therefore impossible. However, Theil et al. found that implant fixation was not correlated with functional outcome [17].
Limitations
This study has several limitations. First, implant survival was validated after a follow-up with a minimum of 48 months. We state that these results are midterm results because, although these findings are of clinical interest, additional studies with follow-up periods of 5 or 10 years are required to assess long-term implant outcome parameters. Second, we report a limited cohort of 48 patients because all implant designs other than the investigated one were strictly excluded. Moreover, an a priori power analysis and reliable sample calculation could not be performed due to the rare indication and especially limited use of porous osseointegrating stems in the literature, with the potential of low statistical power. However, considering single implants, our patient number is comparable to those of several recently published studies that examined outcomes after H-TKA [7, 8, 19]. Third, for six patients (12.5%), postoperative PROMs could not be obtained because patient travel distance to the hospital was too far. Nonetheless, patients were followed up with telephone interviews to monitor complications and implant survival. Fourth, cemented implantations were excluded, leading to a potential bias towards more easily managed bone defects with better implant survival and functional outcome. During the study period, only 13 patients had at least one of the stems in their implant cemented as we favour cementless stem implantation whenever possible. In previous literature, no significant difference in implant survival was observed comparing hybrid and cemented fixation of the studied implant [17]. However, to our knowledge, studies investigating functional outcomes comparing cemented and hybrid fixation of the implant in this study do not exist and differences between fixation methods might occur. Despite these limitations, the findings of this study are of clinical relevance because they provide data on a rarely reported implant and an infrequently used implantation method for patients with complex primary and revision arthroplasty.
Conclusion
This is the first study investigating the clinical and functional outcomes after hybrid fixation of the GenuX implant (Implantcast, Germany) in complex primary and revision arthroplasty. Clinical and functional outcomes significantly improve postoperatively, with reduced pain, increased mobility, and good-to-excellent results in functional scores. Although total complication rates are comparably high in the context of H-TKA cases, cementless fixation-associated complications are low compared with the published literature. Cementless stems in combination with modular components as augments, offsets, and sleeves or cones lead to the possibility of guaranteeing a proper fixation even in large bone defects.
Data availability
Raw data for this study are not publicly available to preserve individuals’ privacy under the European General Data Protection Regulation.
Abbreviations
- AORI:
-
Anderson Orthopaedic Research Institute
- H-TKA:
-
Hinge total knee arthroplasty
- KSS:
-
Knee Society Score
- PJI:
-
Periprosthetic joint infection
- PMMA:
-
Polymethyl methacrylate
- PROMS:
-
Patient-reported outcome measures
- ROM:
-
Range of motion
- SF-12:
-
Short-Form Health Survey 12
- SF-12 MCS:
-
SF-12 mental component score
- SF-12 PCS:
-
SF-12 physical component score
- TiN:
-
Titanium nitride coating
- TKA:
-
Total knee arthroplasty
- WOMAC:
-
Western Ontario McMasters Universities Osteoarthritis Index
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Tarazi JM, Chen Z, Scuderi GR, Mont MA (2021) The epidemiology of revision total knee arthroplasty. J Knee Surg 34(13):1396–1401
Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G (2013) Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 28(8):1329–1332
Kim YH, Park JW (2020) Long-term (Up to 21 Years) survival of revision total knee arthroplasty with use of a constrained condylar knee prosthesis: a concise follow-up of a previous report. J Bone Joint Surg Am 102(8):674–678
Miralles-Muñoz FA, Pineda-Salazar M, Rubio-Morales M, González-Parreño S, Ruiz-Lozano M, Lizaur-Utrilla A (2022) Similar outcomes of constrained condylar knee and rotating hinge prosthesis in revision surgery for extension instability after primary total knee arthroplasty. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2022.103265
Shen C, Lichstein PM, Austin MS, Sharkey PF, Parvizi J (2014) Revision knee arthroplasty for bone loss: choosing the right degree of constraint. J Arthroplasty 29(1):127–131
Wignadasan W, Chang JS, Kayani B, Kontoghiorghe C, Haddad FS (2021) Long-term results of revision total knee arthroplasty using a rotating hinge implant. Knee 28:72–80
Bingham JS, Bukowski BR, Wyles CC, Pareek A, Berry DJ, Abdel MP (2019) Rotating-hinge revision total knee arthroplasty for treatment of severe arthrofibrosis. J Arthroplasty 34(7s):S271-s276
Gehrke T, Kendoff D, Haasper C (2014) The role of hinges in primary total knee replacement. Bone Joint J 96(11):93–95
Fischer LT, Heinecke M, Röhner E, Schlattmann P, Matziolis G (2022) Cones and sleeves present good survival and clinical outcome in revision total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 30(8):2824–2837
Kang SG, Park CH, Song SJ (2018) Stem fixation in revision total knee arthroplasty: indications, stem dimensions, and fixation methods. Knee Surg Relat Res 30(3):187–192
Driesman AS, Macaulay W, Schwarzkopf R (2019) Cemented versus cementless stems in revision total knee arthroplasty. J Knee Surg 32(8):704–709
Wang C, Pfitzner T, von Roth P, Mayr HO, Sostheim M, Hube R (2016) Fixation of stem in revision of total knee arthroplasty: cemented versus cementless-a meta-analysis. Knee Surg Sports Traumatol Arthrosc 24(10):3200–3211
Goslings JC, Gouma DJ (2008) What is a surgical complication? World J Surg 32(6):952
Lizaur-Utrilla A, Gonzalez-Parreño S, Martinez-Mendez D, Miralles-Muñoz FA, Lopez-Prats FA (2020) Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surg Sports Traumatol Arthrosc 28(5):1473–1478
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167–175
Theil C, Schmidt-Braekling T, Gosheger G et al (2020) Acceptable mid- to long-term survival rates and functional outcomes following a single design rotating hinge total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28(6):1868–1875
Heesterbeek PJ, Wymenga AB, van Hellemondt GG (2016) No difference in implant micromotion between hybrid fixation and fully cemented revision total knee arthroplasty: a randomized controlled trial with radiostereometric analysis of patients with mild-to-moderate bone loss. J Bone Joint Surg Am 98(16):1359–1369
Houfani F, Mainard D, Rubens-Duval B, Papin PE, Pasquier G, Ehlinger M (2021) Rotating-hinge prosthesis for aseptic revision knee arthroplasty: a multicentre retrospective study of 127 cases with a mean follow-up of five years. Orthop Traumatol Surg Res 107(3):102855
Hu CC, Chen SY, Chen CC, Chang YH, Ueng SW, Shih HN (2017) Superior survivorship of cementless vs cemented diaphyseal fixed modular rotating-hinged knee megaprosthesis at 7 years’ follow-up. J Arthroplasty 32(6):1940–1945
Kearns SM, Culp BM, Bohl DD, Sporer SM, Della Valle CJ, Levine BR (2018) Rotating hinge implants for complex primary and revision total knee arthroplasty. J Arthroplasty 33(3):766–770
van Laarhoven SN, van Eerden AHJ, van Hellemondt GG, Schreurs BW, Wymenga AB, Heesterbeek PJC (2022) Superior survival of fully cemented fixation compared to hybrid fixation in a single design rotating hinge knee implant. J Arthroplasty 37(3):482–487
Spranz DM, Koch KA, Reiner T, Hetto P, Gotterbarm T, Merle C (2022) Mid-term results of complex primary total knee arthroplasty using a rotating-hinge implant. Knee 34:34–41
Baek JH, Lee SC, Jin H, Kim JW, Ahn HS, Nam CH (2021) Poor outcomes of revision total knee arthroplasty in patients with septic loosening compared to patients with aseptic loosening. J Orthop Surg Res 16(1):624
Caron É, Gabrion A, Ehlinger M et al (2021) Complications and failures of non-tumoral hinged total knee arthroplasty in primary and aseptic revision surgery: a review of 290 cases. Orthop Traumatol Surg Res 107(3):102875
Onggo J, Onggo J, Phan K, Wilson C (2020) Comparison of infection in cemented, cementless and hybrid primary total knee arthroplasty: a network meta-analysis and systematic review of randomized clinical trials. ANZ J Surg 90(7–8):1289–1298
Farid YR, Thakral R, Finn HA (2015) Intermediate-term results of 142 single-design, rotating-hinge implants: frequent complications may not preclude salvage of severely affected knees. J Arthroplasty 30(12):2173–2180
Baier C, Lüring C, Schaumburger J et al (2013) Assessing patient-oriented results after revision total knee arthroplasty. J Orthop Sci 18(6):955–961
Molfetta L, Casabella A, Palermo A (2020) The patellar resurfacing in total knee prosthesis: indications for bone stock and patellar morphology. Front Med (Lausanne) 7:405
Ponzio DY, Shahi A, Park AG, Purtill JJ (2015) Intraoperative proximal femoral fracture in primary cementless total hip arthroplasty. J Arthroplasty 30(8):1418–1422
Hossain F, Patel S, Haddad FS (2010) Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res 468(5):1221–1228
Guttowski D, Polster V, Huber G, Morlock MM, Püschel K, Nüchtern J (2020) Comparative biomechanical in vitro study of different modular total knee arthroplasty revision stems with bone defects. J Arthroplasty 35(11):3318–3325
Fleischman AN, Azboy I, Fuery M, Restrepo C, Shao H, Parvizi J (2017) Effect of stem size and fixation method on mechanical failure after revision total knee arthroplasty. J Arthroplasty 32(9s):S202-S208.e201
Hipfl C, Leopold V, Becker L, Pumberger M, Perka C, Hardt S (2022) Two-stage revision for periprosthetic joint infection in cemented total hip arthroplasty: an increased risk for failure? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04671-3
Larson DJ, Rosenberg JH, Lawlor MA et al (2021) Pain associated with cemented and uncemented long-stemmed tibial components in revision total knee arthroplasty. Bone Joint J 103(6):165–170
Morgan-Jones R, Oussedik SI, Graichen H, Haddad FS (2015) Zonal fixation in revision total knee arthroplasty. Bone Joint J 97(2):147–149
Singleton N, Nicholas B, Gormack N, Stokes A (2019) Differences in outcome after cruciate retaining and posterior stabilized total knee arthroplasty. J Orthop Surg (Hong Kong) 27(2):2309499019848154
Trieu J, Gould DJ, Schilling C, Spelman T, Dowsey MM, Choong PF (2020) Patient-reported outcomes following total knee replacement in patients <65 years of age-a systematic review and meta-analysis. J Clin Med 9(10):3150
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript. Study is based on institutional review board (IRB) approval. Study is part of thesis of Line Hofmann.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schnetz, M., Hofmann, L., Ewald, L. et al. Midterm results of modular hinge total knee arthroplasty using cementless osseointegrating stems: low fixation associated complications and good functional outcome in primary and revision knee arthroplasty. Arch Orthop Trauma Surg 144, 831–845 (2024). https://doi.org/10.1007/s00402-023-05148-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05148-7