Abstract
Purpose
Computer-assisted surgery (CAS) has been proposed to improve the performance of total knee arthroplasty (TKA) by reducing implant mal-position and mechanical axis mal-alignment. However, no clinical study has been performed to evaluate whether CAS improves survivorship of cementless TKA at long-term follow-up. This prospective and comparative study evaluated the outcome and survivorship of a cementless rotating mobile-bearing TKA performed with or without CAS at a minimum 10-year follow-up.
Methods
A continuous series of 138 TKA (SCORE®, Amplitude, Valence, France) comparing 87 CAS TKA versus 51 conventional mechanical technique (MECA) TKA was prospectively included in our total joint registry.
Results
At 10.5 years after implantation, 95 TKA (59 CAS and 36 MECA TKA) were evaluated. No significant difference was detected in the clinical outcome and mechanical axis between the two groups. The overall 10-year survivorship using revision for any reason as end-point was 91 ± 5 % without significant difference detected between the two groups [86 ± 10 % in the MECA group and 94 ± 5 % in the CAS group (n.s.)]. Using aseptic loosening as end-point, the 10-year survivorship was 100 % in both groups. Using secondary patellar resurfacing as end-point, the 10-year survivorship was significantly higher in the CAS than in MECA group (100 and 85 ± 15 %, respectively; p = 0.0039).
Conclusion
With no implant aseptic loosening or mechanical failure at 10.5 years after implantation, the cementless rotating mobile-bearing SCORE® TKA demonstrated favourable survivorship without influence of CAS. However, CAS might influence TKA survivorship by limiting secondary patellar resurfacing.
Level of evidence
Therapeutic, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although cemented fixed-bearing total knee arthroplasty (TKA) is still considered as the gold-standard procedure, cementless mobile-bearing TKA has been proposed as an alternative in an attempt to reduce mechanical failure of implant fixation and aseptic loosening at long-term follow-up, particularly in younger patients [2, 13, 15, 23, 28]. The rationale of cementless mobile-bearing TKA is to reduce contact stress within the implants and subsequent polyethylene (PE) wear, to minimise mechanical forces transferred to the bone–implant interfaces and to overcome—with a biologic fixation—the potential osteolytic effects of PE wear [1, 21]. Modern series focused on cementless TKA outcome reported survivorship up to 96 % at 12.4-year follow-up without significant difference in long-term survivorship between cementless and cemented TKA demonstrated in meta-analyses [22]. More than implant fixation or bearing systems, other parameters such as the design of the prosthetic trochlear groove, patellar resurfacing, bone cuts, ligament balancing and restoration of an anatomic mechanical axis could influence survivorship [20, 25, 36]. To control some of these parameters during surgery, computer-assisted surgery (CAS) has been developed to minimise outliers in component positioning and to improve final mechanical alignment and ligament balance [10, 27, 32]. Meta-analyses tend to demonstrate that improvement in component positioning and mechanical alignment could be achieved with CAS; however, the influence of CAS on TKA clinical outcome and survivorship at long-term follow-up remains controversial [4, 10, 20, 22].
Previous prospective series comparing CAS versus conventional mechanical TKA reported encouraging results of CAS at short-term follow-up or included a limited number of patients for those with a follow-up close to 10 years or reported the use of navigation system prototype [10, 32, 40]. To our knowledge, no prospective and comparative study has been designed to evaluate the long-term outcome and survivorship of a cementless mobile-bearing TKA with selective patellar resurfacing performed using a CAS or using a conventional mechanical technique. Therefore, this prospective study aimed to compare the outcome and survivorship of CAS versus mechanical SCORE® TKA (Amplitude, Valence, France) performed with a selective patellar resurfacing at a 10-year minimum follow-up. The use of CAS was hypothesised to improve outcome and survivorship of cementless TKA and to reduce revisions associated with implant fixation failure or patello-femoral (PF) complications.
Materials and methods
From 2002 to 2004, a continuous series of 128 patients [138 TKA; 88 women, 40 men, mean age = 70 ± 8 years and mean body mass index (BMI) = 30.5 ± 5.5 kg/m2] who underwent TKA for primary knee osteoarthritis using a cementless mobile-bearing SCORE® TKA (Amplitude, Valence, France) were prospectively included in our institutional total joint registry according to the methods proposed in the literature (Fig. 1) [5]. The exclusion criteria were TKA performed for post-traumatic osteoarthritis, inflammatory and micro-crystalline rheumatisms, osteonecrosis and haemophilic arthropathy. Fifty-one SCORE® TKA were implanted using a mechanical conventional technique (MECA group; Fig. 1). Eighty-seven SCORE® TKA were implanted using a CAS technique with a passive imageless navigation system (AMPLIVISION®, Amplitude, Valence, France) dedicated for the SCORE® TKA (CAS group; Fig. 1). In addition, a staged-bilateral TKA was performed with the same technique in four patients in the MECA group and ten patients in the CAS group (n.s.). No randomization was performed for CAS or MECA group assignment. However, the choice of the technique for TKA was defined peri-operatively according to the operating room where the TKA was performed since only one was equipped with a navigation system at the time of the study. The patella was selectively resurfaced in 52 TKA in cases of severe patellar cartilage erosion (Outerbridge grades III and IV), and patellar instability and mal-tracking (28 TKA in the MECA group versus 24 TKA in the CAS group, p = 0.003) [30]. Patellar instability and mal-tracking was investigated intraoperatively with the trial components, and the patella was resurfaced in case of decentred tracking onto the femoral component trochlear groove, lateral sub-luxation or dislocation persistent after patellar reticulum balance. At a minimum 10-year follow-up, 20 patients (22 TKA, mean follow-up = 102 ± 19 months) in the CAS group and 9 patients (9 TKA, mean follow-up = 88 ± 39 months) in the MECA group died of causes that were unrelated to the TKA (Fig. 1). In addition, 6 patients (6 TKA, mean follow-up = 16 ± 20 months) in the CAS group and 4 patients (6 TKA, mean follow-up = 20 ± 37 months) in the MECA group were lost to FU (Fig. 1). Therefore, 59 CAS TKA and 36 MECA TKA were prospectively evaluated and compared at a minimum 10-year follow-up (Fig. 1). No significant difference was detected between the two groups in terms of age, gender, BMI, knee deformity, Ahlback’s stage of osteoarthritis and preoperative Knee Society Score (KSS; Table 1).
Flow diagram illustrating patients’ enrolment, allocation, follow-up and analysis [5]
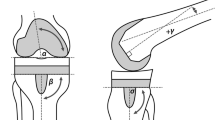
The SCORE® TKA (Amplitude, Valence, France) was introduced in 2002 at our institution and can be implanted using a dedicated passive imageless CAS technique or a conventional mechanical technique. The SCORE® TKA is a cementless ultracongruent mobile-bearing total knee system with an anatomic trochlear groove that aims to prevent patellar instability and mal-tracking, and allows selective patellar resurfacing [12]. The cast of the implants is cobalt–chromium alloy with porous titanium plasma spray–hydroxyapatite (HA) double coating. The PE insert is made of GUR1050 ultra-high molecular weight PE sterilized under vacuum pressure with 30 kGy of γ-irradiation from a 60Co source. The PE insert is ultracongruent and mobile in rotation. All the TKA were performed by or under the supervisions of two senior surgeons without tourniquet and through a standard medial parapatellar approach regardless of the preoperative knee deformity. All patients had peripheral nerve blockade with an indwelling femoral nerve catheter preoperatively. Intraoperative anaesthesia was performed with spinal or general anaesthesia at the discretion of the anaesthesiologist. For both MECA and CAS TKA, the aims to achieve were restoration of a neutral mechanical alignment of 180° ± 3°, symmetric gaps in flexion and extension, and a centred and stable patellar tracking. A mechanical conventional technique was used to implant 51 TKA. Tibial bone resection was determined by the deformity: 10 mm under the lateral plateau for a varus deformity and 7 mm under the medial plateau for a valgus deformity. Gaps in extension and flexion were evaluated before the femoral bone resection with a symmetric 10-mm spacer, and ligament and soft tissue release was eventually performed in a stepwise fashion in order to obtain an optimal ligament tensioning. For the femoral bone resection, a 5-in-1 jig was used with a valgus of 7° for a varus deformity and 5° for a valgus deformity. A CAS technique using a ligament referencing technique was used to implant 87 TKA. The CAS technique (AMPLIVISION®, Amplitude, Valence, France) was composed by passive infrared sensors fixed into the femur and the tibia by threaded bone pins. A “bone morphing” of distal femur and proximal tibia was performed intraoperatively with a special probe. The mechanical axis and angle deformity of the knee were determined with the acquisition of anatomic landmarks (i.e. centre of rotation of the hip, centre of the medial and lateral posterior femoral condyles, centre of the medial and lateral tibial plateaus and tip of the medial and lateral malleoli). Tibial bone resection was performed first according to the deformity and checked using the CAS system. Then, tibiofemoral gaps in flexion and extension, and ligament tensioning were evaluated using the CAS system with a symmetric 10-mm spacer. Ligament and soft tissue release was eventually performed in a stepwise fashion in order to obtain an optimal tensioning. The femoral bone resection was performed using a 5-in-1 jig according to the parameters defined using the CAS system (i.e. varus/valgus alignment, internal/external rotation, lateralization of the femoral component) and then checked. After implantation of the trial components, restoration of the mechanical axis, ligament balance and range of motion (ROM) of the knee were evaluated using the CAS system. Dynamic patellar tracking was carefully investigated intraoperatively with the trial components and balanced whether necessary with a lateral release or medial reefing procedure. Patients were admitted to the hospital after surgery, and a 3- to 5-day stay was routine. All patients received routine peri-operative antibiotic prophylaxis and appropriate anticoagulation for deep venous thrombosis prophylaxis. No peri- or immediate post-operative complications were reported. The same post-operative physical rehabilitation protocol was used for each patient regardless of the group. Structured physical therapy was begun the day after surgery and continued during the in-hospital stay. The patients were instructed to sit up at the bedside the evening of their surgery and to begin ambulating with assistance the day after surgery. Active ROM was encouraged and full weight-bearing ambulation was allowed on post-operative day 2 when quadriceps inhibition from the femoral nerve block had ceased. Discharge was allowed when patients could ambulate 30 m, could ascend and descend three steps, and had pain well controlled with oral medications. Patients were sent home with specific knee ROM exercises and encouraged to seek formal physical therapy on an outpatient basis two or three times per week for the first month.
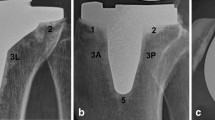
Patients returned for post-operative follow-up visits at 6 weeks, 3 months, 6 months, 1 year and yearly thereafter. At latest follow-up, the evaluation was performed by a single surgeon not involved in any aspect of these patients’ management, care or rehabilitation. In case of inability to attend to the yearly visit, patients were contacted by phone calls and radiographs were prescribed and sent to the evaluating surgeon. The pre- and post-operative evaluations entailed a physical examination with specific evaluation according to Knee Society Score (KSS) with particular attention to anterior knee pain and PF symptoms [17]. Patient’s satisfaction was evaluated using a 4-point Likert scale (i.e. very satisfied, satisfied, disappointed and non-satisfied). Standard weight-bearing antero-posterior and lateral radiographs, full weight-bearing long-leg radiographs and PF Merchant view of the operated knee were obtained pre- and post-operatively. The radiographs at 6 weeks were considered as baseline radiographs for post-operative follow-up comparison. At latest follow-up, comparative radiograph analysis was performed to identify radiolucent lines or osteolysis at the bone–implant interface and the hip–knee–ankle (HKA) angle was measured. Merchant views were compared to assessed PF complications such as centring and tilt of the patella, and progressive narrowing of the PF joint space particularly in case of non-resurfaced patella. Radiographs were assessed using our institutional software (Centricity®, GE Healthcare, Barrington, IL USA) allowing a measurement accuracy of 1 mm for distances and 1° for angles. Owing to the French regulation, patient’s informed consent was not required to be included in this study.
Statistical analysis
Data descriptive statistics are presented as mean ± SD. Qualitative variables were compared using the Chi-squared test. Quantitative and continuous variables were analysed using the following parametric tests: (1) Student’s paired t tests for intragroup comparison of two variables and (2) two-sample t tests for intergroup comparison of two variables. The cumulative survivorship was analysed using Kaplan–Meier curves survival analysis with 95 % confidence intervals, and the survivorship between the two groups was compared using the log-rank test. Failure was defined as the revision of the TKA for any reason, aseptic loosening and secondary patellar resurfacing for PF complications. Patients’ inclusion in this study was not based on an “a priori” sample size calculation. A post hoc power analysis of the hazard ratio between the CAS and MECA groups using TKA revision for any reason has been performed, and the power (1 − β) of this study was 0.21. Statistical analyses were performed using R software (version 2.14.1.) with a level of significance set at p ≤ 0.05.
Results
The mean follow-up of the series averaged 126 ± 6 months (Table 2). At latest follow-up, the improvement in the global KSS, knee KSS and function KSS was significant in both groups (p < 0.0001), except for the gain in flexion, without significant difference detected between the two groups (Table 2). No significant difference in terms of patient’s satisfaction was detected between the two groups (Table 2). The radiographic evaluation demonstrated a significant improvement in the mean post-operative HKA angle in both groups (p < 0.0001) without significant difference between the two groups (Table 2). Ten TKA (32 %) in the MECA group and 13 TKA (23 %) in the CAS group were considered as alignment outliers since their post-operative HKA angle was outside the anatomic range of 180° ± 3° without significant difference detected between the two groups. No radiolucent lines, osteolysis or evidence for aseptic loosening was observed in both groups at latest follow-up. Ten TKA required revision: anterior knee pain in five cases, supracondylar femoral fracture in two cases, peri-prosthetic infection in two cases and stiffness in one case. Among the five TKA revised for anterior knee pain, three revisions were performed in the MECA group for isolated secondary patellar resurfacing and two revisions were performed in the CAS group: one for an over-sizing of the femoral component requiring isolated femoral component revision and one for a patellar over-stuffing of a primary patellar resurfacing requiring isolated patellar component revision. Importantly, no secondary patellar resurfacing was performed in the CAS group at latest follow-up.
At 10-year post-implantation, the overall survivorship of the SCORE® TKA using revision for any reason as end-point was 91 ± 5 % without significant difference detected between the two groups [86 ± 10 % in the MECA group and 94 ± 5 % in the CAS group (n.s.)] (Fig. 2). Using aseptic loosening as end-point, the 10-year survivorship was 100 % in both groups. Importantly, using secondary patellar resurfacing as end-point, the 10-year survivorship was significantly higher in the CAS group than in MECA group (100 and 85 ± 15 %, respectively; p = 0.0039; Fig. 3).
Discussion
The most important finding of the present study was that favourable long-term fixation and survivorship could be achieved with a cementless ultracongruent rotating mobile-bearing TKA in patients with primary osteoarthritis without significant influence of CAS at 10-year follow-up. To our knowledge, the current study was the first designed to prospectively compare the outcome and survivorship of a single design of cementless ultracongruent mobile-bearing TKA with selective patellar resurfacing performed using a CAS technique or a conventional mechanical technique at a minimum 10-year follow-up. Overall, the outcome and the 10-year survivorship of the SCORE® TKA were comparable to previous series focused on cementless fixed- or mobile-bearing TKA [6, 8, 11, 14, 16, 33, 34, 38, 39] (Table 3). With no revision for aseptic loosening at 10.5 years after implantation, our results confirmed and strengthened those previously reported by Châtain et al. [9] demonstrating encouraging results of 447 CAS SCORE® TKA with no aseptic loosening at a mean follow-up of 6.6 years. In addition, Mont et al. [22] reported in a recent review a 10-year survivorship of 95.6 % with cementless TKA, which is comparable to the current series. Importantly, this review did not demonstrate any significant difference in terms of survivorship between cementless TKA and the gold-standard cemented TKA. Taken altogether, these results obtained with hydroxyapatite- or titanium porous-coated cementless TKA indicate that reliable long-term implant osseointegration and fixation could be achieved in primary knee osteoarthritis. However, caution is advised regarding the use of cementless TKA in other aetiologies characterised by a poor bone quality, such as rheumatisms or haemophilic arthropathy, and further clinical studies are required.
CAS has been developed in TKA to minimise outliers in component positioning and to improve final mechanical alignment and soft tissue balance [3, 4, 9, 10, 27, 31, 40]. Châtain et al. [9] demonstrated that CAS enabled a more accurate soft tissue balance achievement and restoration of a neutral limb alignment with improved clinical scores when compared to the conventional mechanical technique. In addition, reporting the results issued from the Australian Orthopaedic Association National Joint Replacement Registry, de Steiger et al. [35] emphasised that CAS reduced the overall rate of TKA revision as well as the rate of revision for loosening/lysis, particularly in patients less than 65 years of age in which higher rates of revision due to wear-related issues were reported in the literature. However, the influence of CAS on TKA clinical outcome and survivorship at long-term follow-up remains debated. Several studies and meta-analyses have demonstrated that positioning the TKA components within 3° of the neutral mechanical axis in the post-operative alignment of the knee could reduce the risks of early PE wear, component loosening and implant mechanical failure [3, 4, 9, 10, 27, 31]. Interestingly, Parratte et al. [24] demonstrated that achievement of a post-operative neutral mechanical axis alignment of 0° ± 3°, as is currently obtained with contemporary CAS systems, could not substantially improve TKA survivorship at long-term follow-up compared to TKA that missed this goal. This result suggests that the importance of a post-operative neutral mechanical axis could be relative compared to ligament and soft tissue balance [7, 9]. Balanced soft tissue and ligament are essential for optimal knee kinematics, and over-tensioning of ligaments could lead to reduced range of motion and increase the likelihood of flexion deformity and medial–lateral instability [37]. According to our experience, a computer-assisted ligament referencing technique such as used with the CAS SCORE® TKA constitutes the most accurate technique to control the ligament and soft tissue balance in relation to a specific mechanical axis intraoperatively. In the current series, no significant difference in terms of clinical scores or final mechanical alignment was detected between MECA and CAS SCORE® TKA. However, this result can be explained by the high-volume experience in conventional mechanical TKA of the two senior surgeons when CAS was introduced at our institution in 2002. In this way, our results were in agreement with those reported by Zhu et al. [40] in a recent randomized clinical trial comparing the outcome of minimally invasive TKA performed with CAS versus conventional mechanical TKA, demonstrating no difference in clinical, radiographic and functional outcome between the two techniques at a 9-year follow-up.
Design of the implants remains an essential parameter in TKA outcome and survivorship, especially for the PF compartment [12, 29]. Along with neutral mechanical axis restoration and equilibrated soft tissue balancing, one of the TKA goals is to restore anatomic parameters such as the PF alignment and tracking [26]. Importantly, Dejour et al. [12] demonstrated, in a biomechanical study, that the femoral component of the SCORE® TKA avoids the mistake of a “dysplasia design” with an optimal trochlear design that reproduces an anatomic, non-dysplastic and asymmetric trochlear groove that is deep, wide and more proximally extended. In addition, Piriou et al. demonstrated that the CAS system used with the SCORE® TKA allowed a reliable and reproducible method for setting the femoral component rotation during TKA with navigation of the femoral trochlea [18, 19, 26, 29]. The femoral component rotation is set intraoperatively when the component trochlea is perfectly super-imposed over the native trochlea on sunrise views at 30°, 60° and 90° of knee flexion during the simulated femoral component planning on the computer. Therefore, the component trochlea is aligned on the native trochlear groove axis which was defined during the trochlear bone morphing. This technique optimises the balance of the medial and lateral patellar retinaculum and helps to balance the arthroplasty PF joint, thus preserving the kinematics of the extensor mechanism. In addition, the CAS system maintains a rectangular medial and lateral flexion gap to avoid ligament laxity in flexion due to the femoral component rotation. Therefore, by reducing rotational mal-alignment, potential negative anatomic and clinical consequences such as anterior knee pain or patellar mal-tracking could be also avoided. In the current series, the survivorship of the SCORE® TKA using secondary patellar resurfacing as an end-point was significantly higher in the CAS group with no revision at 10.5 years after implantation. In the context of selective patellar resurfacing, CAS could improve the restoration of the distal femoral anatomy and important patello-femoral parameters such as the antero-posterior femoral offset, medio-lateral positioning and rotation alignment of the femoral component, and PF balance and tracking.
There are four main limitations to the current study. First, this study could be considered as statistically underpowered. However, this study reported the largest series available in the literature comparing CAS and conventional mechanical TKA with a follow-up of at least 10 years. Second, although comparative, no randomization has been performed pre- or intraoperatively to allocate patients into the MECA or the CAS group. However, no significant difference in the patients’ preoperative status was detected between the two groups (Table 1). Third, 7 and 12 % of the TKA in the CAS and MECA group, respectively, were lost to follow-up despite the prospective follow-up allowed by our institutional total joint registry. Fourth, variability which could affect outcome and survivorship such as slight technical variations between the two senior surgeons was not evaluated in this study though both were high-volume knee surgeons.
Conclusion
With a 91 ± 5 % survivorship using revision for any reason and 100 % survivorship using revision for aseptic loosening as end-points, the cementless ultracongruent rotating mobile-bearing SCORE® TKA demonstrated favourable outcome, long-term fixation and survivorship in patients with primary osteoarthritis without significant influence of CAS at 10-year follow-up. However, CAS might influence TKA survivorship by limiting secondary patellar resurfacing.
References
Bartel DL, Bicknell VL, Wright TM (1986) The effect of conformity, thickness, and material on stresses in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg Am 68:1041–1051
Bassett RW (1998) Results of 1,000 performance knees: cementless versus cemented fixation. J Arthroplasty 13:409–413
Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J (2004) Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br 86:682–687
Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D (2007) Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am 89:261–269
Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, Pitkin R, Rennie D, Schulz KF, Simel D, Stroup DF (1996) Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 276:637–639
Berger RA, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, Rosenberg AG, Galante JO (2001) Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res 392:196–207
Blakeney WG, Khan RJK, Palmer JL (2014) Functional outcomes following total knee arthroplasty: a randomised trial comparing computer-assisted surgery with conventional techniques. Knee 21:364–368
Buechel FF Sr (2002) Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res 404:40–50
Châtain F, Gaillard TH, Denjean S, Tayot O (2013) Outcomes of 447 SCORE® highly congruent mobile-bearing total knee arthroplasties after 5–10 years follow-up. Orthop Traumatol Surg Res 99:681–686
Cheng T, Zhao S, Peng X, Zhang X (2012) Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg Sports Traumatol Arthrosc 20:1307–1322
Cross MJ, Parish EN (2005) A hydroxyapatite-coated total knee replacement: prospective analysis of 1000 patients. J Bone Joint Surg Br 87:1073–1076
Dejour D, Ntagiopoulos PG, Saffarini M (2014) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 22:2599–2607
Dixon MC, Brown RR, Parsch D, Scott RD (2005) Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am 87:598–603
Epinette J, Manley MT (2007) Hydroxyapatite-coated total knee replacement: clinical experience at 10 to 15 years. J Bone Joint Surg Br 89:34–38
Font-Rodriguez DE, Scuderi GR, Insall JN (1997) Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res 345:79–86
Hofmann AA, Evanich JD, Ferguson RP, Camargo MP (2001) Ten- to 14-year clinical followup of the cementless Natural Knee system. Clin Orthop Relat Res 388:85–94
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jenny JY, Boeri C (2004) Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand 75:74–77
Jerosch J, Peuker E, Philipps B, Filler T (2002) Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc 10:194–197
Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K (2007) Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty 22:1097–1106
Matsuda S, White SE, Williams VG, McCarthy DS, Whiteside LA (1998) Contact stress analysis in meniscal bearing total knee arthroplasty. J Arthroplasty 13:699–706
Mont MA, Pivec R, Issa K, Kapadia BH, Maheshwari A, Harwin SF (2013) Long-term implant survivorship of cementless total knee arthroplasty: a systematic review of the literature and meta-analysis. J Knee Surg 27:369–376
O’Rourke MR, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC (2002) Osteolysis associated with a cemented modular posterior-cruciate-substituting total knee design: five to eight-year follow-up. J Bone Joint Surg Am 84:1362–1371
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E (2011) Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am 93:1301–1309
Piriou P, Peronne E, Ouanezar H (2013) Rotational alignment of the femoral component using trochlear navigation during total knee arthroplasty: a dual-center study of 145 cases. J Arthroplasty 28:1107–1111
Quack VM, Kathrein S, Rath B, Tingart M, Lüring C (2012) Computer-assisted navigation in total knee arthroplasty: a review of literature. Biomed Tech 57:269–275
Ranawat CS, Flynn WF, Saddler S, Hansraj KK, Maynard MJ (1993) Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin Orthop Relat Res 286:94–102
Rhoads DD, Noble PC, Reuben JD, Mahoney OM, Tullos HS (1990) The effect of femoral component position on patellar tracking after total knee arthroplasty. Clin Orthop Relat Res 260:43–51
Rodríguez-Merchán EC, Gómez-Cardero P (2010) The outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res 468:1254–1257
Saragaglia D, Picard F, Chaussard C, Montbarbon E, Leitner F, Cinquin P (2001) Computer-assisted knee arthroplasty: comparison with a conventional procedure. Results of 50 cases in a prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot 87:18–28
Saragaglia D, Picard F, Leitner F (2007) An 8- to 10-year follow-up of 26 computer-assisted total knee arthroplasties. Orthopedics 30:S121–S123
Schrøder HM, Berthelsen A, Hassani G, Hansen EB, Solgaard S (2001) Cementless porous-coated total knee arthroplasty: 10-year results in a consecutive series. J Arthroplasty 16:559–567
Sorrells RB, Voorhorst PE, Murphy JA, Bauschka MP, Greenwald AS (2004) Uncemented rotating-platform total knee replacement: a five to twelve-year follow-up study. J Bone Joint Surg Am 86:2156–2162
de Steiger RN, Liu YL, Graves SE (2015) Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty–five years of age. J Bone Joint Surg Am 97:635–642
Varadarajan KM, Rubash HE, Li G (2011) Are current total knee arthroplasty implants designed to restore normal trochlear groove anatomy? J Arthroplasty 26:274–281
Warren PJ, Olanlokun TK, Cobb AG, Walker PS, Iverson BF (1994) Laxity and function in knee replacements. A comparative study of three prosthetic designs. Clin Orthop Relat Res 305:200–208
Watanabe H, Akizuki S, Takizawa T (2004) Survival analysis of a cementless, cruciate-retaining total knee arthroplasty. Clinical and radiographic assessment 10 to 13 years after surgery. J Bone Joint Surg Br 86:824–829
Whiteside LA (2001) Long-term followup of the bone-ingrowth Ortholoc knee system without a metal-backed patella. Clin Orthop Relat Res 388:77–84
Zhu M, Ang CL, Yeo SJ, Lo NN, Chia SL, Chong HC (2015) Minimally invasive computer-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a prospective 9-year follow-up. J Arthroplasty. doi:10.1016/j.arth.2015.11.023
Acknowledgments
The authors thank Mr. Jerôme CRETON for providing assistance in statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HO, FF, AJ and JW declare that they have no conflict of interest. VP declares royalties perceived from Amplitude, Valence, France.
Rights and permissions
About this article
Cite this article
Ouanezar, H., Franck, F., Jacquel, A. et al. Does computer-assisted surgery influence survivorship of cementless total knee arthroplasty in patients with primary osteoarthritis? A 10-year follow-up study. Knee Surg Sports Traumatol Arthrosc 24, 3448–3456 (2016). https://doi.org/10.1007/s00167-016-4112-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4112-3