Abstract
Introduction
Although intramedullary nailing is a popular method for tibiotalocalcaneal arthrodesis, nonunion is one of the most commonly reported complications. This study aimed to evaluate the fusion rate, improvement in functional outcomes, and occurrence of complications in tibiotalocalcaneal arthrodesis using retrograde intramedullary nailing with partial fibulectomy and onlay bone graft technique.
Materials and methods
Twenty-six consecutive patients using the proposed technique were retrospectively reviewed. For radiographic outcomes, the union rate, alignment, and any related complications were assessed. Functional outcomes were evaluated using the American Orthopedic Foot and Ankle Society hindfoot scale, Foot and Ankle Outcome Score, and visual analog scale, preoperatively and at the final follow-up.
Results
The mean follow-up period was 38.2 months. The tibiotalar joint achieved complete union in 80.8% at six months postoperatively, while all the cases achieved complete union at 12 months postoperatively. However, the subtalar joint achieved complete union in 26.9% at six months postoperatively, which gradually increased to 73.1% at 12 months postoperatively, and 80.8% at the final follow-up without revision surgery. A subgroup analysis showed there was a trend of higher subtalar fusion rate when an additional screw for the subtalar joint fixation was placed (86.7% vs. 54.5%). The functional outcomes significantly improved at the final follow-up. A few minor complications occurred, including surgical site infection, irritational symptoms, and metal failure; however, they eventually resolved.
Conclusions
Our technique of tibiotalocalcaneal arthrodesis with partial fibulectomy and onlay bone grafting could be a good option where both the tibiotalar and subtalar joints need to be fused.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibiotalocalcaneal (TTC) arthrodesis is a valuable surgical option for patients with end-stage ankle joint arthritis combined with subtalar joint arthritis. While various surgical procedures and implants have been developed to perform TTC arthrodesis [4, 20], retrograde intramedullary nailing is a popular method [11]. Technical simplicity and great biomechanical stability crossing both the ankle and subtalar joints are considered the advantages of this technique [17].
Despite enormous efforts to develop a stable TTC construct, nonunion at either the tibiotalar or subtalar joint is one of the most commonly reported complications following TTC arthrodesis [11]. According to a meta-analysis of 33 studies analyzing 641 cases of TTC arthrodesis by intramedullary nailing, nonunion was reported in 13.3% [11]. Gross et al. reported a union rate of 86% for the tibiotalar joint and 74% for the subtalar joint with an average follow-up of two years [9]. It was explained that the lower rate of subtalar fusion was due to a lack of compression and subtalar joint preparation. However, even if isolated subtalar arthrodesis is performed, the results are not always favorable, especially when arthrodesis is performed adjacent to the site of a previous ankle arthrodesis [7]. Therefore, it is challenging to achieve successful fusion of both joints, and it is necessary to understand why the subtalar joint has a relatively low fusion rate.
In a previous study, tibiotalar joint arthrodesis using a modified transfibular approach with partial fibular resection and onlay bone graft showed excellent fusion results [15]. They reported that by preserving the posterior half of the distal fibula, the anatomical path of the peroneal tendon can be maintained reducing irritation, and the likelihood of subsequent valgus deformity in the ankle joint can be reduced in cases of nonunion or delayed union. In addition, resected fibula was a good source of bone graft, where none of the patients in their study needed a remote incision for bone graft. As such, we thought of applying the method to TTC arthrodesis, hoping to achieve adequate tibiotalar and subtalar joint fusion. To the best of our knowledge, this is the first report of the short-term clinical outcomes of TTC arthrodesis with retrograde intramedullary nailing combined with partial fibular resection and onlay bone grafting. This study aimed to evaluate the fusion rate of both the tibiotalar and subtalar joints, improvement in functional outcomes, and occurrence of any complications during follow-up. In addition, through further subgroup analysis, we investigated how additional screw fixation affected the subtalar fusion rate. We hypothesized that successful fusion of the tibiotalar and subtalar joints would be achieved, especially with additional subtalar screw fixation, and expected satisfactory clinical outcomes with minimal postoperative complications.
Materials and methods
This retrospective study was approved by our Institutional Review Board (IRB). The requirement for informed consent was waived by IRB owing to the retrospective nature of the study.
We reviewed 30 consecutive patients who underwent TTC arthrodesis using our technique, between November 2016 and December 2020. Patients with end-stage ankle joint arthritis or a history of failed ankle surgery combined with subtalar joint arthritis were included. Four patients were excluded because their follow-up period was less than 12 months. Finally, 26 patients were included in this study. For subgroup analysis, the patients were divided into two groups depending on the presence of additional screws for subtalar joint fixation: 15 patients with subtalar joint fixation (SF) and 11 patients without subtalar joint fixation (WSF). All patients underwent TTC arthrodesis after sufficient conservative treatment, which included taking medications and wearing an ankle brace for over six months. Besides patients with previous failed ankle surgeries, we chose the TTC arthrodesis method over total ankle arthroplasty combined with subtalar joint arthrodesis for the remaining patients because there is a higher likelihood of total ankle arthroplasty failing in the presence of malalignment or poor bone stock of talus. Additionally, the transfibular approach made it easier to prepare both joints.
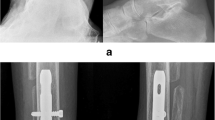
A modified transfibular approach with partial fibular resection and an onlay bone graft technique was adopted in this study [15]. A single longitudinal incision was made over the distal fibula. The distal anterior half of the fibula about 7 cm was marked and resected using an oscillating saw (Fig. 1A). After visualization of the ankle joint, nearby osteophytes were removed. In cases of previous total ankle arthroplasty, removal of the entire implant was performed prior to joint preparation. Following distraction of the joint with a lamina spreader, fusion bed preparations of both tibiotalar and subtalar joints were performed by removing the denudated cartilage using a burr and curette. After meticulous irrigation, feathering using a Hoke osteotome or drilling with a Kirschner wire (K-wire) was performed to enhance fusion between the joints. In this process, a portion of the cancellous subchondral bone was kept between the joint intervals. Alignment was checked under intraoperative fluoroscopy, and the ankle was positioned in a neutral position. To maintain alignment, two temporary K-wires were inserted in parallel from the talus to the tibia posteromedially, and another from the end of the calcaneus, crossing the talus, to the tibia. A guide pin was inserted from the plantar side of the calcaneus, followed by reaming of the intramedullary canal. A 5-degree valgus curved retrograde intramedullary T2™ ankle arthrodesis nail (Stryker, Schönkirchen, Germany) was inserted in all our consecutive cases. Interlocking screws were subsequently placed into the tibia, talus, and calcaneus. An endcap was inserted. Additionally, in the SF group, another 6.0-mm headless compression screw (HCS) was inserted in the oblique direction from the end of the calcaneus towards the anterior talus to fixate the subtalar joint. Two 6.0-mm HCS were inserted from the lateral to the medial side of the tibiotalar joint through the previous two temporary K-wires. After meticulous irrigation, autologous bone grafting at the site of fusion was performed using chopped cancellous bones from the partially resected fibula. An onlay bone graft with a remnant resected fibula was fixed (Fig. 1B), as previously described [15]. Except for one case, there was no need to harvest bone from remote locations like the anterior superior iliac spine. In that one case, after a previously failed total ankle arthroplasty, there was hardly any bone stock left in the talus. Consequently, both femoral allobone graft and autologous iliac bone graft were additionally utilized. Thereafter, the wounds were closed, followed by a compressive dressing with a short leg plaster splint to maintain stability.
The postoperative management protocol followed a course similar to that described in an earlier study [15]. After the swelling of the ankle had subsided, a short leg cast was applied before being discharged from the hospital and maintained for one month postoperatively. Patients were allowed partial weight-bearing (approximately 50%), but were advised to take cautious steps and always use crutches during postoperative one month. The short leg cast was then removed and changed to a short leg Yogips Velcro splint with an ankle brace for another month. Patients were also advised to partially (approximately 50%) bear weight and encouraged to perform a range of motion exercises adjacent to the ankle joints to avoid stiffness until postoperative two months. Then, patients were instructed to fully bear weight with an ankle brace until six months postoperatively and to sustain activities of daily living (ADL).
Serial plain radiographs at six and 12 months postoperatively and at the final follow-up were assessed to check the bony union status. Complete bony union was defined as the presence of trabecular lines between the tibia and the talus or the talus and the calcaneus at the point of contact and the disappearance of the radiolucent line [2]. The partial union was defined as partial osseous bridging formation (< 70%) with a significant radiolucent gap [15]. A subgroup analysis was performed to evaluate the difference in the fusion status of the subtalar joint between the SF and WSF groups at six and 12 months postoperatively. For the assessment of alignment correction, the frontal tibiotalar angle (FTTA) was compared between the preoperative state and the final follow-up [21]. The radiographic parameters were evaluated by two orthopaedic surgeons with experience of 7 years.
Functional outcomes were evaluated based on a survey using the American Orthopedic Foot and Ankle Society (AOFAS) hindfoot scale, Foot and Ankle Outcome Score (FAOS), and visual analog scale (VAS). FAOS is divided into several categories, including symptoms, pain, sports, ADL, and quality of life (QOL). These surveys were conducted on all patients preoperatively and postoperatively at the final follow-up visit.
IBM SPSS Statistics 25 (New York, USA) was used for statistical analysis. The Kolmogorov–Smirnov test was used to determine the normal distribution of the data. The Wilcoxon signed-rank test was performed to evaluate the significant difference between the pre- and postoperative states. Fisher’s exact test was performed to evaluate significant differences in categorical variables between the groups. Statistical significance set at P < 0.05 was considered statistically significant.
Results
The patients’ demographic data are summarized in Table 1. The mean follow-up period was 38.2 (range 12–63) months. Nine patients had a previous history of ankle and/or hindfoot surgery. Three underwent total ankle arthroplasty with Hintegra® (Newdeal, Lyons, France) and converted to TTC arthrodesis after an average of 7.3 years (range 5–11) due to aseptic loosening. Six underwent tibiotalar joint arthrodesis and were revised to TTC arthrodesis after an average of 6.3 years (range 0.8–30) due to painful nonunion.
A representative case of preoperative (Fig. 2A), follow-up radiographs at six months postoperatively (Fig. 2B) and at the final follow-up (Fig. 2C) is shown.
For the tibiotalar joint, the union rate was 80.8% (21 out of 26) at six months postoperatively, while all the cases achieved complete bony union at twelve months postoperatively and at the final follow-up (Fig. 3). However, for the subtalar joint, the union rate was 26.9% (7 out of 26) at six months postoperatively (P < 0.001), which gradually increased to 73.1% (19 out of 26) at twelve months postoperatively (P = 0.010). At the final follow-up, 21 out of 26 patients (80.8%) achieved complete union at the subtalar joint without further surgery (P = 0.051). Four out of the 26 patients (15.4%) achieved complete union after subsequent subtalar revision arthrodesis. Although one patient did not achieve complete fusion even after subsequent subtalar revision arthrodesis, residual symptoms were minimal; therefore, regular follow-up was planned.
A subgroup analysis demonstrated that although there was no significant difference in subtalar joint union rate between SF and WSF groups at six (P = 0.658) and 12 months postoperatively (P = 0.095), there was a trend of higher fusion rate when an additional screw for subtalar joint fixation was placed (86.7% vs. 54.5% at 12 months postoperatively) (Fig. 4).
For the alignment, FTTA changed from 85.3 (range, 67.1–115.2) degrees preoperatively to 89.2 (range, 88–90) degrees postoperatively at the final follow-up (P = 0.135).
Four patients underwent removal of the hardware without revision operation: (1) Surgical site infection occurred in one patient at a follow-up period of 16 months and was treated by removal of all hardware implants and intravenous antibiotics; (2) one patient had symptoms of irritation near the interlocking screws at the proximal nail area, whereas another patient had irritation symptoms in the plantar area near the entry site of the nail. The symptoms subsided after the removal of the implants in these two patients, and (3) one patient complained of unexplained ambiguous pain even after radiographic union. Subsequent hardware removal was performed, and the patient is undergoing follow-up while continuing conservative treatment such as medications and ankle braces.
One patient had a breakage of the intramedullary nail at the subtalar joint level, which was subsequently removed, and revision subtalar arthrodesis was performed. Union of the subtalar joint was eventually achieved at the final follow-up.
Overall FAOS significantly improved at the final follow-up; however, FAOS sports (P = 0.396) did not when compared to the preoperative state (Table 2). The AOFAS hindfoot scale score improved from 40.4 to 64.1 (P < 0.001), while the VAS decreased from 6.2 to 3.1 (P < 0.001).
Discussion
In this study, our technique of TTC arthrodesis using intramedullary nailing combined with partial fibulectomy and onlay bone grafting showed good fusion rates and satisfactory clinical outcomes. In addition, the fusion rate tended to increase when an additional subtalar fixation screw was placed.
The ultimate goal of TTC arthrodesis would be to make a stable TTC construct with good alignment, enabling patients to walk pain-free with a plantigrade foot. However, as this procedure crosses two joints (tibiotalar and subtalar), achieving stable TTC fixation can be challenging. Since Charnley reported a compressive method using an external fixator to perform ankle joint arthrodesis [6], the concept of compression between joints to achieve good fusion has been the basis for the development of various implants. Among these, retrograde intramedullary nails have been widely used for stable arthrodesis [11]. An earlier biomechanical study showed that intramedullary nail fixation was superior to crossed lag screw fixation in terms of overcoming bending and torsional forces, which may help increase the fusion rate [4].
In our study, the union rate for the tibiotalar joint was 80.8% at six months postoperatively, while all the cases achieved complete bony union at 12 months postoperatively and at the final follow-up. This result is comparable to that of the previous study, 74.1% at six months postoperatively, using a modified transfibular technique of tibiotalar joint arthrodesis with partial fibulectomy and onlay bone grafting [15]. Moreover, the union rate at the final follow-up was comparable to those of previous studies [8]. However, for the subtalar joint, the fusion rate was 26.9% at six months postoperatively, which gradually increased to 73.1% at 12 months postoperatively. At the final follow-up, 80.8% achieved complete union without further operation, whereas 15.4% achieved complete union after subsequent subtalar revision arthrodesis. The result of fusion in the first six months may be inferior to that of other studies, as Boer et al. reported an average of 19.8 weeks to achieve fusion [5]. Eventually, our technique demonstrated successful fusion at the subtalar joint as well. In other words, the ankle joint was fused quickly and easily, whereas the subtalar joint was fused relatively slowly and with difficulty. This phenomenon can be explained by previous studies, in that it is not easy to obtain favorable fusion outcomes in the joint adjacent to a previous ipsilateral ankle joint arthrodesis [7, 12]. One possible cause is that as the ankle joint fuses early, leading to a lack of movement at the ankle joint while the remaining movement of the subtalar joint occurs during gait, increased forces are transmitted to the subtalar joint, hindering subtalar union. Another possible reason for the slow initial progress of subtalar fusion could be the early postoperative rehabilitation protocol, which includes partial weight-bearing during postoperative two months. In other previous studies, maintaining non-weight-bearing for more than 6 weeks has been reported [9, 17]. However, the reason we adhered to an earlier rehabilitation protocol is that outcomes following ankle arthrodesis seemed to be similar regardless of the duration of postoperative non-weight-bearing [19], and due to high concerns about complex regional pain syndrome-like changes following surgery and long-term immobilization, as supported by Pepper et al. [18].
We believe that the reason for the successful radiographic outcome in our study was a stable TTC construct. To create a stable TTC construct, a firm fixation, and a good fusion bed are required. In this study, a valgus curved retrograde intramedullary nail with distal and proximal interlocking screws was used for fixation. Those interlocking screws were inserted in static mode, while there were no cases in our series that required dynamization. This was combined with two additional HCS crossing the tibiotalar joint for increasing stability. In addition, in the SF group, placement of an augmentation HCS crossing the subtalar joint enabled favorable union. This supports the fact that the complex motion at the subtalar joint, which includes rotation and translation, or a combination of both [10, 14], renders intramedullary nailing alone insufficient to achieve good subtalar fusion. Although this nail system provides compression at the tibiotalar and talocalcaneal joints, according to a biomechanical study by O’Neill et al., the use of a TTC augmentation screw in addition to an intramedullary nail provided more stable fixation [16]. Moreover, delicate fusion bed preparation at both the tibiotalar and subtalar joints was performed, as Gross et al. pointed out that an inferior result might be related to the omission of subtalar joint fusion bed preparation [9]. Anterior half fibulectomy using the onlay bone graft method was also used to enhance fusion, which enabled cancellous bone-to-cancellous bone contacts between the tibia, fibula, talus, and fibular onlay graft [15].
According to a systematic review by Jehan et al., earlier procedures prior to TTC arthrodesis were reported as high as 48.5%, of which failed total ankle arthroplasty or failed arthrodesis accounted for the majority [11]. In our study, the study subjects included nine patients (34.6%) with previous hindfoot surgery. In one patient, previous hindfoot fusion surgery was performed twice, including tibiotalar joint arthrodesis followed by revision tibiotalar fusion with iliac bone graft. Although these nine cases could be considered as failed ankle surgeries before our TTC arthrodesis, successful radiographic and functional outcomes were demonstrated in the follow-up period. In other words, we believe that TTC arthrodesis using our technique plays a great role as a salvage operation.
Despite its biomechanical advantages, metalwork-related complications are the most common (30.0%) complications following TTC arthrodesis [11]. However, the postoperative complication rate was low in the present study. Only one case of metal failure occurred at the subtalar joint level and required revision subtalar arthrodesis, while the other case included postoperative infection that might be associated with underlying conditions including uncontrolled diabetes, and was treated by removing all hardware implants and administrating intravenous antibiotics. Furthermore, metal irritation at interlocking screw and nail entry sites can often be problematic. Additionally, one patient complained of unexplained ambiguous pain even after radiographic union. Although simple radiographs only showed mild osteopenia in the tibia with no other significant findings, we suspected that the intramedullary nail might be contributing to the stress-shielding effect. As a result, the removal of the whole implant was performed. Previous studies have shown that the presence of a prosthesis alters stress loading on the native bone, which leads to bone resorption and reduced bone mass in areas of decreased loading [13]. Allen Jr. et al. also reported that retained intramedullary nails have been associated with stress shielding and an overall decrease in bone mineral density of the tibia [3]. Since bone resorption is frequently associated with pain [22], it is possible that it also caused pain in this patient. Although dual-energy X-ray absorptiometry was not performed in this study, future studies focusing on the bone mineral density near the implant will be of great help in determining the stress-shielding effect of intramedullary nails. Therefore, patients undergoing TTC arthrodesis should be informed in advance that metal-related complications may occur during follow-up.
Functional outcomes showed significant improvements in the overall questionnaires. This result is comparable to those of previous studies showing AOFAS scores of 66.5 and VAS of 2.8 [1]. However, regarding why there was no significant increase in FAOS sports, patients with a mean age of 65.1 years who underwent TTC arthrodesis would have lived with severe chronic hindfoot pathology, and thus participation in sports activities would have been low even postoperatively. Furthermore, in sports activities, not only the motion of the ankle joint but also that of the subtalar joint may be important. As such, the fused state of both the tibiotalar and subtalar joints may be uncomfortable for patients participating in sports activities. Nonetheless, our study showed favorable functional outcomes, including ADL and QOL.
This study has several limitations. First, this study was retrospective, and a small number of patients were included. Due to the lack of a sufficient number of study subjects, statistically significant differences between the SF and WSF groups were not observed. A prospective randomized cohort study with a large number of subjects is needed to confirm the merit of additional subtalar fixation. Second, the follow-up period and diagnoses of patients were heterogeneous. Therefore, analysis could not be performed between subgroups. However, as TTC arthrodesis tends to be offered to patients with severe hindfoot pathologies with various causes as a limb salvage procedure [1], we believe our study’s comparable results, with a lower complication rate, will be helpful. Lastly, from the perspective of radiographic measurement, the union status was evaluated solely based on plain radiographs, and the assessment of alignment before and after surgery was only confirmed by the FTTA.
Conclusion
TTC arthrodesis with retrograde intramedullary nailing combined with partial fibular resection and onlay bone grafting had comparable radiographic and clinical outcomes with less complication rate. A higher fusion rate of the subtalar joint was achieved with additional subtalar joint fixation. We believe that our method of TTC arthrodesis is a good option where both the tibiotalar and subtalar joints need to be fused.
Data availability
The datasets used and aalyzed during the current study are available from the corresponding author on reasonable request.
References
Ajis A, Tan KJ, Myerson MS (2013) Ankle arthrodesis vs TTC arthrodesis: patient outcomes, satisfaction, and return to activity. Foot Ankle Int 34(5):657–665. https://doi.org/10.1177/1071100713478929
Akra GA, Middleton A, Adedapo AO, Port A, Finn P (2010) Outcome of ankle arthrodesis using a transfibular approach. J Foot Ankle Surg 49(6):508–512. https://doi.org/10.1053/j.jfas.2010.07.004
Allen JC Jr, Lindsey RW, Hipp JA, Gugala Z, Rianon N, LeBlanc A (2008) The effect of retained intramedullary nails on tibial bone mineral density. Clin Biomech (Bristol, Avon) 23(6):839–843. https://doi.org/10.1016/j.clinbiomech.2008.02.003
Berend ME, Glisson RR, Nunley JA (1997) A biomechanical comparison of intramedullary nail and crossed lag screw fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 18(10):639–643. https://doi.org/10.1177/107110079701801007
Boer R, Mader K, Pennig D, Verheyen CC (2007) Tibiotalocalcaneal arthrodesis using a reamed retrograde locking nail. Clin Orthop Relat Res 463:151–156. https://doi.org/10.1097/BLO.0b013e31814fb1bb
Charnley J (1951) Compression arthrodesis of the ankle and shoulder. J Bone Joint Surg Br 33B(2):180–191
Easley ME, Trnka HJ, Schon LC, Myerson MS (2000) Isolated subtalar arthrodesis. J Bone Joint Surg Am 82(5):613–624. https://doi.org/10.2106/00004623-200005000-00002
Franceschi F, Franceschetti E, Torre G et al (2016) Tibiotalocalcaneal arthrodesis using an intramedullary nail: a systematic review. Knee Surg Sports Traumatol Arthrosc 24(4):1316–1325. https://doi.org/10.1007/s00167-015-3548-1
Gross JB, Belleville R, Nespola A et al (2014) Influencing factors of functional result and bone union in tibiotalocalcaneal arthrodesis with intramedullary locking nail: a retrospective series of 30 cases. Eur J Orthop Surg Traumatol 24(4):627–633. https://doi.org/10.1007/s00590-013-1347-2
Jastifer JR, Gustafson PA (2014) The subtalar joint: biomechanics and functional representations in the literature. Foot (Edinb) 24(4):203–209. https://doi.org/10.1016/j.foot.2014.06.003
Jehan S, Shakeel M, Bing AJ, Hill SO (2011) The success of tibiotalocalcaneal arthrodesis with intramedullary nailing–a systematic review of the literature. Acta Orthop Belg 77(5):644–651
Jennison T, Dalgleish J, Taher S et al (2022) Subtalar arthrodesis union rates with and without adjacent ankle arthrodesis. Foot Ankle Int 43(10):1295–1299. https://doi.org/10.1177/10711007221110873
Keogh CF, Munk PL, Gee R, Chan LP, Marchinkow LO (2003) Imaging of the painful hip arthroplasty. Am J Roentgenol 180(1):115–120. https://doi.org/10.2214/ajr.180.1.1800115
Krahenbuhl N, Horn-Lang T, Hintermann B, Knupp M (2017) The subtalar joint: A complex mechanism. EFORT Open Rev 2(7):309–316. https://doi.org/10.1302/2058-5241.2.160050
Lee DY, Kyung MG, Cho YJ, Hwang S, Kang HW, Lee DO (2020) A modified transfibular technique of ankle arthrodesis using partial fibular resection and onlay bone graft. PLoS ONE 15(10):e0241141. https://doi.org/10.1371/journal.pone.0241141
O’Neill PJ, Parks BG, Walsh R, Simmons LM, Schon LC (2007) Biomechanical analysis of screw-augmented intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int 28(7):804–809. https://doi.org/10.3113/FAI.2006.0804
Pelton K, Hofer JK, Thordarson DB (2006) Tibiotalocalcaneal arthrodesis using a dynamically locked retrograde intramedullary nail. Foot Ankle Int 27(10):759–763. https://doi.org/10.1177/107110070602701001
Pepper A, Li W, Kingery WS, Angst MS, Curtin CM, Clark JD (2013) Changes resembling complex regional pain syndrome following surgery and immobilization. J Pain 14(5):516–524. https://doi.org/10.1016/j.jpain.2013.01.004
Potter MJ, Freeman R (2019) Postoperative weightbearing following ankle arthrodesis: a systematic review. Bone Joint J. 101-B(10):1256–1262. https://doi.org/10.1302/0301-620X.101B10.BJJ-2019-0207.R1
Prissel MA, Simpson GA, Sutphen SA, Hyer CF, Berlet GC (2017) Ankle arthrodesis: a retrospective analysis comparing single column, locked anterior plating to crossed lag screw technique. J Foot Ankle Surg 56(3):453–456. https://doi.org/10.1053/j.jfas.2017.01.007
Willegger M, Holinka J, Nemecek E et al (2016) Reliability of the radiographic sagittal and frontal tibiotalar alignment after ankle arthrodesis. PLoS ONE 11(4):e0154224. https://doi.org/10.1371/journal.pone.0154224
Zhen G, Fu Y, Zhang C et al (2022) Mechanisms of bone pain: progress in research from bench to bedside. Bone Res 10(1):44. https://doi.org/10.1038/s41413-022-00217-w
Funding
This study was supported by a grant (NRF-2016R1D1A1B02009379) from the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education. The funding source did not have a role in the study design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
MGK and IH: participated in the data collection, performed data analysis, provided the interpretation, conception and design of the study, and drafted the manuscript. CL and GYP: participated in the data collection and performed data analysis. DYL: participated in the conception and design of the study, and as well as data interpretation. All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This research ethics was approved by the Seoul National University Hospital Institutional Review Board (IRB Number: H-1806–151-953). This study was carried out in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
The need for informed consent was waived by the Institutional Review Board owing to the retrospective design of the study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kyung, M.G., Hwang, IU., Lee, C. et al. Clinical outcomes following tibiotalocalcaneal arthrodesis with intramedullary nailing combined with partial fibulectomy and onlay bone graft. Arch Orthop Trauma Surg 144, 567–574 (2024). https://doi.org/10.1007/s00402-023-05097-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05097-1