Abstract
Background
Learning curves associated with independent practice and anterior approach total hip arthroplasty (AA-THA) has been associated with inferior outcome. This study compared outcome of junior, fellowship-trained, surgeons who perform THA through both anterior and posterior (PA) approach, with senior surgeons who perform either AA or PA, to determine whether: 1. Fellowship training and selective practice allows for safe introduction of AA into practice; and 2. Whether selective approach-use influences outcome.
Methods
This is a prospective, consecutive study comparing the first 800 THAs of two junior, dual-approach, surgeons (AA/PA: 455/345), with 400 THAs cases of two senior, single-approach, surgeons (AA/PA: 200/200), between 2018 and 2020. Most patients were female (54.4%), mean age was 65 years-old (range 19–96) and mean BMI was 29 kg/m2 (range 16–66). Outcome included radiologic measurements (inclination/anteversion and leg-length), complication- and revision rates, and patient-reported outcomes including Oxford Hip Score (OHS).
Results
At 3.1 years (range 2.0–6.8) follow-up, there were 43 complications (3.6%), including 27 re-operations (2.3%); with no difference between junior and senior surgeons for AA-THA (Junior: 8/455 vs. Senior: 3/200; p = 0.355) or PA-THA (Junior: 11/345 vs. Senior: 5/200; p = 0.400). Amongst juniors, there was no difference in complications (AA:8/455 vs. PA:11/345; p = 0.140) and in ΔOHS (AA:20.5 ± 7.7 vs. PA:20.5 ± 8.0; p = 0.581) between approaches.
Conclusion
Contemporary training and selective approach-use minimizes the learning curve, allowing junior staff to have equivalent outcome to established, senior surgeons in both AA and PA. We would advocate for selective approach use amongst junior arthroplasty surgeons when introducing the AA into independent practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The three most common approaches for Total hip arthroplasty (THA) include the posterior (PA), direct lateral, and anterior (AA), with well-documented advantages and disadvantages for each [1, 2]. The AA has gained popularity, because it is an inter-nervous and inter-muscular approach, offering presumed advantages such as enhanced recovery, decreased postoperative pain, and decreased dislocation rates [3,4,5,6]. However, several studies have failed to show a distinct advantage of AA over PA [1, 2, 7, 8]. In fact, opponents of AA have reported higher rates of complications associated with AA [9,10,11,12]. It is thought that higher complication rates after AA are associated with its learning curve [13]. Based on registry data, the AA’s learning curve is between 50 and 100 cases, [13] with complication rates reported at 7–44% during the introductory phase [14]. Limited data exists as to (1) whether fellowship training and selective practice allows for safer introduction of AA into practice and (2) whether selective approach-use influences outcome.
This study aims to compare outcome (reconstruction, complications, reoperations, and patient-reported outcome scores) of the first THAs of junior, fellowship-trained, surgeons who perform THA through both (AA and PA) approaches, and of THAs performed by senior surgeons who perform THA exclusively through either AA or PA. We hypothesized that fellowship training and selective choice of approach reduces risk of complications with AA-THA, seen in the beginning of independent practice amongst junior surgeons, and that their outcome would be equivalent to senior surgeons.
Methods
Study design
This is prospective, IRB-approved, consecutive, longitudinal cohort study from two academic tertiary referral centers (The Ottawa Hospital, Ottawa Ontario, Canada & Mayo Clinic, Phoenix, Arizona, United States). Outcomes were compared between two junior and two senior surgeons for respectively AA and PA-THA, as well as between approaches.
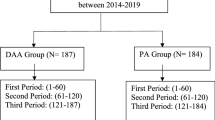
A sample size calculation was performed in SPSS v28 (IBM Corp, New York, United States). Previous studies have shown a complication rate of 13% in the early stage of the AA learning curve [15], whilst an incidence of 3% has been described among experienced surgeons [16]. Based on this data, a minimum of 188 cases per group was needed to achieve sufficient power (1-β = 0.95, α = 0.05).
Surgeon training & practice
Junior surgeons were fellowship-trained staff in the first 2 years of independent practice. Prior to starting independent practice, one junior surgeon had been involved in over 350 PA-THA and 150 AA-THA; during his residency training he had been utilizing the posterior approach for THAs, exclusively. He underwent his fellowship in a tertiary care unit with a high volume of THAs performed with AA-THA. The other junior surgeon also underwent arthroplasty fellowship training and had been involved in 300 posterolateral or direct lateral approaches and 130 AA-THA during residency and fellowship training.
Both senior surgeons were staff in the respective tertiary referral centers with a minimum of 10 years’ experience, and exclusively (> 98% of cases) use either AA or PA for primary THA [17].
Study population
Between January 1st, 2018 and December 31st, 2020, the first 400 THAs of the two junior, dual-approach, surgeons (AA/PA: 455/345) (751 patients) were compared with 400 consecutive THAs (AA/PA: 200/200) (386 patients) of two senior, single-approach, surgeons operated in the same period.
There were 547 males (45.6%) and 653 females (54.4%), with a mean Body Mass Index (BMI) of 29.2 ± 5.8 kg/m2. Mean age of the cohort was 65.0 ± 11.7 years, with a mean follow-up of 3.1 ± 0.7 years. Patients that underwent THA by junior surgeons were on average younger (64.0 ± 12.5 vs. 66.8 ± 9.4 years; p < 0.001) and had higher BMI (30.7 ± 5.7 vs. 28.4 ± 5.8 kg/m2; p < 0.001) (Table 1). Patients that underwent AA-THA had lower BMI in comparison to those that underwent PA-THA (28.0 ± 5.1 vs. 30.7 ± 6.2 kg/m2; p < 0.001). Primary osteoarthritis (OA) was the indication in 1,067 (88.9%) hips, followed by secondary OA due to dysplasia (3.2%; n = 38); hip fracture (3.5%; n = 42); avascular necrosis of the femoral head (3.2%; n = 38), tumor metastasis (0.9%; n = 11) and failed open reduction, internal fixation (0.4%; n = 5).
Surgical technique
The choice of approach was based on patient anatomy, weight, body shape and individual patient wishes. PA was favored in patients with greater abdominal girth overlying incision (grade ≥ 2 abdominal pannus), obesity (BMI ≥ 35), and in those with secondary osteoarthritis (e.g. acetabular dysplasia Crowe grade ≥ 2, history of Legg-Calve-Perthes disease or Slipped-Capital avascular necrosis due to sickle cell anemia, juvenile arthritis, conversion of failed fixation of a previous fracture).
AA-THAs were performed with patients positioned supine on a standard operating table (n = 455) [4] or using a positioning table (n = 228) [16], and through horizontal ‘bikini’ incision (n = 227) or longitudinal incision (n = 428). Anterior capsule was preserved and subsequently repaired in 227 cases. The ‘bikini’ incision and capsular repair technique was exclusively used by one of the junior surgeons. Intraoperative fluoroscopy was used in 455 AA-THAs to assist in component positioning. Patients were allowed weight-bearing as tolerated post-operatively without any anterior/posterior hip precautions.
All PAs were performed with patients in a lateral decubitus position [18]. External rotators and posterior capsule were taken down and repaired after the procedure in a standard fashion. Gluteus maximus tendon was not released in any of the cases. No intra-operative fluoroscopy was used in PA-THA. Patients were allowed weight-bearing as tolerated with posterior hip precautions during the first 6 weeks.
Most used acetabular implants were G7® (Zimmer-Biomet, Warsaw, Indiana, United States) (n = 487), Trident® cup (Stryker, Kalamazoo, Michigan, United States) (n = 496), CSF® (JRI Orthopaedics, Sheffield, United Kingdom) (n = 98), and Trilogy® (Zimmer-Biomet) (n = 96). Most commonly used femoral stems were Accolade 2® (Stryker) (n = 462), Microplasty® (Zimmer-Biomet) (n = 339), Alloclassic® (Zimmer-Biomet) (n = 98), and Furlong® Evolution (JRI Orthopaedics) (n = 97). Most stems were uncemented (92.5%). Cemented stems were used more often in PA-THA (30.1% vs. 2.6%; p < 0.001), and by junior surgeons (10.9% vs. 1.0%; p < 0.001), who would tend to use cemented implants in cases of poor bone quality and hip fractures, in line with national recommendations [19]. Articulating bearing surface was metal-on-polyethylene (52.2%) or ceramic-on-polyethylene (47.8%).
Radiographic measurements
Anteroposterior (AP) pelvic radiographs were obtained at 3-months and 1-year postoperatively, and annually thereafter. Radiographic measurements were performed by two fellowship-trained arthroplasty surgeons (GG & JB) using Picture Archiving Communication System (PACS) (Change Healthcare, Nashville, United States) and Ein-Bild-Röntgen-Analyse (EBRA-cup®) (University of Innsbruck, Innsbruck, Austria). Leg length discrepancy (LLD) was measured [20], as well as acetabular cup inclination and anteversion [21]. The optimum orientation zone was defined as 40° ± 10° inclination and 20° ± 10° anteversion [22]. Average-measure correlation coefficients with a two-way random effects model for absolute agreement was calculated, showing excellent intra- and inter-observer reliabilities (range 0.901 (95% CI 0.705–0.969) to 0.932 (95% CI 0.796–0.979).
Clinical outcome measurements
Outcome measures included surgical related intra-operative and post-operative complications, and reoperations. The Clavien-Dindo classification was used to grade complications [23, 24]. To assess the learning curve of the junior surgeons, complication rates of their first 100 cases was compared to their second 100 cases.
Patient-reported outcome measures (PROMs) were obtained pre-operatively, and at a minimum of 12 months post-operatively, including Oxford Hip Score (OHS) (0–48; worse to best) [25] and EuroQOL Five Dimensions Questionnaire (EQ5D) (-0.594 to 1.000; worse to best) [26]. The difference between the latest follow-up and the pre-operative PROM values was defined as Δ, and the meaningful clinically important difference (MCID) for the OHS is 5 points [27].
Statistics
Statistical analysis was performed using SPSS v27 (IBM Corp, New York, United States). Normal distribution of data was tested with the Kolmogorov–Smirnov test and Q-Q plots. A Mann Whitney U test or a Kruskal–Wallis was used to compare continuous variables between different groups, for non-normally distributed data and a Chi Square test to compare categorical variables. A p-value of < 0.05 was considered to indicate statistical significance.
Results
Radiographic measurements
Mean post-operative leg-length difference was 1.0 ± 2.0 mm with a mean cup inclination of 42.0° ± 5.5° and anteversion of 24.3° ± 5.4°, and 84.2% of cups were positioned in the optimal orientation zone (Table 2). Junior surgeons had more cups within this zone than senior surgeons (90.0% vs. 73.9%; p < 0.001), with the difference being the greatest in AA-THA (91.8 vs. 57.1%; p < 0.001).
Amongst juniors, there was no difference in cup positioning between AA-THA and PA-THA (inclination: 42.2° ± 4.4° vs. 42.2° ± 5.8°; p = 0.245 & anteversion: 23.1° ± 4.9° vs. 22.8 ± 4.9°; p = 0.266), and a same proportion of cups within the optimal orientation zone (91.8% vs. 87.4%; p = 0.106).
Complications and reoperations
At a mean follow-up of 3.1 ± 0.7 years, overall complication rate 3.6% (n = 43/1,200). Clavien-Dindo grade 3 complications were seen in 2.3% (27/1,200) of this cohort, and 1.8% implants were revised (22/1,200). The majority of revisions were peri-prosthetic joint infection (PJI) (9/1200; 0.8%), followed by instability (8/1200; 0.7%) and peri-prosthetic fractures (4/1200; 0.3%) (Table 2).
There was no difference in overall complication rate between junior and senior surgeons with AA-THA (Junior: 14/455; 3.1% vs. Senior: 4/200; 2.0%; p = 0.312) or PA-THA (Junior: 20/345; 5.8% vs. Senior: 5/200; 2.5%; p = 0.076). Similarly, no difference in re-operation (AA-THA: p = 0.355; PA-THA; p = 0.400), or revision (AA-THA: p = 0.462; PA-THA; p = 0.589) was detected between surgeon groups for each approach. There were more dislocations with PA-THA (7/545; 1.3%) than with AA-THA (1/655; 0.2%) (p = 0.019), with no difference between junior (3/345; 0.9%) and senior (4/200; 2.0%) surgeons (p = 0.227).
In the first 200 AA-THA cases of the junior surgeons (100 each), there were 9 complications (4.5%), of which 6 (3.0%) were grade 2, all wound-related problems that resolved with a course of antibiotics; and 3 were grade 3 (1.5%), including one dislocation, one periprosthetic fracture and one early stem loosening. Revision rate after the first 100 cases for each junior surgeon was 1.5%, whilst revision rate for the remaining 245 reported was 0.8% (p = 0.358).
Patient-reported outcome measures
Mean ΔOHS was 20.6 ± 7.9. There was no difference in pre-operative OHS between AA-THA and PA-THA patients (18.7 ± 6.9 vs. 17.5 ± 5.2; p = 0.198), but AA-THA patients had slightly higher ∆OHS (21.3 ± 8.3 vs. 19.6 ± 7.2; p < 0.001) (Table 2).
Patients that underwent THA by junior surgeons had lower pre-operative OHS (17.8 ± 6.1 vs. 18.8 ± 6.3; p = 0.008), but a similar ∆OHS (20.5 ± 7.8 vs. 20.8 ± 8.2; p = 0.657), than those operated by senior surgeons.
Amongst juniors, there was no difference in pre-operative OHS (AA-THA: 18.0 ± 6.2 vs. 17.5 ± 6.0; p = 0.912), nor in ΔOHS (AA:20.5 ± 7.7 vs. PA:20.5 ± 8.0; p = 0.581), between approaches (Fig. 1).
OHS scores were different between institutions, both pre-operatively (17.9 ± 3.6 vs. 19.5 ± 8.8; p = 0.038) and at latest follow-up (36.0 ± 4.1 vs. 43.7 ± 5.2; p < 0.001).
Discussion
The optimum approach for THA is a matter of continuous debate and is likely surgeon- and patient- dependent. Furthermore, how to implement ones’ training into the beginning of practice may further complicate this decision. Particularly, AA is associated with a long learning curve and high complication risk during introduction into practice [10, 15]. In this prospective study we report the outcome of two newly appointed staff surgeons, with contemporary, dual-approach, training experiences and practice implementations of selective (anterior or posterior) approach for primary THA; and compared their outcomes with those of experienced surgeons who predominantly use a single (either anterior or posterior) approach. AA was more commonly offered to patients with a lower BMI and those with primary osteoarthritis, as AA can often be more challenging and associated with technical difficulties in other patients [28, 29]. At 3 years follow-up, the overall complication- and revision- rates were 3.6% and 2.3% respectively, without differences between junior and senior surgeons when analyzed as per approach, and with similar clinical improvement. Furthermore, the selection process of what approach to use by the junior surgeons, was not associated with an increased incidence of adverse outcomes. Outcomes were superior to historic reports on introduction of AA to surgical practice [9, 30, 31]. This is encouraging, especially when one considers that these results are in the presence of challenges associated with independent practice and use of AA. Therefore, this study shows that contemporary training and selective approach-use helps minimizing complication risk during the learning curve associated with independent practice and AA, allowing junior staff to have equivalent outcomes to established, senior surgeons in both approaches.
AA may offer certain advantages [1, 32], however, opponents have criticized AA-THA because of its technical difficulty, leading to complications [33]. There is no level 1 evidence to support one approach over the other, especially in higher risk patients (e.g. those with high BMI, overlying abdominal pannus, secondary osteoarthritis or abnormal anatomy). It is intuitively logical that an easier extensile approach, such as the posterior approach, would be more likely the approach of choice, especially amongst surgeons that are not experienced with AA. In this study, revision rate after the first 100 cases for each junior surgeon was 1.5%, whilst revision rate for the remaining 245 reported was 0.8%, indicating that with selective use, the learning curve had a smaller effect on patients compared to the previously reported learning curve figures of 7–44% [14]. We would therefore advocate selective AA use amongst junior surgeons when introducing the AA into practice. During contemporary training, young surgeons are likely to encounter both anterior and posterior approaches. Junior surgeons involved in this study received dedicated fellowship training in tertiary referral centers with a high volume of AA-THA and had each been involved in over 300 PA-THA and 150 AA-THA before starting practice. Given that the introduction of the AA took place during residency/fellowship training, the results of the first few 200 cases as staff do not reflect their learning curve with the AA, rather the learning curve of the introduction of the AA into independent practice.
By collecting surgical outcomes of THA performed by senior, established surgeons, we were able to create important benchmarks for quality of care delivered for each approach. Among junior surgeons, there was a high accuracy to reconstruct the hip, with no difference between approaches. Equally importantly, there were no differences in the complication- and revision-rates, nor the clinically important differences in PROMs between seniority levels. We did notice subtle difference in PROMs between groups, which might reflect cohort-biases. The AA-senior surgeon had higher OHS pre- and post- THA, and a slightly higher ∆OHS. This is also due to patients in one institution having lower pre- and post-operative scores. Previous work has shown that a higher pre-THA OHS is likely to lead to superior improvement (ΔOHS), as seen in this study [29].
Selective approach for THA may lead to unfavorable outcomes for some patients. It was thus of value to compare outcomes for the surgeons with such practice. The choice of approach was at the discretion of the surgeon. Therefore, selection biases may exist; with more complex cases having been performed with PA. There were no differences in reconstruction, revision- rates, nor PROMs between AA- and PA-THAs amongst junior staff. It is thus arguable that appropriate patient selection was undertaken, and no patients were placed at undue risk during this early phase of independent surgical practice. However, higher re-operation risk was seen among PA-THA patients, with a significantly higher incidence of instability in PA-THA. While this can be partially attributed to the selection of complex cases for PA-THA, there was also a higher incidence of instability after PA-THA among senior surgeons, in coherence with previous reports [1].
This study is not without limitations. Firstly, this is the experience of two surgeons and the training and abilities of every surgeon is unique, as such these results are not necessarily transferrable. Both surgeons received contemporary training in AA-THA and the learning curve here would not apply to surgeons learning the technique for the first time. Furthermore, both surgeons were appointed in high-volume hip arthroplasty centers, and previous reports have suggested that the learning curve might be shorter in a high-volume centers [34]. Secondly, mean follow-up was only 3 years, these short-term outcomes should not be directly compared to other studies using long-term outcomes. Thirdly, the approach chosen for each patient in this study was at the discretion of the treating surgeon, and as such these outcomes may not be comparable to those that exclusively use AA-THA, and other surgeons might maintain different criteria. However, this study was focusing on surgeons that utilize two approaches in practice and thus selection biases would be unavoidable. Fourthly, a variability in used implants was present among surgeons between different centers, which was the consequence of the multi-center design of the study, and junior surgeons adhering to a unit’s standard of practice upon commencing practice, using similar implants as the ones predominantly used by the other surgeons in the unit, reflecting common clinical practice.
Conclusion
Contemporary training and selective approach-use minimizes the learning curve associated with independent practice and AA-THA allowing junior staff to have equivalent outcomes to established, senior surgeons in both approaches. We would thus advocate for selective approach use amongst junior arthroplasty surgeons when introducing the AA into practice. It should however be noted that surgeons in this study considered patient factors including BMI and bone morphology when choosing the ideal surgical approach, and that one surgical approach may not be right for every patient.
References
Higgins BT, Barlow DR, Heagerty NE, Lin TJ (2015) Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty 30(3):419–434
Yue C, Kang P, Pei F (2015) Comparison of direct anterior and lateral approaches in total hip arthroplasty: a systematic review and meta-analysis (PRISMA). Medicine 94(50):e2126
Chechik O, Khashan M, Lador R, Salai M, Amar E (2013) Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg 133(11):1595–1600
Corten K, Holzapfel BM (2021) Direct anterior approach for total hip arthroplasty using the “bikini incision.” Oper Orthop Traumatol 33(4):318–330
Barrett WP, Turner SE, Leopold JP (2013) Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty 28(9):1634–1638
Sibia US, Turner TR, MacDonald JH, King PJ (2017) The impact of surgical technique on patient reported outcome measures and early complications after total hip arthroplasty. J Arthroplasty 32(4):1171–1175
Lee GC, Marconi D (2015) Complications following direct anterior hip procedures: costs to both patients and surgeons. J Arthroplasty 30(9 Suppl):98–101
Taunton MJ, Trousdale RT, Sierra RJ, Kaufman K, Pagnano MW (2018) John Charnley award: randomized clinical trial of direct anterior and miniposterior approach THA: which provides better functional recovery? Clin Orthop Relat Res 476(2):216–229
Angerame MR, Fehring TK, Masonis JL, Mason JB, Odum SM, Springer BD (2018) Early failure of primary total hip arthroplasty: is surgical approach a risk factor? J Arthroplasty 33(6):1780–1785
Spaans AJ, van den Hout JA, Bolder SB (2012) High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop 83(4):342–346
Müller DA, Zingg PO, Dora C (2014) Anterior minimally invasive approach for total hip replacement: five-year survivorship and learning curve. Hip Int 24(3):277–283
Christensen CP, Karthikeyan T, Jacobs CA (2014) Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty 29(9):1839–1841
de Steiger RN, Lorimer M, Solomon M (2015) What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res 473(12):3860–3866
Nairn L, Gyemi L, Gouveia K, Ekhtiari S, Khanna V (2021) The learning curve for the direct anterior total hip arthroplasty: a systematic review. Int Orthop 45(8):1971–1982
Woolson ST, Pouliot MA, Huddleston JI (2009) Primary total hip arthroplasty using an anterior approach and a fracture table: short-term results from a community hospital. J Arthroplasty 24(7):999–1005
Matta JM, Shahrdar C, Ferguson T (2005) Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 441:115–124
Gofton WT, Ibrahim MM, Kreviazuk CJ, Kim PR, Feibel RJ, Beaulé PE (2020) Ten-year experience with the anterior approach to total hip arthroplasty at a tertiary care center. J Arthroplasty 35(5):1281–9.e1
Browne JA, Pagnano MW (2012) Surgical technique: a simple soft-tissue-only repair of the capsule and external rotators in posterior-approach THA. Clin Orthop Relat Res 470(2):511–515
National Institute for Health and care Excellence (NICE) (2011) Hip fracture: management. www.nice.org.uk/guidance/cg124. Accessed 2 Nov 2022
Nossa JM, Muñoz JM, Riveros EA, Rueda G, Márquez D, Pérez J (2018) Leg length discrepancy after total hip arthroplasty: comparison of 3 intraoperative measurement methods. Hip Int 28(3):254–258
Park YS, Shin WC, Lee SM, Kwak SH, Bae JY, Suh KT (2018) The best method for evaluating anteversion of the acetabular component after total hip arthroplasty on plain radiographs. J Orthop Surg Res 13(1):66
Grammatopoulos G, Alvand A, Monk AP, Mellon S, Pandit H, Rees J et al (2016) Surgeons’ accuracy in achieving their desired acetabular component orientation. J Bone Joint Surg Am 98(17):e72
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Wells J, Schoenecker P, Petrie J, Thomason K, Goss CW, Clohisy JC (2019) Are complications after the bernese periacetabular osteotomy associated with subsequent outcomes scores? Clin Orthop Relat Res 477(5):1157–1163
Wylde V, Learmonth ID, Cavendish VJ (2005) The Oxford hip score: the patient’s perspective. Health Qual Life Outcomes 3:66
EuroQol Group (1990) EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208
Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ et al (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68(1):73–79
Hartford JM, Knowles SB (2016) Risk factors for perioperative femoral fractures: cementless femoral implants and the direct anterior approach using a fracture table. J Arthroplasty 31(9):2013–2018
Watts CD, Houdek MT, Wagner ER, Sculco PK, Chalmers BP, Taunton MJ (2015) High risk of wound complications following direct anterior total hip arthroplasty in obese patients. J Arthroplasty 30(12):2296–2298
Hartford JM, Bellino MJ (2017) The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon’s first 500 cases. Hip Int 27(5):483–488
Barnett SL, Peters DJ, Hamilton WG, Ziran NM, Gorab RS, Matta JM (2016) Is the anterior approach safe? early complication rate associated with 5090 consecutive primary total hip arthroplasty procedures performed using the anterior approach. J Arthroplasty 31(10):2291–2294
Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH et al (2018) A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 13(1):229
Meermans G, Konan S, Das R, Volpin A, Haddad FS (2017) The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 99-b(6):732–740
Seng BE, Berend KR, Ajluni AF, Lombardi AV Jr (2009) Anterior-supine minimally invasive total hip arthroplasty: defining the learning curve. Orthop Clin North Am 40(3):343–350
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest directly related to this study. Separate conflict of interest forms for each author have been uploaded.
Institutional review board
This study was approved by the Institutional Review Board of the institution and all patients signed an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verhaegen, J.C.F., Ojaghi, R., Kim, P. et al. Selective THA-approach use amongst junior surgeons improves safety of introducing the anterior approach: a prospective, multi-surgeon, comparative, study. Arch Orthop Trauma Surg 143, 6829–6836 (2023). https://doi.org/10.1007/s00402-023-04895-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04895-x