Abstract
Introduction
To report clinical and radiographic outcomes of revision total hip arthroplasty (THA) through the direct anterior approach (DAA) using primary stems.
Materials and methods
The authors assessed a consecutive series of revision THAs operated by DAA using primary (cemented and uncemented) stems between 1/1/2010 and 30/06/2017. The initial cohort comprised 47 patients (50 hips), aged 65 ± 10 years with BMI of 25 ± 4 kg/m2. Clinical assessment included modified Harris Hip Score (mHHS) and satisfaction with surgery. Radiographic assessment included radiolucent lines > 2 mm, bone remodelling, cortical hypertrophy, pedestal formation, and osteolysis. Linear regression analyses were performed.
Results
Of the 50 hips (47 patients) in the initial cohort, intraoperative complications that did not require re-revision occurred in 5 hips. At a follow-up of > 2 years: 5 hips (10%) were lost to follow-up and 3 hips (6%) required stem re-revision, leaving a final cohort of 42 hips (40 patients). Postoperative complications that did not require re-revision occurred in 4 hips (8%). At 4.3 ± 1.6 years, post-revision mHHS was 89 ± 14 (range 47–100) and 38 patients were satisfied or very satisfied with revision surgery. Bone remodelling was observed in 8 hips (16%), cortical hypertrophy in 6 hips (12%), grade I heterotopic ossification in 7 hips (14%), and grade II in 1 hip (2%). There were no cases of radiolucent lines, pedestal formation, or osteolysis. Regression analyses revealed that post-revision mHHS was not associated with any variable.
Conclusions
Revision THA performed through the DAA using primary stems grants satisfactory clinical and radiographic outcomes at a minimum follow-up of two years.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Advancements in bearing materials and implant design over the past two decades have helped overcome some of the challenges encountered during revision total hip arthroplasty (THA) due to severe osteolysis or bone loss. Revision THA is thus increasingly possible through minimally invasive approaches [1,2,3,4], without the need for long or distal-locking femoral stems [5,6,7], which could be preferable for surgeons that have been accustomed to performing primary THA through anterior approaches early in their specialty training.
The choice of stem in revision THA depends on multiple factors, including the presence of fractures, bone loss patterns, proximal femoral morphology, and whether the previous stem was cemented or uncemented [8,9,10]. If bone quality is adequate and there are no fractures, a primary stem can be considered, even when replacing a revision stem, which would prevent treatment escalation if additional revisions are required. Furthermore, the distal femoral canal can be difficult to prepare in cases with pedestal formation, distal narrowing, or well-fixed cement plugs; such challenges could be overcome by implanting a shorter stem than that removed.
In 2010, the senior author started performing revision THA using primary stems through the direct anterior approach (DAA) (his preferred technique for primary THA), except if the implanted stem was long and appeared to be well-fixed on radiographs, in which case the posterolateral approach was used to facilitate stem extraction. The DAA, although more challenging than the lateral or posterior approaches [3, 11], has been shown to reduce pain [12, 13], recovery time [12,13,14], and dislocation rates [15, 16], mainly because it is a minimally-invasive approach, which preserves the inter-nervous and inter-muscular planes [17]. The purpose of the study was to report clinical and radiographic outcomes of revision THA through the DAA using primary stems.
Materials and methods
The authors retrospectively assessed a consecutive series of 56 hips that underwent revision THA using a primary stem by the senior surgeon (FL) between 1 January 2010 and 30 June 2017. Hips were excluded from the study if they underwent revision THA through the posterior approach (n = 6), which was used if the stem implanted was long and appeared well fixed on radiographs. Therefore, the initial cohort comprised 47 patients (50 hips), aged 65 ± 10 years with a BMI of 25 ± 4 kg/m2, that underwent revision THA through the DAA using primary stems (Table 1). Reasons for revision THA were aseptic loosening in 30 hips (60%), periprosthetic joint infection (PJI) in 5 hips (10%), aseptic loosening secondary to periprosthetic fracture in 3 hips (6%), instability in 2 hips (4%), and acetabular cup protrusion with limb length discrepancy in 1 hip (2%). It is worth noting that 1 of the 5 cases operated for PJI had a 2-stage procedure. Twenty-three hips (46%) had isolated stem revision, while 27 hips (54%) had cup and stem revision (Table 2). All patients provided informed consent to use their data and images for research and publication purposes. The study was approved in advance by ‘GCS Ramsay Santé pour l’Enseignement et la Recherche’ (#COS-RGDS-2019-12-003-LAUDE-F).
Surgical technique
All patients were operated by the senior surgeon through the DAA with the patient placed in a supine position on an orthopaedic traction table. In cases where the primary stem to be implanted was shorter than the previous stem, residual cement was not removed in the distal area, thus reducing the risk of a false stem trajectory, femoral perforation or femoral fracture. For cemented stems, synthetic bone grafts (with or without autograft) were impacted using a trial femoral stem to improve the quality of the intra-medullary bone and limit the thickness of the cement mantle (Fig. 1). For uncemented stems, the femoral canal was reamed to a size that secured primary axial and rotational stability; in the presence of any small remaining gaps between the stem and the host bone, autograft was used to fill small bone defects prior to stem insertion (Figs. 2 and 3). From the initial cohort of 50 hips, 25 (50%) were revised with cemented stems, while 25 (50%) were revised with uncemented stems. It is worth noting that 1 of the 3 bilateral cases had an uncemented hip followed by a cemented hip. The choice between cemented and uncemented stems was not dependent on previous stem fixation, but only on bone quality; hips that required impaction grafting with either allo- and/or auto-graft were always cemented, while hips that did not require impaction grafting were always uncemented, even if autograft may have been used to fill small bone defects. Cases that required cemented stems were always implanted with the cemented Amistem, while cases that required uncemented stems were implanted with either the uncemented Amistem, Minimax, or Quadra, depending on femoral shape, bone quality and implant availability.
Process of a cemented stem being revised with a primary cemented stem. The failed cemented stem is first removed, then the proximal cement is removed, leaving the cement plug and distal cement mantle intact, then synthetic bone grafts (with or without autograft) are added to the femoral canal and then impacted using a trial stem, and finally, a primary cemented stem is implanted
Pre- and post-operative assessment
Before revision THA, all patients were clinically evaluated by the senior surgeon using the modified Harris Hip Score (mHHS). Pre-revision radiographic assessment was performed to evaluate the severity of femoral bone defects according to the Paprosky classification [18]. Pre-revision bone loss was grade I in 18 hips (36%), grade II in 13 hips (26%) and grade III in 19 hips (38%).
At a minimum follow-up of 2 years, an independent observer recorded the mHHS, as well as overall satisfaction with surgery (very satisfied, satisfied, disappointed, dissatisfied). Complications, reoperations, and re-revisions were noted. Post-revision radiographic assessment of standing antero-posterior (AP) pelvic and lateral hip radiographs, taken between 1 and 3 months post-revision and at last follow-up, was performed, which allowed comparison of the following: bone remodelling, cortical hypertrophy, subsidence, pedestal formation and osteolysis. Heterotopic ossification was determined according to the Brooker classification [19]. Stem subsidence was defined as a > 5 mm change in distance between the tip of the greater trochanter and the stem shoulder, when comparing first and final follow-up radiographs. Furthermore, for cemented stems, the following were also assessed: distal cement fractures and radiolucent lines (RLs) > 2 mm at the bone-cement and cement-stem interfaces. For uncemented stems, the following were also assessed: stress shielding, spot welds (endosteal bone bridges), and RLs > 2 mm at the bone-stem interface [20, 21]. Stem loosening was defined as subsidence > 5 mm, multiple bone cavitations or RLs > 2 mm along the entire femoral component [22, 23].
Statistical analyses
Descriptive statistics were used to summarise the data. Normality was assessed through Shapiro–Wilk tests. Univariable regression analyses were performed to determine associations of continuous outcomes (post-revision and net change in mHHS) with 14 independent variables. Subgroups were excluded from regression analyses if they contained under 5 patients. Multivariable regression analyses were not performed due to insufficient sample size [24]. P values < 0.05 were considered significant. Statistical analyses were performed using R, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Of the 50 hips (47 patients) in the initial cohort, 5 (10%; 5 patients) had minor intraoperative complications:
-
1 femoral calcar crack, fixed with orthoCord wire; this hip had Paprosky I before revision, the prior stem fixation was uncemented, and the current stem fixation was also uncemented.
-
3 femoral fractures, 2 of which were fixed with cerclage wire only, and 1 of which was fixed with a trochanteric plate, screws, and cerclage wire; two hips had Paprosky III before revision and one hip had Paprosky II, the prior stem fixation was cemented in the two hips with Paprosky III and uncemented in the hip with Paprosky II, and the current stem fixation was also cemented in the two hips with Paprosky III and uncemented in the hip with Paprosky II.
-
1 greater trochanter non-displaced fracture, left untreated; this hip had Paprosky III before revision, the prior stem fixation was cemented, and current stem fixation was uncemented.
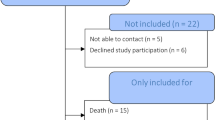
At a minimum follow-up of 2 years, 8 hips (16%, 7 patients) were excluded from the final cohort because 5 (10%; 4 patients) were lost to follow-up and 3 (6%; 3 patients) required stem re-revision (Fig. 4):
-
One for periprosthetic joint infection (2%; 1 patient), which required stem and cup re-revision 1 month after surgery; prior stem fixation was cemented, and current stem fixation was also cemented.
-
One for an intraoperative femoral calcar crack (2%; 1 patient), which was left untreated intraoperatively but progressed to stem loosening, and therefore required stem re-revision 13 months after surgery; prior stem fixation was uncemented, and current stem fixation was also uncemented.
-
One for subsidence > 5 mm resulting in aseptic loosening (2%; 1 patient), which required stem re-revision 67 months after surgery; prior stem fixation was cemented, and current stem fixation was also cemented.
Flowchart indicating number of hips and patients in the initial and final cohorts; *Of the 3 bilateral patients: 1 patient had both hips revised with cemented stems, 1 patient had both hips revised with uncemented stems (one hip was re-revised afterwards), and 1 patient had one hip revised with a cemented stem and the other hip with an uncemented stem
This left a final cohort of 42 hips (40 patients) available for clinical assessment; one of these hips was missing radiographic analysis, which left 41 hips (39 patients) for radiographic assessment. Postoperative complications that did not require stem re-revision were noted in 4 hips (8%; 4 patients):
-
1 hip required reoperation due to limb length discrepancy, and underwent femoral head exchange 1 month after surgery. This hip was included in the final cohort because the stem was left in place.
-
1 transitory neuropraxia of the lateral femoral cutaneous nerve
-
2 cases of early dislocation at 2 and 4 weeks, requiring closed reduction. There were no recurrent dislocations.
The final cohort of 42 hips (40 patients) was assessed at 4.3 ± 1.6 (range 2–8) years. Their mHHS improved from 51 ± 12 (range 32–81) to 89 ± 14 (range 47–100), with 32 patients (34 hips, 81%) being very satisfied and 6 patients (6 hips, 14%) being satisfied post-revision (Table 3). Univariable analysis revealed that post-revision mHHS was not associated with any variable; in contrast, the net improvement in mHHS decreased with pre-revision mHHS (Table 4).
In the final cohort, bone remodelling was observed in 8 hips (19%), cortical hypertrophy in 6 hips (14%), grade I heterotopic ossification in 7 hips (16%), and grade II in 1 hip (2%) (Table 5). There were no significant differences in the incidence of radiographic outcomes between cemented and uncemented stems. Of the 25 cemented stems, a distal cement fracture was observed in 1 hip. Of the 25 uncemented stems, spot welds were observed in 19 hips, and progressive stress shielding in 2 hips; but all stems were well osseointegrated. There were no cases of pedestal formation, osteolysis, RLs, or loosening (Figs. 5 and 6). No cases of subsidence were recorded between the radiographs performed at 1 to 3 months and at last follow-up.
A Pre-revision radiograph of the former cemented stem in a hip with Paprosky grade IIIA. B Radiograph taken 3 months after revision with a shorter primary cemented stem using impaction bone grafting. The previous stem was removed by performing a trochanterotomy and a longitudinal calcar osteotomy, the latter being fixed with 2 lag screws. C Radiograph taken 5 years after revision, showing consolidation of osteotomies and bone remodelling
Discussion
The most important finding of the present study is that revision THA performed through the DAA using primary stems grants satisfactory clinical and radiographic outcomes at a minimum follow-up of two years. At a follow-up of 4.3 ± 1.6 (range 2–8) years, the present series had a postoperative mHHS of 89 ± 14 (range 47–100), an intraoperative complication rate of 10%, a postoperative complication rate of 8%, and a re-revision rate of 6%. Furthermore, univariable analysis revealed no associations between postoperative mHHS and neither patient demographics nor surgical data.
The clinical outcomes of the present series are comparable to those reported in the literature following revision THA using primary stems performed by other approaches, which have reported mean post-revision mHSS ranging between 75 and 90 [6,7,8, 25,26,27], as well as intraoperative complication rates ranging between 0 and 20% [6,7,8, 26,27,28,29], postoperative complication rates ranging between 0 and 26% [6,7,8, 25,26,27,28,29,30], and re-revision rates ranging between 2 and 9% [6,7,8, 25,26,27,28,29,30]. In terms of radiographic outcomes, four studies have reported subsidence rates ranging between 0 and 36%, with varying subsidence thresholds [6,7,8, 28], while three studies have reported loosening rates ranging between 0 and 4% [7, 8, 28]. This is comparable to the present series, which reported no cases of subsidence or loosening, although it is possible that the subsidence rate was underdiagnosed as last follow-up radiographs were compared to radiographs taken at 1–3 months.
A recent systematic review [5] on nine clinical studies and 454 hips that underwent revision THA using primary uncemented stems concluded that primary stems represent a viable option in selected patients, with the 9 included studies reporting survival rates above 90% at last follow-up (> 2 years). The authors did not consider the effect of surgical approach (direct anterior, posterolateral…) on outcomes, but they did state that patient selection was important, and recommend the use of primary uncemented stems only in patients who had (i) pre-revision femoral Paprosky grades I or II, (ii) low number of previous surgeries, and (iii) a previous cementless stem. This is in contrast to the findings of the present study, as linear regression analyses revealed no association between clinical outcomes and pre-revision femoral Paprosky grade, number of previous surgeries, and previous stem fixation.
Surgeons do not always consider primary stems for revision THA, with some preferring to use long stems, especially those with distal fixation, as they may provide stability in femurs with poor proximal bone stock [31,32,33]. However, the use of long stems may increase the risk of intraoperative femoral fracture, distal femoral loading, proximal stress shielding and stem fracture [5, 34, 35], all of which could reduce bone stock in case of future revisions.
The DAA may be the preferred approach for primary THA by some surgeons, in terms of pain [12, 13], recovery time [12,13,14] and dislocation rates [15, 16]; though it has also been associated with greater risks of femoral failure, including stem loosening and perioperative fractures [36,37,38,39]. Only one previous study [4] has assessed the outcomes of revision THA through the DAA, although the type of stem used (primary, revision, or a combination of both) was not specified. The authors performed 349 stem revisions and reported a postoperative complication rate of 10%, which is slightly higher than that reported in the present study (8%); furthermore, no clinical outcomes or re-revision rates were reported.
The present retrospective study has a number of limitations. First, there was heterogeneity in follow-up, with a minimum of 2 years and a maximum of 8 years. Second, there was heterogeneity in the model of stem used (Amistem, Minimax, or Quadra), as well as in the fixation technique used (cemented or uncemented). Third, the first post-revision radiographs were taken between 1 and 3 months, meaning any subsidence or migration that occurred before this will not have been recorded. Fourth, the modified version of the Harris hip score (mHHS) was used, which does not include range of motion assessment; a correction factor was applied to be able to directly compare the mHHS to the original HHS. Fifth, the cohort size was small; nevertheless, this is the largest series up to date reporting on clinical and radiographic outcomes of a consecutive series of patients following revision THA operated by the same surgeon through the DAA using primary stems.
Conclusion
Revision THA performed through the DAA using primary stems grants satisfactory clinical and radiographic outcomes at a minimum follow-up of two years.
Data availability
Data can be requested from the corresponding author.
References
Baba T, Homma Y, Jinnai Y, Tanabe H, Banno S, Watari T et al (2020) Posterior versus direct anterior approach in revision hip arthroplasty using Kerboull-type plate. Sicot j 6:2
Thaler M, Dammerer D, Leitner H, Lindtner RA, Nogler M (2020) Mid-term follow-up of the direct anterior approach in acetabular revision hip arthroplasty using a reconstruction cage with impaction grafting. J Arthroplasty 35(5):1339–1343
Mast NH, Laude F (2011) Revision total hip arthroplasty performed through the Hueter interval. J Bone Joint Surg Am 93(Suppl 2):143–148
Kennon R, Keggi J, Zatorski LE, Keggi KJ (2004) Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg Am 86(2):91–97
Cavagnaro L, Formica M, Basso M, Zanirato A, Divano S, Felli L (2018) Femoral revision with primary cementless stems: a systematic review of the literature. Musculoskelet Surg 102(1):1–9
Kelly SJ, Incavo SJ, Beynnon B (2006) The use of a hydroxyapatite-coated primary stem in revision total hip arthroplasty. J Arthroplasty 21(1):64–71
Salemyr MF, Skoldenberg OG, Boden HG, Ahl TE, Adolphson PY (2008) Good results with an uncemented proximally HA-coated stem in hip revision surgery: 62 hips followed for 2–13 years. Acta Orthop 79(2):184–193
Gastaud O, Cambas PM, Tabutin J (2016) Femoral revision with a primary cementless stem. Orthop Traumatol Surg Res 102(2):149–153
Della Valle CJ, Paprosky WG (2004) The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res 420:55–62
Migaud H, Ala Eddine T, Demondion X, Jardin C, Laffargue P, Dujardin F et al (2000) Classification of bone loss: reproducibility of classifications and lesion groupings. Rev Chir Orthop Reparatrice Appar Mot 86(Suppl 1):38–42
Manrique J, Chen AF, Heller S, Hozack WJ (2014) Direct anterior approach for revision total hip arthroplasty. Ann Transl Med 2(10):100
Jia F, Guo B, Xu F, Hou Y, Tang X, Huang L (2019) A comparison of clinical, radiographic and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: a systematic review and meta-analysis. Hip Int 29(6):584–596
Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH et al (2018) A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 13(1):229
Rodriguez JA, Deshmukh AJ, Rathod PA, Greiz ML, Deshmane PP, Hepinstall MS et al (2014) Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res 472(2):455–463
Sariali E, Leonard P, Mamoudy P (2008) Dislocation after total hip arthroplasty using Hueter anterior approach. J Arthroplasty 23(2):266–272
Siguier T, Siguier M, Brumpt B (2004) Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res 426:164–173
Bremer AK, Kalberer F, Pfirrmann CW, Dora C (2011) Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br 93(7):886–889
Paprosky WG, Burnett RS (2002) Assessment and classification of bone stock deficiency in revision total hip arthroplasty. Am J Orthop 31(8):459–464
Brooker AF, Bowerman JW, Robinson RA Jr, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55(8):1629–1632
Engh CA, Massin P, Suthers KE (1990) Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res 257:107–128
Engh CA, Bobyn JD (1988) The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res 231:7–28
Dihlmann W, Dihlmann SW, Hering L (1991) Alloarthroplasty of the hip joint. Radiologic diagnosis of loosening and infection in cemented total endoprostheses. Radiologe 31(10):496–505
Melloh M, Eggli S, Busato A, Roder C (2011) Predictors of early stem loosening after total hip arthroplasty: a case-control study. J Orthop Surg (Hong Kong) 19(3):269–273
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68(6):627–636
Pinaroli A, Lavoie F, Cartillier JC, Neyret P, Selmi TA (2009) Conservative femoral stem revision: avoiding therapeutic escalation. J Arthroplasty 24(3):365–373
Tetreault MW, Shukla SK, Yi PH, Sporer SM, Della Valle CJ (2014) Are short fully coated stems adequate for “simple” femoral revisions? Clin Orthop Relat Res 472(2):577–583
Thorey F, Lerch M, Kiel H, von Lewinski G, Stukenborg-Colsman C, Windhagen H (2008) Revision total hip arthroplasty with an uncemented primary stem in 79 patients. Arch Orthop Trauma Surg 128(7):673–678
Howie DW, Wimhurst JA, McGee MA, Carbone TA, Badaruddin BS (2007) Revision total hip replacement using cemented collarless double-taper femoral components. J Bone Joint Surg Br 89(7):879–886
Petrie MJ, Harrison TP, Buckley SC, Gordon A, Kerry RM, Hamer AJ (2017) Stay short or go long? Can a standard cemented femoral prosthesis be used at second-stage total hip arthroplasty revision for infection following an extended trochanteric osteotomy? J Arthroplasty 32(7):2226–2230
Stigbrand H, Ullmark G (2017) A 3- to 18-year follow-up of revision total hip arthroplasty with impacted bone allografts and cemented lubinus SP II stem. Clinical, radiographic, and survivorship analysis with comparison to the literature. J Arthroplasty 32(9):2810–2814
Gabor JA, Padilla JA, Feng JE, Schnaser E, Lutes WB, Park KJ et al (2020) Short-term outcomes with the REDAPT monolithic, tapered, fluted, grit-blasted, forged titanium revision femoral stem. Bone Joint J 102(2):191–197
Ngu AWT, Rowan FE, Carli AV, Haddad FS (2019) Single 3 degrees tapered fluted femoral stems demonstrate low subsidence at mid-term follow-up in severe bony deficiency. Ann Transl Med 7(23):725
Herry Y, Viste A, Bothorel H, Desmarchelier R, Fessy MH (2019) Long-term survivorship of a monoblock long cementless stem in revision total hip arthroplasty. Int Orthop 43(10):2279–2284
Busch CA, Charles MN, Haydon CM, Bourne RB, Rorabeck CH, Macdonald SJ et al (2005) Fractures of distally-fixed femoral stems after revision arthroplasty. J Bone Joint Surg Br 87(10):1333–1336
MacDonald SJ, Rosenzweig S, Guerin JS, McCalden RW, Bohm ER, Bourne RB et al (2010) Proximally versus fully porous-coated femoral stems: a multicenter randomized trial. Clin Orthop Relat Res 468(2):424–432
Crawford DA, Rutledge-Jukes H, Berend KR, Morris MJ (2019) Does a triple-wedge, broach-only stem design reduce early postoperative fracture in anterior total hip arthroplasty? Surg Technol Int 35:386–390
Eto S, Hwang K, Huddleston JI, Amanatullah DF, Maloney WJ, Goodman SB (2017) The direct anterior approach is associated with early revision total hip arthroplasty. J Arthroplasty 32(3):1001–1005
Janssen L, Wijnands KAP, Janssen D, Janssen M, Morrenhof JW (2018) Do stem design and surgical approach influence early aseptic loosening in cementless THA? Clin Orthop Relat Res 476(6):1212–1220
Meneghini RM, Elston AS, Chen AF, Kheir MM, Fehring TK, Springer BD (2017) Direct anterior approach: risk factor for early femoral failure of cementless total hip arthroplasty: a multicenter study. J Bone Joint Surg Am 99(2):99–105
Funding
This work was supported by ‘GCS Ramsay Santé pour l’Enseignement et la Recherche’, which provided funding for manuscript preparation and statistical analyses. GCS Ramsay Santé pour l’Enseignement et la Recherche, COS-RGDS-2019-12-003-LAUDE-F, Frederic Laude.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MRVG, SRP, and MS have nothing to declare. FL declares royalties from Medacta.
Ethical approval
The present work was completed after being approved by an institutional review board (IRB: COS-RGDS-2019-12-003-LAUDE-F).
Informed consent
All patients provided informed consent for the use of their data and images for research and publishing purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Viamont-Guerra, MR., Ramos-Pascual, S., Saffarini, M. et al. Satisfactory clinical and radiographic outcomes following revision total hip arthroplasty by direct anterior approach using primary femoral stems at 2–8 years of follow-up. Arch Orthop Trauma Surg 143, 6393–6402 (2023). https://doi.org/10.1007/s00402-023-04838-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04838-6