Abstract
Background
Newer surgical approaches to THA, such as the direct anterior approach, may influence a patient’s time to recovery, but it is important to make sure that these approaches do not compromise reconstructive safety or accuracy.
Questions/purposes
We compared the direct anterior approach and conventional posterior approach in terms of (1) recovery of hip function after primary THA, (2) general health outcomes, (3) operative time and surgical complications, and (4) accuracy of component placement.
Methods
In this prospective, comparative, nonrandomized study of 120 patients (60 direct anterior THA, 60 posterior THAs), we assessed functional recovery using the VAS pain score, timed up and go (TUG) test, motor component of the Functional Independence Measure™ (M-FIM™), UCLA activity score, Harris hip score, and patient-maintained subjective milestone diary and general health outcome using SF-12 scores. Operative time, complications, and component placement were also compared.
Results
Functional recovery was faster in patients with the direct anterior approach on the basis of TUG and M-FIM™ up to 2 weeks; no differences were found in terms of the other metrics we used, and no differences were observed between groups beyond 6 weeks. General health outcomes, operative time, and complications were similar between groups. No clinically important differences were observed in terms of implant alignment.
Conclusions
We observed very modest functional advantages early in recovery after direct anterior THA compared to posterior-approach THA. Randomized trials are needed to validate these findings, and these findings may not generalize well to lower-volume practice settings or to surgeons earlier in the learning curve of direct anterior THA.
Level of Evidence
Level II, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, surgeons have attempted to increase the speed of postoperative recovery after primary THA with the use of so-called minimally invasive surgical (MIS) techniques. The posterior approach and anterior (Smith-Petersen) approach have been modified for MIS THA, referred to as the mini-posterior and direct anterior approach, respectively [9, 20, 22, 26]. Proposed advantages of MIS techniques include reduced blood loss, less pain, less postoperative limp, and faster rehabilitation [5, 7, 9, 22, 28]. These advantages are naturally appealing to both patients and surgeons. Dorr et al. [9], in a prospective, randomized, blinded study, reported that mini-posterior THA was associated with improved pain control and better early function and allowed earlier discharge to home when compared to conventional posterior-approach THA. It has also been reported that mini-posterior THA positively influenced postoperative patient satisfaction compared with conventional-incision-length posterior THA [10]. However, some literature has suggested that actual functional recovery may not be better when mini- and conventional posterior procedures are compared [6, 9, 23, 32]. Other studies have identified an increased frequency of complications with MIS THA compared to more traditional approaches [3, 31–33]. These complications include, but are not limited to, increased intraoperative blood loss, wound-healing problems, femoral or acetabular fracture, suboptimal implant alignment, dislocation, and early component loosening and subsidence. The complication rate seems to be higher in low-volume community settings [33] and during the learning curve of the surgeon with a new approach [31].
Some studies have compared recovery after THA performed through the direct anterior approach with other commonly used surgical approaches [1, 4, 21, 22, 30]. One study showed earlier normalization of Trendelenburg’s sign, single-leg stance, and walking velocity and fewer patients using walking aids at 3 weeks with THA using the direct anterior approach compared to mini-posterior approach [22]. However, no substantial gait benefit was found when spatiotemporal parameters were assessed in another study at 6 months’ followup [18]. We are unaware of any study comparing postoperative pain, early ambulation independence, return to activities of daily living, and general health outcomes between the direct anterior approach and the conventional posterior approach.
In this prospective, nonrandomized study, we compared the direct anterior approach and conventional posterior approach to THA in terms of (1) recovery of hip function after primary THA, (2) general health outcomes, (3) operative time and surgical complications, and (4) accuracy of component placement.
Patients and Methods
From January through December 2010, all patients undergoing primary THA who qualified according to prespecified inclusion and exclusion criteria were invited to enroll in this single-institution prospective, comparative trial. Surgeon 1 (JAR) exclusively utilized the direct anterior approach for primary THA during the study period, except on three occasions; two involved a hip with presence of hardware that was removed at the time of THA and the third involved a large gluteus medius tear that was repaired during the procedure. A posterior approach was used for these three THAs. Surgeons 2 and 3 (ASR, MSH) performed all surgeries via the posterior approach, making this a prospective comparative study of three parallel consecutive series. The inclusion criteria were age of 25 to 75 years, diagnosis of unilateral osteoarthrosis of the hip without a defined cause, and willingness to comply with the study protocol. Exclusion criteria included diagnosis other than unilateral hip osteoarthrosis without a defined cause, patients undergoing bilateral THAs, THA for femoral neck fracture, previous open surgery on/around the hip with or without presence of hardware, infection, neuromuscular disorders, inflammatory arthropathy, and other musculoskeletal disorders with potential to impede postoperative rehabilitation and weightbearing. The study was approved by the institutional review board of our hospital and written informed consent was obtained from all patients.
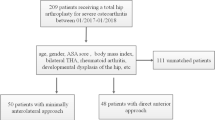
During the study period, a total of 458 primary THAs (458 patients) were performed by the three participating surgeons. Of these, 205 patients declined to participate, and 121 patients failed to qualify based on the prespecified inclusion and exclusion criteria (Fig. 1), leaving 132 patients who consented to participate in the study. Of those, seven patients were subsequently removed (three in the direct anterior group, four in the posterior group) because of lack of timely followup visits and five voluntarily withdrew (four in the direct anterior group, one in the posterior group), leaving 120 patients (60 for each approach) for final data analysis. The direct anterior group consisted of 60 patients (28 men, 32 women) with a mean ± SD age of 60 ± 10 years and a mean BMI of 27 ± 4. The posterior group comprised 60 patients (26 men, 34 women) with a mean age of 59 ± 6 years and a mean BMI of 28 ± 4. Surgeon 2 (ASR) contributed 39 THAs and Surgeon 3 (MSH) contributed 21 THAs in the posterior group. There were no significant differences in patient demographics and preoperative scores between the two groups (Table 1).
All participating surgeons were fellowship trained and were primarily trained for posterior THA. The surgeon who performed direct anterior THAs obtained cadaver training and numerous operating room visits observing and assisting other surgeons who performed this approach. To minimize the influence of a learning curve, this study was initiated after performance of 150 THAs via the direct anterior approach by Surgeon 1. Direct anterior THAs were performed according to the technique described by Lovell [17], with anterior capsulotomy and closure, the use of a standard operating table (Fig. 2) with a table mounted femoral elevator (Omni-Tract Surgical, St Paul, MN, USA), selective soft tissue releases (posterosuperior hip capsule over the saddle of the femoral neck, conjoined and piriformis tendons) based on mobility of the femur, and the use of fluoroscopy in every case. Stability was assessed with provocative testing in extension and external rotation, and leg length and socket position were adjusted to achieve stability. Leg length was determined by direct comparison between legs and using the C-arm. Posterior THAs were performed as previously reported [28] and involved an incision of 14 to 16 cm in length with release of gluteus maximus tendon, quadratus femoris, obturator externus tendon, conjoined tendon, piriformis tendon, and reflected head of rectus femoris. Repair of capsular and musculotendinous structures (piriformis, conjoined tendon, quadratus and gluteus maximus tendon) was performed through trochanteric drill holes and/or direct repair. Compared to the conventional posterior approach, the mini-posterior approach consists of an incision length of approximately 10 cm, less splitting (6 cm) of the gluteus maximus muscle, no splitting of the tensor fascia latae, preservation of the gluteus maximus tendon and quadratus femoris, reflected head of the rectus femoris, and smaller (3–4 cm) posterior capsulotomy [9]. Stability was assessed with provocative testing in flexion, adduction, and internal rotation, and leg length and socket position were adjusted to achieve stability. Leg length was determined using a Steinman pin in the infracotyloid groove as previously described [29]. All hips received similar designs of uncemented acetabular and femoral components. Femoral components were of a tapered-wedge, proximally porous-coated design (direct anterior group: Anthology™; Smith & Nephew, Inc, Memphis, TN, USA; posterior group: Accolade® TMZF; Stryker Orthopaedics, Mahwah, NJ, USA). Acetabular components (direct anterior group: R3™; Smith & Nephew, Inc; posterior group: Trident®; Stryker Orthopaedics) were also porous titanium implants. All liners were of highly crosslinked polyethylene. Ceramic surface femoral heads were used in all hips and were either 32 or 36 mm, depending on cup size.
A photograph demonstrates operating room setup for the direct anterior approach performed on a standard operating table with a table mounted femoral elevator. The foot end of the table is dropped during femoral preparation to achieve the desired hip extension and the contralateral lower extremity is placed on a Mayo stand to allow adduction and external rotation for femoral exposure. A C-arm can be easily used as the pelvis and hips are placed on the radiolucent part of the operating table.
All patients were managed with the same multimodal anesthesia and analgesia protocol. Preoperatively, patients received 20 mg sustained-release oxycodone (Oxycontin®; Perdue Pharma, Stamford, CT, USA) and 200 mg celecoxib (Celebrex®; Pfizer, New York, NY, USA). Spinal anesthesia with supplemental intravenous sedation was used, as well as a periarticular cocktail injection [19]. The postoperative analgesia protocol included oral acetaminophen, celecoxib, and sustained-release and short-acting oxycodone. This was supplemented with intravenous morphine or ketorolac on an as-needed basis. Patients were discharged on a combination of sustained-release and short-acting oxycodone with acetaminophen. All patients received warfarin for postoperative thromboprophylaxis. Patients were first seen by a physical therapist on the morning after surgery and received two sessions of physical therapy daily until discharge from the hospital. Patients were encouraged to move from bed to chair on the first postoperative day with weightbearing as tolerated. A walker frame with wheels or a pair of Lofstrand crutches was provided depending on patient preference. All patients were assessed according to similar objective discharge criteria by the physical therapy department. Patients were discharged home if they could transfer in and out of bed and chair independently, walk a minimum distance of 150 feet (46 m), and ascend-descend a flight of four stairs. Patients were discharged to a skilled nursing facility if they failed to meet the criteria listed above. No hip precautions were imposed on patients receiving the anterior approach, whereas patients who received the posterior approach were advised to use an abduction pillow and high chair and to avoid a combination of flexion of more than 90° with adduction and internal rotation for 6 weeks. On discharge, patients were advised to resume activities as they could tolerate, with hip comfort being their guide. Patients were also encouraged to progress to a cane as tolerated. Apart from the difference in hip precautions, standardized rehabilitation instructions were issued to physical therapists taking care of patients at home or at outpatient physical therapy facilities. Driving was allowed once narcotic medications had been discontinued and all employed patients were encouraged to return to work as soon as they felt comfortable.
Care was taken not to discuss the study hypothesis with patients. Pre- and postoperative data were collected by administering self-reported questionnaires to patients during their office visits, thus comprising a subjective assessment of when specific milestones of recovery were achieved by the patient. All patients were queried for the presence of groin pain at followup visits. To minimize bias, physical examination and special tests required for the study were performed and results recorded by either an arthroplasty fellow or a physician assistant and not by the operating surgeon. Intraoperative data were recorded by a research fellow and postoperative recovery during hospital stay was evaluated by an experienced physical therapist. Each patient maintained a milestone diary to self-record attainment of activities of daily living, which was returned to the clinical research department after completion. All patients received weekly telephone calls from the clinical research department to monitor progress and ensure the milestone diaries remained current.
Recovery during hospital stay was recorded on a twice-daily basis. This was done using the partial motor component of the Functional Independence Measure™ (M-FIM™), which included independence of bed/chair transfers and walking and stair functions [12]. The FIM™ has been widely used to assess basic quality of daily living activities in persons with a disability with excellent reliability [25]. Maximum achievable M-FIM™ score before discharge from hospital was 19 points (of 21) and corresponded with ability to walk 150 feet with an assistive device, go up and down one flight of stairs (12 stairs), sit and get up to a standing position from a chair, and safely and independently transfer from bed to chair.
The timed up and go (TUG) test [14, 27] was performed on Postoperative Day 3 or at the time of discharge, if earlier. This test has been validated and found to correlate significantly with gait velocity, stride length, step frequency, functional capacity (Barthel index), and the FIM™ and M-FIM™ [14]. Pain was assessed using the 10-point VAS at 48 hours postoperatively and the mean VAS scores of the two groups were compared. Length of hospital stay, narcotic consumption, discharge disposition, and postoperative complications were recorded.
Harris hip score (HHS) [13], UCLA activity score [2], M-FIM™, and TUG were recorded preoperatively and at 2, 6, and 12 weeks postoperatively. HHS and UCLA were recorded additionally during the 1-year followup. The milestone diary was derived from a previously published study [26]. This was handed over to patients postoperatively and was returned to the clinical research department on completion.
General health outcomes were assessed with SF-12 scores [15, 24]. This was completed preoperatively and at 6 weeks, 12 weeks, and 1 year.
Operative time (time from incision to end of closure) was recorded, as were intraoperative and early postoperative complications and reoperation frequency.
Postoperative radiographs were obtained in the recovery room and then at 6 weeks and 1 year. Radiographic analysis was performed by a blinded observer on 6-week and 1-year postoperative, standardized, AP pelvis radiographs using a Picture Archiving and Communications System Software (Synapse®; Fujifilm Medical System, Stamford, CT, USA). Anteversion and inclination of the acetabular cup were assessed as previously described by Liaw et al. [16], femoral stem alignment was determined as per Ellison et al. [11], hip offset was measured as described by Dastane et al. [8], and limb length difference was assessed as described by Ranawat et al. [29]. Osseointegration of components was assessed based on absence of radiolucent lines and implant migration or subsidence.
Power analysis was carried out before initiation of the study to ensure an adequate sample size. This was based on a previous study utilizing similar milestones for comparison of different approaches for THA [26]. The primary outcome of effect size was defined as the difference in time to discontinue all walking aids and time to walk 0.5 miles (0.8 km). A sample size of at least 26 patients in each group would provide 80% power to detect a difference of 4.0 days in the time to discontinue all walking aids and a difference of 6.6 days in the time to walk 0.5 miles. For statistical analysis, a p value of 0.05 or less was considered significant. Clinical data collected at each visit and radiographic data were compared using independent t-tests (for continuous variables with normal distribution), Mann-Whitney U tests (for nonparametric outcomes), and chi-square analysis (for categorical data). Levene’s test for equality of variances was used to compare any differences in variances in acetabular cup positioning between groups. Variances were defined as the square of the SD around the mean for that sample. The statistical software used was SPSS® Version 16 (SPSS Inc, Chicago, IL, USA).
Results
Patients in the direct anterior group achieved some, but not all, functional milestones earlier than the patients in the posterior group; most of these differences had disappeared by 2 weeks, and all of them had disappeared by 6 weeks after surgery. Patients in the direct anterior group achieved their peak M-FIM™ score significantly earlier than patients in the posterior group (p = 0.001) (Table 2). By the second postoperative day, 50 patients in the direct anterior group versus 28 in the posterior group were able to walk 150 feet (p = 0.001), 49 versus 25 were able to go up and down a flight of stairs (p = 0.001), and 54 versus 35 were able to independently perform bed/chair transfers (p = 0.03). Additionally, walking velocity was greater with the direct anterior approach based on the TUG test (p = 0.001) as measured on the third postoperative day or before discharge, if earlier. There was no difference in the mean VAS scores (direct anterior 3.3 versus posterior 3.5; p = 0.52) and average narcotic consumption in morphine equivalents (direct anterior 43 versus posterior 49; p = 0.21). The length of hospital stay was not different between groups (direct anterior 3.05 days versus posterior 3.2 days; p = 0.1). Similarly, there was no difference in the number of patients discharged to a skilled nursing facility from either group (direct anterior five patients versus posterior six patients). At 2 weeks, the TUG was still significantly quicker in the direct anterior group (p = 0.008); however, no differences were observed between groups for M-FIM™ (p = 0.23), UCLA (p = 0.07), and HHS (p = 0.09) scores (Table 3). As assessed from the milestone diary, the average time at which patients reported achieving milestones of recovery and resumption of activities of daily living was not different between groups (Table 4). The need for assistive devices and time taken from surgery to be able to walk 0.5 miles likewise was not different between groups. We found no significant differences in TUG (p = 0.32), M-FIM™ (p = 0.40), HHS (0.13), and UCLA (p = 0.39) scores at 6 weeks (Table 3). Similarly, at 12 weeks and 1 year postoperatively, no differences were observed between groups (Table 5).
There were no differences at any time point, before or after surgery, in terms of the physical and mental components of the SF-12 between groups (Table 6).
There were no differences between groups in terms of surgical time or complications. Mean surgical time was similar (direct anterior 90 ± 15 minutes versus posterior 85 ± 14 minutes; p = 0.09). Complications in the direct anterior group included one undisplaced greater trochanter fracture, four patients reporting groin pain, and one patient with Grade 2 heterotopic ossification. Forty percent of patients reported numbness somewhat distal and lateral to their anterior incision; no patient had transient paresthesia or true meralgia paraesthetica. In the posterior group, one patient sustained a posterior dislocation (underwent cup revision), two patients reported groin pain, and one patient had Grade 2 heterotopic ossification.
There was a small but statistically significant difference in mean cup anteversion; this difference probably was not clinically significant, and there were no other differences in terms of component alignment between groups (Table 7). There were no cases of failed osseointegration or component loosening at 1-year followup.
Discussion
THA is a common and highly successful orthopaedic procedure and has been performed through a variety of surgical approaches. Surgical approach may influence postoperative recovery after THA; however, there is no consensus as to which approach offers faster recovery. At our institution, the posterior approach has been traditionally used for THA and has been safe, efficacious, and reproducible. The direct anterior approach has been recently championed to be an intermuscular and internervous approach with the potential to offer rapid postoperative recovery without compromising reconstructive safety and accuracy [17, 20]. However, to our knowledge, no study has specifically compared postoperative pain, early ambulation independence, return to activities of daily living, and general health outcomes between the direct anterior approach and conventional posterior approach. In this nonrandomized study, we observed some short-lived functional advantages favoring the direct anterior approach, but none that lasted more than 6 weeks. General health outcomes, operative time, complications, and component alignment were not different between the two treatment groups.
Our study has limitations. There were differences in postoperative instructions pertaining to dislocation precautions. This may have created a psychologic bias in patients’ level of comfort with moving the extremity and thus on early recovery favoring the direct anterior approach. Also, the study was not randomized, and many of the patients in the direct anterior group had sought out this approach, so perhaps were more motivated. The lack of randomization means that selection biases of other sorts might have applied here; selection bias usually favors novel approaches in studies of this design. We tried to offset this by defining the groups by the surgeons, each of whom did his preferred technique in all patients during the period in question. Also, the therapist logging early recovery data was not blinded to the approach, and as such the potential for bias exists. Another limitation of this study was the lack of objective biomechanical data on gait and muscle strength. Lastly, the relatively short followup time of 1 year was a limitation. Although this was primarily a study of early recovery, further followup may elucidate other differences between cohorts.
Our study suggested that, compared to the conventional posterior approach to THA, the direct anterior approach achieved objective measures of postoperative recovery at an earlier time point, based on the TUG and M-FIM™. However, measured differences began to disappear by 2 weeks and no differences could be detected by 6 weeks. Sometime between 2 and 6 weeks, the two groups became comparable and remained similar at 12 weeks and 1 year. Patients’ self-reported subjective measures of activities of daily living and functional recovery were comparable at all times. Better TUG at 2 weeks with the direct anterior approach in our study corroborated with the finding of better gait velocity at 3 weeks in the study of Nakata et al. [22]. However, contrary to their findings, we found no difference in the time taken to give up walking aids between groups. Bergin et al. [6] prospectively compared the direct anterior and posterior approaches seeking to identify differences in serum markers of inflammation and muscle damage. They noted significant differences in serum creatine kinase and tumor necrosis factor α levels, with lower levels with the direct anterior approach, but no differences based on other inflammatory markers. Additionally, no significant differences have been found in spatiotemporal gait parameters between the two approaches [18].
General health outcome measures, operative time, and surgical complications were similar between groups in our study; to our knowledge, these end points have not been specifically evaluated by other studies comparing the direct anterior and posterior approaches. However, a review of recent literature suggested a remarkably higher complication rate associated with the direct anterior approach, especially in lower-volume settings and during the learning curve of the surgeon [31, 33]. It appears that pretraining is critical when embracing a new approach such as the direct anterior approach to minimize complications. The surgeon who performed the anterior procedures in this study had been adequately pretrained with a learning curve of more than 150 cases. Lower-volume and less-experienced surgeons may not achieve comparable clinical results.
Our radiographic analysis revealed smaller variances for acetabular component placement in the direct anterior group, likely due to intraoperative use of the C-arm. This has been illustrated by a scatterplot (Fig. 3). The cup anteversion was intentionally kept less in the direct anterior group due to concerns about anterior instability. As expected, there was a significant difference in mean cup anteversion between groups in our study (direct anterior 13° versus posterior 16°). The lower anteversion may have resulted in a slightly higher number of patients with the direct anterior approach having groin pain related to psoas impingement. There was no difference between groups with regard to mean cup inclination (direct anterior 40° versus posterior 40°).
We found anterior and posterior procedures to provide comparable results in terms of pain and function. Some objective measures of recovery were reached at an earlier time point with the direct anterior approach, but most metrics were comparable at all time points, and even the observed differences were short-lived. The groups became comparable on all measured parameters somewhere between the 2- and 6-week followup. Randomized trials are called for if others agree that these short-term differences are worth pursuing. Future research investigating objective recovery of hip muscle strength and documentation of muscle injury by MRI might also be instructive.
References
Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. 2011;12:123–129.
Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241.
Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique. J Bone Joint Surg Am. 2005;87:2432–2438.
Berend KR, Lombardi AV Jr, Seng BE, Adams JB. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am. 2009;91(suppl 6):107–120.
Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247.
Bergin PF, Doppelt JD, Kephart CJ, Benke MT, Graeter JH, Holmes AS, Haleem-Smith H, Tuan RS, Unger AS. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am. 2011;93:1392–1398.
Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144.
Dastane M, Dorr LD, Tarwala R, Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res. 2011;469:429–436.
Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni L. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty: a prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160.
Dorr LD, Thomas D, Long WT, Polatin PB, Sirianni LE. Psychologic reasons for patients preferring minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2007;458:94–100.
Ellison B, Cheney NA, Berend KR, Lombardi AV Jr, Mallory TH. Minimal stress shielding with a Mallory-Head titanium femoral stem with proximal porous coating in total hip arthroplasty. J Orthop Surg Res. 2009;4:42.
Guide to the Uniform Data Set for Medical Rehabilitation (Adult FIM), Version 4.0. Buffalo, NY: State University of New York at Buffalo; 1993.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end result study using a new method of result evaluation. J Bone Joint Surg Am. 1969:51:737–755.
Hershkovitz K, Brill S. Get up and go—home. Aging Clin Exp Res. 2006;18:301–306.
Kosinski M. Scoring the SF-12 physical and mental summary measures. Medical Outcomes Trust Bulletin. 1997;5:3–4.
Liaw CK, Yang RS, Hou SM, Wu TY, Fuh CS. Measurement of acetabular cup anteversion on simulated radiographs. J Arthroplasty. 2009;24:468–474.
Lovell TP. Single-incision direct anterior approach for total hip arthroplasty using a standard operating table. J Arthroplasty. 2008;23:64–68.
Maffiuletti NA, Impellizzeri FM, Widler K, Bizzini M, Kain MS, Munzinger U, Leunig M. Spatiotemporal parameters of gait after total hip replacement: anterior versus posterior approach. Orthop Clin North Am. 2009;40:407–415.
Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467:1418–1423.
Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124.
Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, Leardini A. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon). 2009;24:812–818.
Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty. 2009;24:698–704.
Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D, A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710.
Ostendorf M, van Stel HF, Buskens E, Schrijvers AJ, Marting LN, Verbout AJ, Dhert WJ. Patient-reported outcome in total hip replacement: a comparison of five instruments of health status. J Bone Joint Surg Br. 2004;86:801–808.
Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232.
Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:1000–1006.
Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148.
Ranawat CS, Ranawat AS, Rasquinha VJ. Mastering the art of cemented femoral stem fixation. J Arthroplasty. 2004;19:85–91.
Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16:715–720.
Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty. 2010;25:671–679.
Spaans AJ, van den Hout JA, Bolder SB. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012;83:342–346.
Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86:1353–1358.
Woolson ST, Pouliot MA, Huddleston JI. Primary total hip arthroplasty using an anterior approach and a fracture table: short-term results from a community hospital. J Arthroplasty. 2009;24:999–1005.
Acknowledgments
We thank Kelly Stets MD, Raman Thakur MD, Anitha Jacob PA-C, Julie Pate PA-C, Leah Verebes PA, Neil Moskowitz PT, Daniel Gross DPT, PT, and Kshitij Agrawal MD for their help with this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Rodriguez, J.A., Deshmukh, A.J., Rathod, P.A. et al. Does the Direct Anterior Approach in THA Offer Faster Rehabilitation and Comparable Safety to the Posterior Approach?. Clin Orthop Relat Res 472, 455–463 (2014). https://doi.org/10.1007/s11999-013-3231-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3231-0