Abstract
Introduction
The incidence of periprosthetic femur fractures is increasing. Multiple treatment methods exist to treat fractures surrounding stable hip arthroplasty implants including locking plate fixation, cable fixation, allograft augmentation, and revision arthroplasty. No consensus regarding optimal treatment has been reached, and significant complications remain. Recently, biomechanical studies have demonstrated the benefits of orthogonal dual-plate fixation, but little clinical data exist. The purpose of the current study was to investigate the clinical and radiographic outcomes of dual-plated periprosthetic femur fractures around stable hip stems.
Materials and methods
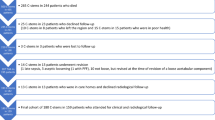
Patients with periprosthetic femur fractures following hip arthroplasty with a stable femoral stem treated with dual-plate fixation were identified through chart review at a single institution. Fracture classification, fixation characteristics, radiographic outcomes, clinical outcomes and complications including re-operation were recorded.
Results
Over a 12-year period, 31 patients (mean age 77 years at surgery, range 48–94) underwent dual plating by three traumatologists for implant-stable periprosthetic femur fractures surrounding a hip arthroplasty stem. There were 27 Vancouver B1-type and 9 inter-prosthetic fractures. Average follow-up was 2 years. Of the 26 patients with minimum 6-month follow-up, 24 (92%) united after index surgery (mean time to union 6.0 months, range 1.5–14.0). Mean time to full weight-bearing post-operatively was 2.6 months (range 1.5–4.0 months). Two patients required secondary surgery to address nonunion.
Conclusions
Dual-plating achieved high union rates with an acceptable complication profile for the treatment of periprosthetic femur fractures surrounding a stable hip arthroplasty stem. Our preferred fixation construct involves a lateral plate spanning the entire femur secured with non-locking bicortical screws supplemented with an anteriorly based reconstruction plate. Additional prospective research is required to confirm the results of this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of periprosthetic femur fractures continues to rise [1]. This can be attributed to an increase in primary and revision arthroplasty procedures performed, the increase in age and frailty of the population undergoing these procedures, and the increased preference towards uncemented fixation of femoral components. Proximal fractures involving stable implants are often treated with open reduction and internal fixation (ORIF), while considering the medical and functional status of the patient. Fixation can be particularly challenging for these injuries given the decrease in bone available for fixation surrounding the femoral implant, the high level of stress in the femur at the tip of the prosthesis, and generalized osteopenia. Several strategies have been developed to mitigate these issues including locking plate fixation, cortical strut allografts, cerclage wires/cables, and a combination of these methods. As comparative studies are currently lacking, there is no current consensus for optimal treatment [2, 3]. There remains potential for improvement in managing these injuries given the high rates of re-operation reported following ORIF of periprosthetic femur fractures in the literature to date (12–26%) [4, 5].
Dual-plate fixation, in which an anteriorly based plate supplements laterally based fixation, has demonstrated biochemical merit for proximal periprosthetic femur fractures (PPFFs) [6,7,8]. Little clinical data have been reported using this technique, however. The purpose of this study was to determine clinical and radiographic outcomes of patients with PPFFs about a stable hip stem treated with dual-plate fixation. The primary outcome measured was fracture union. Secondary outcomes included complications and time to weight-bearing.
Materials and methods
Inclusion criteria
Following institutional review board approval, we performed a retrospective review of three surgeons’ surgical logs of all implant-stable acute PPFFs treated with dual-plate fixation from 2008 to 2019. Surgical procedures for nonunions and fixation failure were excluded. Fractures were classified by two observers (–, –) according to the Vancouver system [9] as either B1 (fracture around a well-fixed stem) or C (fracture occurring well below the tip of the stem). Interprosthetic femur fractures were included if classified according to the Unified Classification System [10] as UCS D IV.3 (between hip and knee arthroplasties, close to the hip) and if the choice of fixation construct applied was believed to be independent of the total knee arthroplasty (TKA) implant. Femoral stem type (primary or revision) and mode of fixation (cementless or cemented) were also recorded. Patients lacking initial injury radiographs, operative reports, sufficient clinical and radiographic follow-up were excluded.
Fracture management
Operative management was performed at a single institution by one of the three trauma fellowship-trained orthopedic surgeons. Patients were positioned supine and a standard lateral sub-vastus approach was performed. Anatomic reduction was achieved with a combination of manual traction, leg position, and application of clamps and/or plates. After anatomic reduction, the fracture was stabilized with a lateral and anterior plate. Plate selection and overall fixation construct were at the surgeon’s discretion in each case. Primary (lateral) plates used included the Synthes 4.5 mm Curved Locking Compression Plate (LCP), Synthes 4.5 mm LCP Proximal Femoral Hook Plate and Synthes 4.5 mm LCP (Distal Femur) Condylar Plate (including conventional and variable angle versions). Lateral plate length was selected to ensure that the entire femur was spanned. Secondary (anterior, posterolateral or medial) plates used included Synthes 3.5 mm reconstruction plate, Synthes 3.5 mm LCP, Synthes 3.5 mm T-Plate, and Synthes 4.5 mm LCP. Post-operative rehabilitation regime was at each surgeon’s discretion and modified on a case-by-case basis, but typically involved toe-touch weight-bearing with 20lbs for 6 weeks followed by progressive weight-bearing to as tolerated over the course of a few weeks guided by a physical therapist.
Outcomes
Outcomes were assessed by chart and imaging review. Union was the primary outcome and defined as cortical bridging of the fracture on at least 3 of the 4 cortices on orthogonal radiographs and correlated with pain-free weight-bearing. Nonunion was defined as lack of progressive fracture healing over a three-month period extending beyond six months from the date of surgery. Malunion was defined as > 5º malalignment on either anteroposterior or lateral radiographs. Additionally, time to weight-bearing as tolerated (regardless of ambulatory aid), use and type of ambulatory aid were documented. Complications including hardware failure, stem subsidence, infection, and additional surgical procedures were assessed. Elements of fixation construct were recorded based on several factors: plate type and length, plate orientation, number and type of screws adjacent to implant, number of cerclage wires/cables, number of screws into cement mantle (if present), bone graft presence and type.
Results
Demographics and fracture characteristics (Table 1)
We identified 31 periprosthetic femur fractures in 31 patients (mean age 77.6 ± 11.7 years, range 48–94 years; 19 females, 12 males) treated with dual-plate fixation during the period of 2008–2019. The mean follow-up after PPFF surgery was 2 years (range 2 months–6 years).There were 13 left-sided and 18 right-sided femur fractures. Two patients had hemiarthroplasty components and 29 patients had total hip arthroplasty (THA) components in situ, 4 of which were uncemented diaphyseal-engaging revision femoral stems.
There were 26 Vancouver B1-type fractures and 5 Vancouver C-type fracture. There were 20 simple spiral fractures (4 of which extended to the distal femoral metaphysis), 2 fractures with a butterfly fragment, 4 significantly comminuted fractures, and 5 short oblique/transverse fractures. Of the 31 total fractures, 9 were classified as inter-prosthetic fractures (UCS D IV.3). Five of the inter-prosthetic fractures were classified as Vancouver B1 fractures with standard femoral stems proximally and standard TKA distally. One patient had a comminuted distal femur periprosthetic fracture below the anterior flange of a TKA (Su Type-3) in the presence of a long-femoral revision THA stem. The remaining 3 patients had direct fracture involvement of the femoral implants of both the THA and TKA.
Fixation characteristics (Table 2)
Lateral fixation with the Synthes 4.5 mm Curved LCP was performed in 16 cases (Fig. 1), the Synthes 4.5 mm LCP Proximal Femoral Hook Plate was used in 4 cases, and the Synthes 4.5 mm LCP Distal Femur Condylar Plate was used in 11 cases. All lateral plates spanned the length of the femur aside from three cases in which the distal femoral plates overlapped the femoral component but did not extend proximal to the subtrochanteric region. Secondary plates were placed anteriorly in 26 patients; a 3.5 mm reconstruction plate was used in 23 cases, a 3.5 mm LCP in 2 cases, and a 4.5 mm LCP in one case. A posterolateral 3.5 mm reconstruction plate was used as a secondary plate in 3 cases. A medial plate was used on the distal femur in 2 cases, one with a 3.5 mm T-plate and another with 3.5 mm reconstruction plate.
Anteroposterior (a, b) and lateral (c, d) radiographs of an 85-year-old male with a comminuted Vancouver Type-B1 fracture between a cemented hip hemiarthroplasty and total knee arthroplasty. Follow-up radiographs (e, f) demonstrate fracture union two years post-operatively from dual-plate fixation. The lateral 4.5 mm Distal Femur Condylar Plate was secured with non-locking bicortical screws proximally adjacent to the femoral implant, with locking screws placed distally. The anterior 3.5 mm reconstruction plate was secured with non-locking bicortical screws
The plates were secured with a mean of 6 bicortical screws (range 2–9) around the THA femoral component. Supplemental fixation of the bicortical screw and plate construct occurred in four cases with circumferential cerclage wires and two cases with unicortical locking screws. Fifteen of the 16 cemented stems had screw fixation into the cement mantle, with a mean of 2 bicortical screws (range 1–3) placed.
Healing and complications (Table 3)
Of the 26 patients with minimum 6-month follow-up, 24 (92%) went onto union after the index procedure. The mean time to union following fracture fixation was 6.0 months (range 1.5–14.0 months). Time to weight-bearing was recorded in 28 cases, with a mean of 2.6 months (range 1.5–4.0 months). On final follow-up, a total of 15 patients ambulated independently, 10 patients with a walker, 2 with a cane, one with a crutch, and one patient with baseline Parkinson’s disease was wheelchair bound.
Two patients required additional procedures to achieve union. Revision ORIF with repeat orthogonal plating was performed in one case due to varus collapse and impending non-union, achieving union 10 months after the initial injury. Another case of fixation failure underwent a long-femoral stem revision with allograft augmentation. One patient required removal of the most distal screw of the lateral 4.5 mm LCP due to medial-sided pain and was asymptomatic thereafter. One patient had a superficial surgical site infection that resolved with a course of oral antibiotics. There were no cases of deep infection.
At final radiographic follow-up, there were no cases of aseptic loosening or subsidence of the femoral or acetabular components. There were four cases of malunion with a mean coronal malalignment of 11.7° (range 6.0–13.6°), none of which required additional procedures.
Discussion
The management of periprosthetic femur fractures continue to pose a challenge for the orthopedic surgeon. Fracture union and return to baseline ambulatory status remain important treatment goals in light of the significant morbidity and mortality associated with these injuries. Unfortunately, re-operation rates remain quite high in this elderly patient population with many comorbidities [5, 11]. In the current study of 31 periprosthetic femur fractures treated with dual-plate fixation at a single center, we achieved high union rates (92% after index procedure), early weight-bearing (2.6 months) and low complications with a mean follow-up of approximately 2 years.
Modern treatment strategies for PPFFs predominantly involve isolated locked lateral femoral plates or the use of cable plating with and without allograft. However, there is no consensus for optimal management [2], and a lack of comparative trials investigating optimal fixation method makes the literature difficult to interpret. Biomechanical studies have demonstrated that cables are stiffer than cerclage wires, locking plates are stiffer than conventional dynamic plates secured with cables under torsion and axial load, and the addition of a cortical strut allograft to a plate construct is stiffer than a locking plate alone [12,13,14]. A Locking Attachment Plate (LAP; Synthes, Paoli, PA), which allows bicortical screw fixation anterior or posterior to the femoral implant, has shown merit as well [15]. Advocates for allograft augmentation argue that the orthogonal configuration (lateral plate and anterior graft) provides enhanced biomechanical stability and can add to femoral bone stock [13]. Although clinical outcomes have been quite favorable with modern allograft augmentation given the high union rates [16,17,18], several concerns exist. The placement of an anteriorly based allograft secured with circumferential wires may theoretically hinder local femoral blood supply. Moreover, the use of allograft has been associated with higher deep infection rates compared to lateral plating alone (8.3% vs. 3.8%) [19]. It becomes clear that despite advances in technology and biomechanical analysis, no implant or treatment method has proven to be a panacea for PPFFs.
The importance of achieving bicortical fixation around the femoral prosthesis should not be overlooked in the advent of locking plate and cable technology. Laterally based compression plates allow the insertion of non-locking bicortical screws that can be placed ‘off-axis’ around the femoral implant to allow for bicortical or transcortical fixation. This results in higher load to failure, torsional and sagittal bending stiffness than unicortical screws [20]. Our group has noted that positioning screws posterior to the femoral component to purchase the lesser trochanter has been a consistently successful to achieve additional proximal fixation. Moreover, a recent study of 212 Vancouver Type-B1 PPFFs found no advantage in re-operation rate between locking and non-locking plate fixation [5]. Locking plates have also been associated with potentially higher rates of non-union in these fractures [3], potentially due to overuse of locking screws creating an over-rigid construct.
Given the shortcomings of isolated lateral plating secured with locking screws and the use of allograft augmentation, our group continues to implement dual-plate fixation secured with predominantly off-axis non-locking screws for PPFFs. A lateral plate that spans the entire femur is particularly useful as the increased working length of the plate confers greater biomechanical stability and can decrease the incidence of varus collapse through greater tension band effect [21]. The addition of anterior plate further mitigates catastrophic failure by providing a tension band to resist the anterior tensile forces from the intrinsic femoral bow. It also provides more opportunities for screws fixation into limited proximal bone. Additionally, the anterior plate commonly offers the best trajectory for lag screws. These fractures demand a robust construct such as dual plating given the presence of osteopenic bone and decreased blood supply to the fracture secondary to the femoral implant in the intra-medullary canal [22]. In our series of 31 patients with an average age of 77.6 years, we noted an average radiographic healing time of 6 months. Average time to weight-bearing was 2.6 months, indicating further reliance on robust surgical fixation to prevent catastrophic failure.
Several studies highlight the advantages of orthogonal plating in the setting of PPFFs. Dual-plate constructs have demonstrated superior load to failure, mediolateral bending and torsional stiffness compared to single lateral plates with LAPs in periprosthetic fracture models [7, 8]. Choi et al. also determined that a dual-plating construct was stronger than a lateral plate with allograft and lateral plate alone [6]. Construct stability can be further increased with dual plates as it permits additional bicortical fixation in a multiplanar fashion adjacent to the femoral stem; we placed a mean of 6 bicortical screws in this series. Furthermore, dual plating allows more screws to be placed in the cement mantle if needed. Dual-plate fixation is particularly useful in the setting of inter-prosthetic femur fractures with a stemmed TKA. Clinically, Mueller et al. achieved good results in 9 of 10 patients with PPFFs treated with dual plating, although there were three nonunions [23]. Revision was needed for one patient given lateral plate failure, and the authors concluded dual-plating is a viable option for acute and salvage procedures with few complications. In a recent study of six PPFF nonunions, the authors achieved union in all patients treated with orthogonal plating constructs without the need for secondary procedures [24]. Finally, a recent systematic review concluded that dual plating of all types of femur fractures (native, periprosthetic and pathologic) can achieve good clinical outcomes [25].
Although there may be concern for additional soft tissue stripping required to place an anterior plate, we find this to be relatively negligible as necessary dissection is typically performed to properly visualize the fracture to ensure anatomic reduction (if indicated). Certainly, the additional dissection for an anterior 3.5 mm reconstruction plate pales in comparison to securing an allograft with cables. Moreover, application of a second plate is technically familiar to all surgeons, is readily accessible, and is less costly when compared to allograft use. In difficult fracture patterns, additional plates can be used as reduction aids, or can help maintain a reduction while a lateral working plate is applied. In our series, secondary plate location was dictated by fracture pattern. The majority of plates were secured anteriorly; however, medial and posterolateral plates were applied for fractures with distal extent. Notably, we had no cases of deep infection, which has been a concern in cases of dual-plate fixation due to periosteal blood supply injury. It is possible that the careful soft tissue dissection and preservation of periosteum protects against these issues.
In the current study, we achieved a high rate of union after the index procedure. Although the mean time to radiographic union was 6 months, the average time to weight-bearing was significantly shorter (2.6 months). Radiographic union likely lags behind clinical union assessed with history and physical examination at the time of follow-up. The latter should therefore be essential to the orthopedic surgeon when evaluating a patient post-operatively. Previous studies have reported re-operation rates from 9 to 26% for PPFFs to achieve union [3, 5]; whereas, only two patients (6%) required a secondary procedure to address nonunion in the current study. Moreover, no cases of deep infection requiring surgical debridement were identified here. This is in contrast to the use of allograft for PPFFs which has been associated with a deep infection rate up to 8.3% [19].
The current study is intrinsically limited by its lack of comparison group and its retrospective design. A prospective design with more patients and a comparison group would allow a more thorough analysis of risk factors for treatment failure. As such, the follow-up was variable and several patients were not followed beyond two years. This limitation, however, is frequently encountered in a geriatric trauma population, and our mean follow-up of 2 years is consistent with similar studies [18, 26,27,28,29,30]. Although no functional outcome scores were recorded, time to mobilization and time to union were measured, which arguably remain relevant clinical outcomes. Previous studies have reported the Harris Hip Score in the PPFF setting, although the clinical validity of this parameter without a comparative pre-injury score is potentially limited. Finally, the indication for dual-plate fixation, as opposed to a single lateral plate, was not recorded in this study. Our group employs liberal use of additional plate fixation as a means of fracture reduction or to address osteopenia or comminution, and as such, the decision to add a second plate is often made intra-operatively. Not all PPFFs require dual-plate fixation, but the current study demonstrates it is an acceptable technique for treatment.
Conclusion
In the current study of 31 periprosthetic femur fractures surrounding a stable hip arthroplasty stem, we achieved high union rates and low complications with orthogonal dual-plate fixation of PPFFs with a mean follow-up of approximately 2 years. Our results suggest that dual-plate fixation constructs are an acceptable fixation strategy for complex PPFFs. Our preferred fixation construct involves a lateral plate spanning the entire femur secured with non-locking bicortical screws supplemented with an anteriorly based reconstruction plate.
References
Ricci WM (2015) Periprosthetic femur fractures. J Orthop Trauma 29(3):130–137
Bates BD, Walmsley DW, Vicente MR et al (2018) An international, cross-sectional survey of the management of Vancouver type B1 periprosthetic femoral fractures around total hip arthroplasties. Injury 49(2):364–369
Dehghan N, McKee MD, Nauth A, Ristevski B, Schemitsch EH (2014) Surgical fixation of Vancouver type B1 periprosthetic femur fractures: a systematic review. J Orthop Trauma 28(12):721–727
Drew JM, Griffin WL, Odum SM, Van Doren B, Weston BT, Stryker LS (2016) Survivorship after periprosthetic femur fracture: factors affecting outcome. J Arthroplasty 31(6):1283–1288
Chatziagorou G, Lindahl H, Kärrholm J (2019) Surgical treatment of Vancouver type B periprosthetic femoral fractures: patient characteristics and outcomes of 1381 fractures treated in Sweden between 2001 and 2011. Bone Jt J 101-b(11):1447–1458
Choi JK, Gardner TR, Yoon E, Morrison TA, Macaulay WB, Geller JA (2010) The effect of fixation technique on the stiffness of comminuted Vancouver B1 periprosthetic femur fractures. J Arthroplasty 25(6 Suppl):124–128
Lenz M, Stoffel K, Gueorguiev B, Klos K, Kielstein H, Hofmann GO (2016) Enhancing fixation strength in periprosthetic femur fractures by orthogonal plating-a biomechanical study. J Orthop Res 34(4):591–596
Wähnert D, Grüneweller N, Gehweiler D, Brunn B, Raschke MJ, Stange R (2017) Double plating in Vancouver type B1 periprosthetic proximal femur fractures: a biomechanical study. J Orthop Res 35(2):234–239
Duncan CP, Masri BA (1995) Fractures of the femur after hip replacement. Instr Course Lect 44:293–304
Duncan CP, Haddad FS (2014) The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Jt J 96-B(6):713–716
Malige A, Yeazell S, Beck M, Liongson FA, Boateng H, Nwachuku C (2021) Union rate, complication rate, and opioid usage after Vancouver B periprosthetic femur fractures: a comparison of fracture types. Arch Orthop Trauma Surg 141(1):17–22
Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA (2006) Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma 20(2):89–93
Zdero R, Walker R, Waddell JP, Schemitsch EH (2008) Biomechanical evaluation of periprosthetic femoral fracture fixation. J Bone Jt Surg Am 90(5):1068–1077
Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE (2000) Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty 15(4):523–528
OʼConnell RS, Owen JR, Hansen EJ, et al (2018) Biomechanical evaluation of osteoporotic proximal periprosthetic femur fractures with proximal bicortical fixation and allograft struts. J Orthop Trauma 32(10):508–514
Khashan M, Amar E, Drexler M, Chechik O, Cohen Z, Steinberg EL (2013) Superior outcome of strut allograft-augmented plate fixation for the treatment of periprosthetic fractures around a stable femoral stem. Injury 44(11):1556–1560
Kim YH, Mansukhani SA, Kim JS, Park JW (2017) Use of locking plate and strut onlay allografts for periprosthetic fracture around well-fixed femoral components. J Arthroplasty 32(1):166–170
Yeo I, Rhyu KH, Kim SM, Park YS, Lim SJ (2016) High union rates of locking compression plating with cortical strut allograft for type B1 periprosthetic femoral fractures. Int Orthop 40(11):2365–2371
Moore RE, Baldwin K, Austin MS, Mehta S (2014) A systematic review of open reduction and internal fixation of periprosthetic femur fractures with or without allograft strut, cerclage, and locked plates. J Arthroplasty 29(5):872–876
Lenz M, Perren SM, Gueorguiev B et al (2014) A biomechanical study on proximal plate fixation techniques in periprosthetic femur fractures. Injury 45(Suppl 1):S71-75
Moloney GB, Westrick ER, Siska PA, Tarkin IS (2014) Treatment of periprosthetic femur fractures around a well-fixed hip arthroplasty implant: span the whole bone. Arch Orthop Trauma Surg 134(1):9–14
Clark D, Nakamura M, Miclau T, Marcucio R (2017) Effects of aging on fracture healing. Curr Osteoporos Rep 15(6):601–608
Muller FJ, Galler M, Fuchtmeier B (2014) Clinical and radiological results of patients treated with orthogonal double plating for periprosthetic femoral fractures. Int Orthop 38(12):2469–2472
Birch CE, Blankstein M, Chlebeck JD, Bartlett Rd CS (2017) Orthogonal plating of Vancouver B1 and C-type periprosthetic femur fracture nonunions. Hip Int 27(6):578–583
Lodde MF, Raschke MJ, Stolberg-Stolberg J, Everding J, Rosslenbroich S, Katthagen JC (2021) Union rates and functional outcome of double plating of the femur: systematic review of the literature. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03767-6
Froberg L, Troelsen A, Brix M (2012) Periprosthetic Vancouver type B1 and C fractures treated by locking-plate osteosynthesis: fracture union and reoperations in 60 consecutive fractures. Acta Orthop 83(6):648–652
Caruso G, Milani L, Marko T, Lorusso V, Andreotti M, Massari L (2018) Surgical treatment of periprosthetic femoral fractures: a retrospective study with functional and radiological outcomes from 2010 to 2016. Eur J Orthop Surg Traumatol 28(5):931–938
Ricci WM, Bolhofner BR, Loftus T, Cox C, Mitchell S, Borrelli J Jr (2005) Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am 87(10):2240–2245
Buttaro MA, Farfalli G, Paredes Nunez M, Comba F, Piccaluga F (2007) Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Jt Surg Am 89(9):1964–1969
Kammerlander C, Gosch M, Kammerlander-Knauer U, Luger TJ, Blauth M, Roth T (2011) Long-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg 131(10):1435–1444
Acknowledgements
The authors gratefully acknowledge Dr. Dean G. Lorich, who as both one of the orthopedic traumatologists who contributed cases for this study and as a mentor, educator and friend made a significant impact to his specialty. He is sorely missed by his colleagues, friends, patients and family.
Funding
The authors have no relevant financial or non-financial interests to disclose. No funding was sought or required for this research study. Institutional Review Board approval was obtained for this retrospective research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This research was performed at the Hospital for Special Surgery, New York, NY.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kubik, J.F., Bornes, T.D., Gausden, E.B. et al. Surgical outcomes of dual-plate fixation for periprosthetic femur fractures around a stable hip arthroplasty stem. Arch Orthop Trauma Surg 142, 3605–3611 (2022). https://doi.org/10.1007/s00402-021-03950-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03950-9