Abstract
Introduction
Low-grade Cutibacterium acnes (C. acnes) infections after shoulder surgery usually result in unexplained complaints. The absence of clinical signs of infection makes the incidence unclear and underreported. This study aimed to determine the incidence of C. acnes infections in patients with artificial material and unexplained persistent shoulder complaints. We hypothesized that the incidence of C. acnes infections would be higher in patients with artificial material. Risk factors and associations between culture time and contaminations/infections were also assessed.
Materials and methods
This retrospective cohort study included patients with and without artificial material undergoing revision shoulder surgery for persistent complaints after primary surgery and the suspicion of a low-grade infection. Three–six cultures were taken in all patients. C. acnes infection incidence was determined and logistic regression analysis was performed to identify risk factors. The association between time to culture growth and infections/contaminations was evaluated using Kaplan–Meier analysis and log-rank test.
Results
26/61 (42.6%) patients with and 14/33 (42.2%) without material had a C. acnes infection. Age (OR 0.959; 95% CI 0.914–1.000) and BMI (OR 0.884; 95% CI 0.787–0.977) were risk factors. Time to C. acnes culture positivity was not different between infections and contaminations.
Conclusion
The incidence of C. acnes infections was 42.6% in patients with artificial material and 42.2% in patients without artificial material. Younger age and lower BMI are risk factors. Low-grade C. acnes infections should be considered in patients with unexplained persistent complaints following shoulder surgery.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Cutibacterium acnes (C. acnes), formerly known as Propionibacterium acnes, is the most commonly detected pathogen during shoulder surgery [1,2,3,4,5]. It is suggested that C. acnes can contaminate the surgeon’s instruments or gloves when the sebaceous glands are cut [6] and can in that way contaminate the wound. When a low-grade infection is present, it can result in unexplained pain and stiffness, dysfunctional joints, or loosening of shoulder prostheses, which can affect patient outcomes [7,8,9].
Because of these non-specific symptoms without elevated infection parameters [4, 10], low-grade infections are often not considered. Consequently, the incidence of C. acnes infections is probably underestimated. C. acnes infections are currently diagnosed during revision surgery, when cultures are taken. To adequately detect C. acnes, 8–14 days of culturing are required [11,12,13]. Shorter cultivation times result in false-negative results, which contributes to the underestimation of C. acnes infections during shoulder surgery. Contrarily, longer cultivation times can result in false-positive cultures. Research has demonstrated that positive C. acnes cultures after 9 days were more associated with possible contamination; whereas, C. acnes infections showed positive cultures within one week after surgery [13, 14]. It is likely that a higher amount of bacteria are brought into culture in case of infections, and, therefore, show earlier positive cultures compared to contaminations. Therefore, timing of the first positive C. acnes cultures might help to distinguish between C. acnes infections and contaminations, which could aid in the decision to prescribe postoperative antibiotics.
To our knowledge, no studies have been performed that describe C. acnes infections in a comparative group of patients with or without artificial material in the shoulder. This study aimed to gain insight in the incidence of C. acnes infections in patients with pain and/or stiffness following shoulder surgery and the suspicion of a low-grade infection. Risk factors and differences in time to positivity between infections and contaminations were also assessed. We hypothesized that the incidence of C. acnes infections would be higher in patients with artificial material compared to those without, and that male gender and younger age would be risk factors. Moreover, we expected infections to have a shorter cultivation time than contaminations.
Materials and methods
A retrospective cohort study was performed including patients who underwent revision shoulder surgery because of suspicion of a low-grade infection due to unexplained persistent pain and/or stiffness, according to one surgeon. All patients with and without artificial material placement during primary surgery, and in whom cultures were taken during revision shoulder surgery (further referred to as target surgery) that took place between February 2016 and April 2018 were included. Patients were excluded if they had used antibiotics active against C. acnes two weeks prior to target surgery, if fewer than three tissue specimens were collected for culture, or if they showed overt clinical signs of infection (combined elevated infection parameters, wound leakage, fever). Demographic, clinical, microbiological, and therapeutic data were retrieved from patients’ medical records.
Prior to surgery, the skin was disinfected with iodine, or chlorhexidine in case of iodine allergy, and sterilely draped according to protocol. Prophylactic antibiotics were withhold until three–six cultures were taken from the subacromial bursal tissue, intra-articular synovial tissue, acromioclavicular joint capsular tissue or distal clavical bone, biceps tendon, the artificial material itself and/or adjacent soft tissue. Thereafter, the tissue specimens were transported to the microbiology laboratory.
Tissue cultures
All perioperative tissue cultures were put in transport containers, containing thioglycolate, and were processed within 6 h. First, specimens were manually homogenized in thioglycollate (Oxoid, Haarlem, The Netherlands). Thereafter, 100 µL of each suspension was plated onto New York City plates (Oxoid), sheep blood agar plates (Oxoid), and BBA anaerobic plates (Media Products, Groningen, the Netherlands), and 2 mL was inoculated into thioglycollate and brain–heart infusion broth. In an atmosphere of 5% CO2 and a temperature of 35 °C, aerobic cultures were incubated for 5 days. An anaerobic jar with an anaerobic gas mixture containing 80% nitrogen, 10% carbondioxide, and 10% hydrogen, was used to incubate anaerobic cultures. Aerobic plates were examined daily, while anaerobic plates were examined at 3 and 5 days.
After a 10-day incubation period and subculturing on solid media, broths were examined for bacterial growth the following 4 days. Matrix-assisted laser desorption/ionization time-of-flight (MaldiTof) mass spectrometry (Bruker, Bremen, Germany) was used to identify microorganisms. In addition, microorganisms were tested for antimicrobial susceptibility according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST).
Within 14 days after target surgery, final culture results were released. An infection was considered to be present when two or more tissue cultures were positive for the same microorganism. Hence, a C. acnes infection was diagnosed when at least two cultures from the surgical wound were positive for C. acnes. When only one culture was positive for C. acnes, the surgical wound was considered to be contaminated.
Treatment
Treatment of a native shoulder with a clinically high suspicion of a low-grade infection, based on shoulder stiffness during tests under general anesthesia and no other clear reason for the complaints, consisted of postoperative clindamycin until peroperative culture results were known. In case of positive cultures, clindamycin treatment was extended until 6 weeks postoperative when the bacterium showed to be sensitive to this antibiotic (otherwise, other antibiotics were prescribed). When there was a clinically low suspicion of a low-grade infection, based on a full-range of motion during testing under general anesthesia and other reasons for the complaints during shoulder arthroscopy, antibiotics were withhold until culture results were positive.
When a low-grade infection of a shoulder prosthesis was suspected, arthroscopic or mini-open biopsies were taken. A two-stage revision followed in case cultures showed the presence of a low-grade infection. First, six new cultures were taken, the prosthesis was extracted, and diluted betadine lavage was used to reduce bacterial load. After cultures were taken, cefazolin IV was started until the preliminary culture results were ready (5 days postoperative). In case of no bacteria growth, patients went home with clindamycin (or amoxicillin when resistance or intolerance for clindamycin occurred). Culture results were final after two weeks. If the antibiogram showed sensitivity, patients continued clindamycin treatment until six weeks postoperative, followed by an antibiotic holiday of at least two weeks and reimplantation of the prosthesis. During reimplantation, cultures were taken and antibiotics were given in the same way as described previously. When there was no bacteria growth, antibiotics were stopped. When a low-grade infection was detected, rifampicin was added to clindamycin with a maximum duration of three months. No spacers were used.
Statistical analysis
Demographic data, including gender, age, body mass index (BMI), smoking status, comorbidities, and history of cortisone injections, were summarized using descriptive statistics. In addition, information about the indication of primary surgery, the time between primary and target surgery, culture results, cultivation time, and if available, infection parameters were described. For patients with artificial material in the shoulder, primary surgery was defined as the surgery in which artificial material was placed for the first time; whereas, it was defined as the first surgery patients underwent in their lifetime for those without artificial material.
Furthermore, the percentage of C. acnes contaminations and cultures positive for other bacteria was determined. To identify variables associated with C. acnes infections in both groups, simple and multiple logistic regression analyses were performed. After simple logistic regression, variables were included in the multiple regression analysis based on clinical relevance and statistical significance (P < 0.2) between patients with and without C. acnes infections. Variables were checked for collinearity using the variance inflation factor (VIF). Variables were excluded from logistic regression analysis when more than 10% of the data was missing. One possible risk factor was included per ten events. Variables retained in the stepwise backward multiple logistic regression analysis when P < 0.05. Odds ratios (ORs), 95% confidence intervals (CI), and Wald Chi-square P values were presented per variable. To obtain better fitted parameter estimates and ORs, bootstrapping was performed for internal validation.
The association between time to C. acnes growth and C. acnes infections and contaminations was also evaluated. For infections, the cultivation time was calculated until the date at which the first culture was positive for C. acnes. To visualize the time to C. acnes culture growth separately for patients with infections and contaminations, a Kaplan–Meier analysis was performed. Kaplan–Meier curves showed the proportion of patients in whom C. acnes was detected over time, and these curves were tested for significant differences using the log-rank test.
All statistical analyses were performed using SPSS version 21 with a statistical significance level of P < 0.05.
Ethics
This study was approved by the institutional review board of the Sint Maartenskliniek Nijmegen (entry no. 2017-0802).
Results
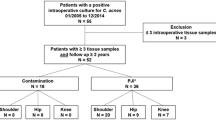
Between February 2016 and April 2018, 118 surgeries were performed in which perioperative cultures were taken. In total, 24 patients met the exclusion criteria (Fig. 1), resulting in 94 patients eligible for inclusion in this study.
The different indications for artificial material placement during primary surgery are listed in Table 1. Five patients without artificial material who did not have primary surgery underwent target surgery for suspicion of an infection after shoulder injections; all other patients in the control group did have previous shoulder surgery on the affected shoulder. In one patient, the date of primary surgery was unknown. For patients with artificial material, insoluble suture material, wires, anchors, screws, pins, plates, prosthesis, or a combination thereof were placed into the shoulder area during shoulder surgery. Median time from primary to target surgery for all patients was 30.5 (IQR 14.0–87.8) and, respectively, 26.0 (IQR 14.0–87.5) and 41.0 (IQR 15.0–99.0) months for patients with and without artificial material separately.
During target surgery, 40 patients (42.6%) had at least two positive cultures for C. acnes (Table 2). C. acnes infections occurred in 26 of the 61 (42.6%) patients with and in 14 of the 33 (42.2%) patients without artificial material. The number of C. acnes infections after different surgery indications is shown in Table 1. Only four patients (all with artificial material) had at least two positive cultures for other bacteria (7.1%), which were S. saccharolyticus, S. capitis, S. epidermis or S. lugdunensis. Three of them also had a C. acnes infection.
After target surgery, 16 patients underwent another revision surgery in which cultures were taken. Of these patients, nine had a C. acnes infection. Five of these patients also had a C. acnes infection detected during previous target surgery, for which four of them were treated with antibiotics (clindamycin).
Characteristics of patients with and without a C. acnes infection are shown in Table 3. Noticeably, most patients with a C. acnes infection were men, while most patients without were women. Additionally, patients with C. acnes infections were on average 6 years younger at the time of primary surgery than patients without infections. Of the 24 patients with prior revision surgeries at the same shoulder, 16 had one revision surgery, five had two revision surgeries, two had three revision surgeries, and one had four revision surgeries before target surgery. More specifically, seven out of the 16 patients with one prior revision surgery and four out of five patients with two prior revision surgeries had a C. acnes infection.
Infection parameters were not measured in all patients between the time of primary surgery and revision surgery. ESR, CRP, and leukocyte levels were available in 28, 30, and 29 patients, respectively. Between primary target surgery, 3 patients had only elevated ESR levels (> 20 mm/u), 3 had solely elevated CRP levels (> 10 mg/L), none had solely elevated leukocytes levels (> 11 × 109/L), and 4 had a combination of elevated infection parameters. Of these 10 patients with elevated infection parameters, 3 had a C. acnes infection. There were 3 patients with rheumatoid arthritis among the patients with elevated infection parameters, of whom one also had a C. acnes infection.
Logistic regression
Simple logistic regression showed that gender, age at primary surgery, BMI, diabetes, history of cortisone injections, and time between primary surgery and complaints were associated (P < 0.2) with C. acnes infections (Table 4). Based on significance and relevance, gender, age, BMI, and a history of cortisone injections were included in the backward multiple logistic regression model (Table 5). There was no collinearity between those variables (VIFs all below 1.1). Age at primary surgery (OR 0.962; 95% CI 0.925–1.000) and BMI (OR 0.891; 95% CI 0.802–0.990) retained in the regression model, indication an association between these variables and the presence of C. acnes infections. After internal validation using bootstrapping, ORs for age at primary surgery and BMI decreased to 0.959 (95% CI 0.914–1.000) and 0.884 (95% CI 0.787–0.977), respectively (Table 6).
Cultivation time
In six patients, a C. acnes contamination was identified. Median time to detect the 1st positive culture was 6.0 (IQR 5.0–7.0) days in the infection group and 7.0 (IQR 4.8–10.0) days in the contamination group. Kaplan–Meier curves (Fig. 2) showed the probability of a positive C. acnes culture over time, separately for contaminations and infections. The log-rank test, comparing these curves, showed that the time to first C. acnes culture was not statistically significantly different between the infection and contamination group (P = 0.219).
Discussion
The incidence of low-grade C. acnes shoulder infections was identified in patients with unexplained persistent pain and/or stiffness following surgery with or without implantation of different kinds of artificial material. The incidence of low-grade C. acnes infections was 42.6% in patients with and 42.2% in patients without artificial material. Other bacterial infections occurred in 4 patients (7.1%). Hence, low-grade C. acnes infections remain the most commonly isolated pathogens after shoulder surgery.
Several studies investigated the incidence of positive perioperative cultures during revision surgery in patients without overt clinical signs of infection [1, 4, 5, 7, 9, 11, 15,16,17,18,19,20]. They found a C. acnes incidence ranging from 4.4 to 79.4%. Comparison of the incidence of C. acnes infections is difficult, since studies used different methods to calculate the incidence. In one study [20], it was not clear how a wound contamination was distinguished from an infection; while, others [1, 5, 7, 9, 15,16,17,18] only looked at the incidence of at least one positive C. acnes culture. This might have overestimated their results. Other studies [5, 15, 17] calculated the incidence by dividing the number of surgeries with a positive C. acnes culture by the total amount of revision surgeries, which might lead to an underestimation of the results, since cultures were not routinely collected. Three studies calculated the incidence of C. acnes infections similar as in our study; by dividing the number of C. acnes infections (≥ 2 positive cultures) by the number of surgeries in which cultures were taken [4, 11, 19]. They found a C. acnes incidence ranging from 4.4 to 9.5%. These results are lower than our C. acnes incidence, which might be explained by the setting. The Sint Maartenskliniek is a tertiary referral center, where a relatively high number of patients are seen for unexplained persistent shoulder complaints after previous surgeries compared to other hospitals. Since patients with C. acnes infections frequently do not have typical infection signs, surgeons in other hospitals may not consider a low-grade infection. As a consequence, these patients are not treated and no perioperative cultures are taken during revision surgery in other hospitals; while, surgeons in our hospital are more aware of possible low-grade infections and are, thus, motivated to take routine cultures during surgery. In addition, one may imagine that the C. acnes incidence is lower in patients who undergo revision surgery for an obvious reason, such as a periprosthetic fracture or rotator cuff failure in case of an anatomical shoulder prosthesis, compared to unexplained persistent pain and/or stiffness.
Gender, age at primary surgery, BMI, diabetes, a history of cortisone injections, and time between primary surgery and complaints were risk factors considered to be in the multiple regression model (P < 0.2). Logistic regression analysis showed that age at primary surgery and BMI were associated with the presence of low-grade C. acnes infections, with each year increase in age and each kg/m2 increase in BMI representing a 4.1% and 11.6% lower risk of C. acnes infections, respectively. This finding of young age as a risk factor is supported by previous studies [18, 21,22,23,24] and may be explained by the fact that younger people have more sebum production, which is favorable for C. acnes colonization [25, 26]. Multiple studies [4, 7, 17, 18, 21,22,23,24, 27,28,29,30] have been performed identifying factors associated with shoulder infections, but most of these studies lacked regression analysis and were, therefore, not able to identify independent risk factors. To our knowledge, five studies performed regression analysis and found the following risk factors: younger age, male gender, obesity, depression, malnutrition, intraoperative steroid injections, chronic anemia, reverse total shoulder prosthesis, and traumatic shoulder arthroplasties [7, 21,22,23,24]. Our study did not find obesity to be a risk factor for C. acnes infections. On the contrary, a higher BMI was found to decrease the risk. This is biologically speaking not logical because of multiple findings that obesity increases the risk of infections due to an impaired immune response [31, 32]. However, our finding could be explained by the selected study population, since most patients with unexplained complaints are referred to our clinic for a second/third opinion. It is possible that patients with such complaints and a higher BMI have shoulder complaints due to obesity. Consequently, a higher BMI looks like a protective factor of C. acnes infections. Hence, the finding of a lower BMI as a risk factor for C. acnes infections is not generalizable to other populations. However, our study does support the evidence that younger age is a risk factor for C. acnes infections.
Limitations
The main limitation of this study includes the small sample size. Due to this limitation, we were not able to identify all factors associated with the presence of C. acnes infections. To prevent overfitting of the model, it is possible that some relevant risk factors were not included in our analysis.
Another limitation is the retrospective design of this study, which did not allow us to take all possible risk factors into account. We may, therefore, have missed some relevant patient-related risk factors. However, based on findings of other studies, we expect that most important patient-related risk factors, such as age, gender, and BMI, were included in this study. Because of the retrospective design, there may also have been selection bias.
Clinical relevance
Unlike what we expected, the incidence of C. acnes infections in the group with artificial material was not different from the group without and therefore, one should take C. acnes infections in mind when unexplained persistent shoulder complaints are present. However, we expected a difference in treatment effect between both groups. Some artificial materials, like suture anchors for rotator cuff or labral tear repair, cannot be removed without severe damage to the shoulder anatomy. In case of a chronic low-grade C. acnes infection, the question is if open or arthroscopic irrigation followed by antibiotic treatment is an effective infection treatment as long as such suture anchors are still in situ. This question will be the subject of our future research.
Conclusion
The incidence of C. acnes infections in patients undergoing revision surgery for unexplained persistent complaints after artificial material placement was 42.6%. Younger age and a lower BMI at primary surgery were risk factors for C. acnes infections. Furthermore, cultivation time was not significantly different between true infections and contaminations.
We recommend that orthopedic surgeons should consider low-grade C. acnes infections in patients with unexplained persistent shoulder complains following shoulder surgery, like pain and/or stiffness.
References
Kelly JD 2nd, Hobgood ER (2009) Positive culture rate in revision shoulder arthroplasty. Clin Orthop Relat Res 467(9):2343–2348. https://doi.org/10.1007/s11999-009-0875-x
Achermann Y, Sahin F, Schwyzer HK, Kolling C, Wust J, Vogt M (2013) Characteristics and outcome of 16 periprosthetic shoulder joint infections. Infection 41(3):613–620. https://doi.org/10.1007/s15010-012-0360-4
Athwal GS, Sperling JW, Rispoli DM, Cofield RH (2007) Deep infection after rotator cuff repair. J Shoulder Elbow Surg 16(3):306–311. https://doi.org/10.1016/j.jse.2006.05.013
Horneff JG 3rd, Hsu JE, Voleti PB, O'Donnell J, Huffman GR (2015) Propionibacterium acnes infection in shoulder arthroscopy patients with postoperative pain. J Shoulder Elbow Surg 24(6):838–843. https://doi.org/10.1016/j.jse.2015.03.008
Kim SJ, Kim JH (2014) Unexpected positive cultures including isolation of Propionibacterium acnes in revision shoulder arthroplasty. Chin Med J (Engl) 127(22):3975–3979
Falconer TM, Baba M, Kruse LM, Dorrestijn O, Donaldson MJ, Smith MM, Figtree MC, Hudson BJ, Cass B, Young AA (2016) Contamination of the surgical field with Propionibacterium acnes in primary shoulder arthroplasty. J Bone Joint Surg Am 98(20):1722–1728. https://doi.org/10.2106/jbjs.15.01133
Pottinger P, Butler-Wu S, Neradilek MB, Merritt A, Bertelsen A, Jette JL, Warme WJ, Matsen FA 3rd (2012) Prognostic factors for bacterial cultures positive for Propionibacterium acnes and other organisms in a large series of revision shoulder arthroplasties performed for stiffness, pain, or loosening. J Bone Joint Surg Am 94(22):2075–2083. https://doi.org/10.2106/jbjs.k.00861
Zeller V, Ghorbani A, Strady C, Leonard P, Mamoudy P, Desplaces N (2007) Propionibacterium acnes: an agent of prosthetic joint infection and colonization. J Infect 55(2):119–124. https://doi.org/10.1016/j.jinf.2007.02.006
Cheung EV, Sperling JW, Cofield RH (2008) Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg 17(3):371–375. https://doi.org/10.1016/j.jse.2007.09.003
Schneeberger AG, Gilbart MK, Sheikh R, Gerber C, Ruef C (2009) Non-purulent low-grade infection as cause of pain following shoulder surgery: preliminary results. Chir Organi Mov 93(Suppl 1):S71–77. https://doi.org/10.1007/s12306-009-0010-x
Butler-Wu SM, Burns EM, Pottinger PS, Magaret AS, Rakeman JL, Matsen FA 3rd, Cookson BT (2011) Optimization of periprosthetic culture for diagnosis of Propionibacterium acnes prosthetic joint infection. J Clin Microbiol 49(7):2490–2495. https://doi.org/10.1128/jcm.00450-11
Schafer P, Fink B, Sandow D, Margull A, Berger I, Frommelt L (2008) Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin Infect Dis 47(11):1403–1409. https://doi.org/10.1086/592973
Bossard DA, Ledergerber B, Zingg PO, Gerber C, Zinkernagel AS, Zbinden R, Achermann Y (2016) Optimal length of cultivation time for isolation of Propionibacterium acnes in suspected bone and joint infections is more than 7 days. J Clin Microbiol 54(12):3043–3049. https://doi.org/10.1128/jcm.01435-16
Frangiamore SJ, Saleh A, Grosso MJ, Alolabi B, Bauer TW, Iannotti JP, Ricchetti ET (2015) Early versus late culture growth of Propionibacterium acnes in revision shoulder arthroplasty. J Bone Joint Surg Am 97(14):1149–1158. https://doi.org/10.2106/jbjs.n.00881
Topolski MS, Chin PY, Sperling JW, Cofield RH (2006) Revision shoulder arthroplasty with positive intraoperative cultures: the value of preoperative studies and intraoperative histology. J Shoulder Elbow Surg 15(4):402–406. https://doi.org/10.1016/j.jse.2005.10.001
Grosso MJ, Frangiamore SJ, Ricchetti ET, Bauer TW, Iannotti JP (2014) Sensitivity of frozen section histology for identifying Propionibacterium acnes infections in revision shoulder arthroplasty. J Bone Joint Surg Am 96(6):442–447. https://doi.org/10.2106/jbjs.m.00258
Foruria AM, Fox TJ, Sperling JW, Cofield RH (2013) Clinical meaning of unexpected positive cultures (UPC) in revision shoulder arthroplasty. J Shoulder Elbow Surg 22(5):620–627. https://doi.org/10.1016/j.jse.2012.07.017
Khan U, Torrance E, Townsend R, Davies S, Mackenzie T, Funk L (2017) Low-grade infections in nonarthroplasty shoulder surgery. J Shoulder Elbow Surg 26(9):1553–1561. https://doi.org/10.1016/j.jse.2017.01.008
McGoldrick E, McElvany MD, Butler-Wu S, Pottinger PS, Matsen FA 3rd (2015) Substantial cultures of Propionibacterium can be found in apparently aseptic shoulders revised three years or more after the index arthroplasty. J Shoulder Elbow Surg 24(1):31–35. https://doi.org/10.1016/j.jse.2014.05.008
Both A, Klatte TO, Lubke A, Buttner H, Hartel MJ, Grossterlinden LG, Rohde H (2018) Growth of Cutibacterium acnes is common on osteosynthesis material of the shoulder in patients without signs of infection. Acta Orthop 89(5):580–584. https://doi.org/10.1080/17453674.2018.1489095
Richards J, Inacio MC, Beckett M, Navarro RA, Singh A, Dillon MT, Sodl JF, Yian EH (2014) Patient and procedure-specific risk factors for deep infection after primary shoulder arthroplasty. Clin Orthop Relat Res 472(9):2809–2815. https://doi.org/10.1007/s11999-014-3696-5
Singh JA, Sperling JW, Schleck C, Harmsen WS, Cofield RH (2012) Periprosthetic infections after total shoulder arthroplasty: a 33-year perspective. J Shoulder Elbow Surg 21(11):1534–1541. https://doi.org/10.1016/j.jse.2012.01.006
Morris BJ, O'Connor DP, Torres D, Elkousy HA, Gartsman GM, Edwards TB (2015) Risk factors for periprosthetic infection after reverse shoulder arthroplasty. J Shoulder Elbow Surg 24(2):161–166. https://doi.org/10.1016/j.jse.2014.05.020
Cancienne JM, Brockmeier SF, Carson EW, Werner BC (2018) Risk Factors for infection after shoulder arthroscopy in a large medicare population. Am J Sports Med 46(4):809–814. https://doi.org/10.1177/0363546517749212
Pochi PE, Strauss JS, Downing DT (1979) Age-related changes in sebaceous gland activity. J Invest Dermatol 73(1):108–111
McGinley KJ, Webster GF, Ruggieri MR, Leyden JJ (1980) Regional variations in density of cutaneous propionibacteria: correlation of Propionibacterium acnes populations with sebaceous secretion. J Clin Microbiol 12(5):672–675
Sethi PM, Sabetta JR, Stuek SJ, Horine SV, Vadasdi KB, Greene RT, Cunningham JG, Miller SR (2015) Presence of Propionibacterium acnes in primary shoulder arthroscopy: results of aspiration and tissue cultures. J Shoulder Elbow Surg 24(5):796–803. https://doi.org/10.1016/j.jse.2014.09.042
Patel A, Calfee RP, Plante M, Fischer SA, Green A (2009) Propionibacterium acnes colonization of the human shoulder. J Shoulder Elbow Surg 18(6):897–902. https://doi.org/10.1016/j.jse.2009.01.023
Hudek R, Sommer F, Kerwat M, Abdelkawi AF, Loos F, Gohlke F (2014) Propionibacterium acnes in shoulder surgery: true infection, contamination, or commensal of the deep tissue? J Shoulder Elbow Surg 23(12):1763–1771. https://doi.org/10.1016/j.jse.2014.05.024
Wang B, Toye B, Desjardins M, Lapner P, Lee C (2013) A 7-year retrospective review from 2005 to 2011 of Propionibacterium acnes shoulder infections in Ottawa, Ontario. Canada Diagn Microbiol Infect Dis 75(2):195–199. https://doi.org/10.1016/j.diagmicrobio.2012.10.018
Abdallah DY, Jadaan MM, McCabe JP (2013) Body mass index and risk of surgical site infection following spine surgery: a meta-analysis. Eur Spine J 22(12):2800–2809. https://doi.org/10.1007/s00586-013-2890-6
Dobner J, Kaser S (2018) Body mass index and the risk of infection: from underweight to obesity. Clin Microbiol Infect 24(1):24–28. https://doi.org/10.1016/j.cmi.2017.02.013
Funding
This research did not receive grants from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author declares that there is no conflict of interest.
Ethical review committee statement
This study was approved by the institutional review board of the Sint Maartenskliniek Nijmegen (entry no. 2017-0802).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was performed at the Sint Maartenskliniek Nijmegen, except for the medical microbiology part, which was performed at the Canisius-Wilhelmina Hospital Nijmegen.
Rights and permissions
About this article
Cite this article
Pruijn, N., van Diek, F.M., Meis, J.F. et al. Cutibacterium acnes infections in revision surgery for persistent shoulder complaints: a retrospective cohort study. Arch Orthop Trauma Surg 141, 197–205 (2021). https://doi.org/10.1007/s00402-020-03415-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03415-5