Abstract
Introduction
Proximal humeral fracture-dislocations can occur in high-energy traumas. This injury can be accompanied by a glenoid fracture; however, it is a rare type of complex injury in patients aged under 60 years.
Materials and methods
A 53-year-old man presented with a three-part fracture-dislocation of the proximal humerus and a severely comminuted glenoid fracture. For the glenohumeral dislocation and proximal humeral fracture, we performed closed reduction using a threaded Steinman pin and fixation with percutaneous cannulated screws. Using arthroscopy, while maintaining humeral traction with the Steinman pin, the intra-articular glenoid fragments were reduced and then fixed with a buttressing headless screw and one suture anchor. After a 6-week immobilization with a shoulder spica cast, rehabilitation was initiated.
Results
We confirmed bony union of the fracture sites after 6 months post-surgery. The patient showed excellent clinical outcomes with a nearly full range of motion without instability
Conclusions
We reported a successful outcome for a complex proximal humeral fracture involving the glenoid using closed reduction and fixation for the proximal humeral fracture and arthroscopic reduction and fixation for the comminuted anteroinferior glenoid fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humerus fracture (PHF) is a common injury in adult patients, accounting for about 6–7% of all adult fractures [1, 2]. Its incidence increases in both men and women aged ≥ 50 years [2]. However, the combined injury of a PHF with a glenoid fracture is relatively uncommon, especially in patients aged < 60 years. Shoulder dislocation occurs in two-thirds of all large anterior glenoid rim fractures [3] and makes the treatment of this combined injury technically challenging.
Several studies have described the operative reduction and fixation techniques [4] for glenohumeral joint fracture-dislocation and their favorable outcomes [5, 6]. Although there is still a debate on the necessity of operative treatment [7], glenoid fractures with a concomitant PHF involving the greater tuberosity require early operative stabilization due to susceptibility to re-dislocation [8].
In this report, we describe a rare case of a middle-aged patient in whom a comminuted glenoid fracture with anterior dislocation was managed by arthroscopic reduction and fixation using a headless screw and suture anchor, and a complex PHF was managed by percutaneous cannulated screw fixation.
Case report
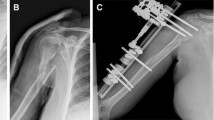
A 53-year-old man was referred to our hospital with right shoulder pain caused by falling off a bicycle on the same day. He had a medical history of osteomyelitis of the right proximal humerus, which occurred 40 years ago and was treated by surgical curettage without any residual sequelae. An initial plain radiography scan revealed a complex PHF with glenohumeral joint anterior dislocation (Fig. 1a). A computed tomography (CT) scan confirmed comminuted greater tuberosity and a surgical neck fracture on the proximal humerus (Neer classification, three parts), along with a glenoid fracture in the anteroinferior portion (Ideberg classification, type Ia) that involved 28% of the surface, as determined by a linear-based method, with severe comminution (Fig. 1b). We did not attempt manual reduction in the emergency room because such a dislocation is difficult to reduce and is susceptible to re-dislocation, and the procedure can worsen the displacement of the PHF fragments. There was no sign of a neurovascular injury.
The operation was performed on the 5th day after trauma. With a beach chair position, we planned closed reduction and screw fixation for the PHF and arthroscopic reduction and fixation for the glenoid fracture to minimize injury to the vascularity of the humeral head. We also prepared for an anatomic and reverse total shoulder arthroplasty (RTSA) in case the arthroscopic procedure failed.
First, we performed reduction of the dislocated humeral head by inserting a fully threaded 2.4-mm Steinmann pin (S-pin) into the fragment to use it as a joystick with a chuck (Fig. 2a), under fluoroscopic guidance (Fig. 2b). After the reduction (Fig. 2c), we inserted four 4.0-mm cannulated screws (Biotech, Wiesbaden, Germany) to fix the humeral head with the distal fragment in an acceptable alignment. We did not fix the greater tuberosity fragments because of severe comminution and minimal displacement of the comminuted fragments. For glenoid fixation, we retracted the humerus laterally using the threaded S-pin and introduced an arthroscope through the posterior portal. After identifying the comminuted anterior glenoid fracture and the intact rotator cuff, we created an anterosuperior portal to visualize the fracture site directly and an anteroinferior portal for performing the fixation. We tried to fix the bone fragments directly using headless screws with guidewires, but failed due to severe comminution (Fig. 3a). Instead, after elevating the depressed articular fragments under arthroscopic and fluoroscopic guidance (Fig. 3b), we inserted a buttressing headless cannulated screw (3.0 × 36.0 mm; Medartis, Basel, Switzerland) into the anterior glenoid rim through the anterior 5-o’ clock portal to maintain a reduced status of the comminuted glenoid parts (Fig. 3c). Thereafter, we inserted one Y-Knot suture-anchor (1.3 mm; Conmed Linvatec, Largo, FL, USA) into the anterior glenoid rim to fix the comminuted bone fragments with the anterior labrum (Fig. 3d). After skin closure, a shoulder spica cast was applied to maintain joint stability.
Reduction and fixation of the glenoid fracture. Severe comminution of the glenoid fragments is noted on arthroscopic examination (a). After reduction of the fragments under arthroscopy and fluoroscopy (b), a buttressing cannulated screw is inserted into the anterior glenoid rim (c). A well-reduced status is confirmed (d). A, arthroscope; C, humeral cannulated screw; S, Steinman pin; D, dura elevator
A postoperative radiograph confirmed that the shoulder joint and fracture fragments were well reduced (Fig. 4). After 6 weeks, we removed the cast and started rehabilitation, which began from a passive range of motion (ROM) and progressed to an active ROM at 8 weeks. After 6 months from the operation, a nearly full ROM was noted without instability (active elevation of 150°, internal rotation L4–5 level; Fig. 5); the VAS pain score was 0 and the DASH score was 8.3. Union of the proximal humerus and glenoid was noted on plain radiography (Fig. 6a, b) and CT scans (Fig. 6c, d) at the same visit. No operation-related complication was reported during the 12-month follow-up period.
Informed consent was obtained from the patient for the use and publication of data for academic purposes.
Discussion
In this case, the patient was a healthy and active middle-aged man with a medical history of osteomyelitis of the proximal humerus when he was younger. However, we assumed that it was irrelevant to this injury because we observed cortical thickening of the proximal shaft of the humerus, distant from the fracture lines, on radiography.
Three- and four-part PHFs can be managed successfully by fixation using the locking plate technique [9, 10], but there are several reports of a relatively high risk of reoperation and complications, such as screw penetration, non-union, and avascular necrosis of the humeral head [11,12,13,14]. To avoid these, other treatment options such as arthroplasty, percutaneous pinning, or screw fixation can be pursued. Ortmaier et al. [15] reported using the Humerusblock (Synthes, Oberdorf, Switzerland) for closed reduction and percutaneous fixation, with favorable functional outcomes and a complication rate lower than that of the locking plate fixation. However, there remains a lack of consensus on the necessity [16, 17] and choice of surgical treatment for complex PHF [18, 19]. In our case, the posterior anatomical neck and the medial hinge of the humerus were comminuted; thus, we assumed that the vascularity of the head was at risk; according to Hertel’s study in 2004 [20], these are poor predictors of head ischemia. Considering the patient’s age, we performed multiple percutaneous screw fixation to reduce the risk of head necrosis and minimize the prolonged limitation of motion due to post-operative adhesion.
Over 30 years, several studies have reported favorable outcomes of arthroplasty for PHFs. Hemiarthroplasty is the most widely used technique for the treatment of complex fractures; however, several recent studies have reported greater unfavorable outcomes for this technique than for RTSA, mainly due to problems with tuberosity healing and rotator cuff dysfunction [21, 22]. In our case, we prepared for RTSA with a glenoid bone graft as well as hemiarthroplasty, in case stable fixation of the glenoid was not possible due to severe comminution and defect. RTSA is mostly performed in complicated cases (such as non-union after primary osteosynthesis), providing improved functional outcomes and a significant reduction in pain [23, 24]. Recently, its application has been broadened to include primary fixation of complex PHFs in elderly patients [25, 26]. However, due to insufficient research on the longevity of shoulder arthroplasty and the risk of revision, it should be considered as a salvage procedure in younger patients.
Due to its rarity, there are very few reports on the management of PHF with glenoid fracture-dislocation. Garofalo et al. [27] reported satisfactory short-term outcomes of RTSA using a glenoid bone graft in 26 patients. Maassen [28] reported a PHF with concomitant glenoid fracture, which were treated with RTSA and internal fixation using two headless compression screws for the glenoid. These two studies were conducted in elderly patients (aged between 63 and 75 years). Considering that our patient was a 53-year-old man who was still active, RTSA was not a feasible treatment option. Furthermore, because the glenoid fracture was comminuted, we determined that postoperative adhesion would be severe if we attempted an open reduction and fixation for the glenoid. Thus, we performed an arthroscopic glenoid reduction and fixation, along with percutaneous fixation of the proximal humerus with cannulated screws.
There are several reports on arthroscopic anterior glenoid fixation, and various methods have been introduced for the same, including trans-osseous repair with suture anchor or endobutton and fixation with headless screws [29,30,31]. However, it is not easy to fix large bone fragments firmly due to a limited access to the fracture site and the use of the fixation devices. Sano et al. [31] reported an excellent functional outcome after a 1-year follow-up for a patient treated with arthroscopic screw and suture anchor fixation for an anterior glenoid fracture involving 40% of the glenoid fossa. It is more difficult to perform this procedure in injuries of comminuted glenoid fractures with concomitant complex PHFs. We used a threaded S-pin, which was inserted for humeral head reduction, to retract the proximal humeral component safely during the arthroscopic procedure. After the fixation of the glenoid with a screw and a suture anchor, the shoulder joint was immobilized with a spica cast, due to large bony fragments involving more than 30% of the surface and severe comminution of the glenoid.
Conclusion
Glenoid fracture-dislocation with complex PHF is extremely rare in middle-aged individuals, and its treatment is technically difficult. To the best our knowledge, this is the first case of a glenoid fracture-dislocation with concomitant complex PHF in a middle-aged patient that was treated using an arthroscopic buttressing screw and suture anchor fixation for the glenoid, in combination with a minimally invasive percutaneous screw fixation for the PHF. We report that this rare case has satisfactory clinical and radiological results. Although the technique is difficult to perform, considering that such combined injuries are rare in the middle-aged population, it seems to be a promising treatment option.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697. https://doi.org/10.1016/j.injury.2006.04.130
Rosengren BE, Karlsson M, Petersson I, Englund M (2015) The 21st-century landscape of adult fractures: cohort study of a complete adult regional population. J Bone Miner Res 30(3):535–542. https://doi.org/10.1002/jbmr.2370
Ideberg R, Grevsten S, Larsson S (1995) Epidemiology of scapular fractures incidence and classification of 338 fractures. Acta Orthop Scand 66(5):395–397
Varghese J, Thilak J, Mahajan CV (2006) Arthroscopic treatment of acute traumatic posterior glenohumeral dislocation and anatomic neck fracture. Arthroscopy 22(6):676.e671–672. https://doi.org/10.1016/j.arthro.2005.08.056
Raiss P, Baumann F, Akbar M, Rickert M, Loew M (2009) Open screw fixation of large anterior glenoid rim fractures: mid- and long-term results in 29 patients. Knee Surg Sports Traumatol Arthrosc 17(2):195–203. https://doi.org/10.1007/s00167-008-0677-9
Tauber M, Moursy M, Eppel M, Koller H, Resch H (2008) Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc 16(3):326–332. https://doi.org/10.1007/s00167-007-0437-2
Maquieira GJ, Espinosa N, Gerber C, Eid K (2007) Non-operative treatment of large anterior glenoid rim fractures after traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br 89(10):1347–1351. https://doi.org/10.1302/0301-620x.89b10.19273
Robinson CM, Kelly M, Wakefield AE (2002) Redislocation of the shoulder during the first six weeks after a primary anterior dislocation: risk factors and results of treatment. J Bone Joint Surg Am 84(9):1552–1559. https://doi.org/10.2106/00004623-200209000-00007
Aguado HJ, Mingo J, Torres M, Alvarez-Ramos A, Martin-Ferrero MA (2016) Minimally invasive polyaxial locking plate osteosynthesis for 3–4 part proximal humeral fractures: our institutional experience. Injury 47(Suppl 3):S22–S28. https://doi.org/10.1016/s0020-1383(16)30602-7
Trikha V, Singh V, Choudhury B, Das S (2017) Retrospective analysis of proximal humeral fracture-dislocations managed with locked plates. J Shoulder Elbow Surg 26(10):e293–e299. https://doi.org/10.1016/j.jse.2017.03.035
Wijgman AJ, Roolker W, Patt TW, Raaymakers EL, Marti RK (2002) Open reduction and internal fixation of three- and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am 84(11):1919–1925
Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF (2010) Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 19(4):489–494. https://doi.org/10.1016/j.jse.2009.09.005
Gupta AK, Harris JD, Erickson BJ, Abrams GD, Bruce B, McCormick F, Nicholson GP, Romeo AA (2015) Surgical management of complex proximal humerus fractures—a systematic review of 92 studies including 4500 patients. J Orthop Trauma 29(1):54–59. https://doi.org/10.1097/bot.0000000000000229
Beeres FJP, Hallensleben NDL, Rhemrev SJ, Goslings JC, Oehme F, Meylaerts SAG, Babst R, Schep NWL (2017) Plate fixation of the proximal humerus: an international multicentre comparative study of postoperative complications. Arch Orthop Trauma Surg 137(12):1685–1692. https://doi.org/10.1007/s00402-017-2790-z
Ortmaier R, Filzmaier V, Hitzl W, Bogner R, Neubauer T, Resch H, Auffarth A (2015) Comparison between minimally invasive, percutaneous osteosynthesis and locking plate osteosynthesis in 3- and 4-part proximal humerus fractures. BMC Musculoskelet Disord 16:297. https://doi.org/10.1186/s12891-015-0770-4
Mao F, Zhang DH, Peng XC, Liao Y (2015) Comparison of surgical versus non-surgical treatment of displaced 3- and 4-part fractures of the proximal humerus: a meta-analysis. J Invest Surg 28(4):215–224
Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, Goodchild L, Chuang LH, Hewitt C, Torgerson D (2015) Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. J Am Med Assoc 313(10):1037–1047. https://doi.org/10.1001/jama.2015.1629
Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K (2012) Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma 26(2):98–106. https://doi.org/10.1097/BOT.0b013e31821c2e15
Solberg BD, Moon CN, Franco DP, Paiement GD (2009) Surgical treatment of three- and four-part proximal humeral fractures. J Bone Joint Surg Am 91(7):1689–1697. https://doi.org/10.2106/jbjs.H.00133
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13(4):427–433. https://doi.org/10.1016/j.jse.2004.01.034
Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV (2015) Reverse shoulder arthroplasty versus hemiarthroplasty for treatment of proximal humerus fractures. J Shoulder Elbow Surg 24(10):1560–1566. https://doi.org/10.1016/j.jse.2015.03.018
Chalmers PN, Slikker W 3rd, Mall NA, Gupta AK, Rahman Z, Enriquez D, Nicholson GP (2014) Reverse total shoulder arthroplasty for acute proximal humeral fracture: comparison to open reduction-internal fixation and hemiarthroplasty. J Shoulder Elbow Surg 23(2):197–204. https://doi.org/10.1016/j.jse.2013.07.044
Zafra M, Uceda P, Flores M, Carpintero P (2014) Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. Bone Joint J 96-b(9):1239–1243. https://doi.org/10.1302/0301-620x.96b9.33157
Schliemann B, Theisen C, Kösters C, Raschke MJ, Weimann A (2017) Reverse total shoulder arthroplasty for type I fracture sequelae after internal fixation of proximal humerus fractures. Arch Orthop Trauma Surg 137(12):1677–1683. https://doi.org/10.1007/s00402-017-2789-5
Obert L, Saadnia R, Tournier C, Bonnevialle N, Saragaglia D, Sirveaux F (2016) Four-part fractures treated with a reversed total shoulder prosthesis: Prospective and retrospective multicenter study Results and complications. Orthop Traumatol Surg Res 102(3):279–285. https://doi.org/10.1016/j.otsr.2016.01.019
Stahl D, Fuente Gde L (2016) Reverse total shoulder arthroplasty for a 4-part proximal humerus fracture. J Orthop Trauma 30(Suppl 2):S9–s10. https://doi.org/10.1097/bot.0000000000000607
Garofalo R, Brody F, Castagna A, Ceccarelli E, Krishnan SG (2016) Reverse shoulder arthroplasty with glenoid bone grafting for anterior glenoid rim fracture associated with glenohumeral dislocation and proximal humerus fracture. Orthop Traumatol Surg Res 102(8):989–994. https://doi.org/10.1016/j.otsr.2016.09.009
Maassen NH (2019) Treatment of a 4-part proximal humeral fracture with a concomitant glenoid fracture in an elderly patient: a case report. J Bone Joint Surg Case Connect 9(1):e13. https://doi.org/10.2106/JBJS.CC.18.00237
Driscoll MD, Burns JP, Snyder SJ (2015) Arthroscopic transosseous bony bankart repair. Arthrosc Tech 4(1):e47–50. https://doi.org/10.1016/j.eats.2014.11.001
Taverna E, Guarrella V, Freehill MT, Garavaglia G (2017) Arthroscopic reduction with endobutton fixation for glenoid fracture. Joints 5(2):127–130. https://doi.org/10.1055/s-0037-1603675
Sano T, Matsuoka H, Nakayama K (2009) Arthroscopic treatment of an anterior glenoid fracture with a cannulated, headless screw and suture anchors: a case report. Knee Surg Sports Traumatol Arthrosc 17(5):539–541. https://doi.org/10.1007/s00167-009-0732-1
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jin-Chul Oh, Hyoung-Sik Kim, Gi-Hoon Lee, and Ho-Jung Kang declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Yonsei University Gangnam Severance Hospital, reference number 3-2019-0158) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the participant included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oh, JC., Kim, HS., Lee, GH. et al. Arthroscopic treatment of a one-fourth anteroinferior glenoid comminuted fracture-dislocation with concomitant three-part complex proximal humerus fracture in a middle-aged man: a case report. Arch Orthop Trauma Surg 140, 1901–1907 (2020). https://doi.org/10.1007/s00402-020-03402-w
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03402-w