Abstract
Introduction
Stress shielding may lead to aseptic loosening which is a common reason for implant failure. An established method to identify implants with risk of implant failure caused by aseptic loosening is to measure early migration of the stem with the “Ein Bild Roentgen Analyse” femoral component analysis (EBRA-FCA). Therefore, the aim of this study was to measure the migration of a cementless short stem prosthesis via EBRA-FCA to predict the future performance.
Materials and methods
A total collective of 71 patients were treated with a cementless short hip stem prosthesis. Indications for surgery were primary coxarthrosis, dysplasia coxarthrosis or femoral head necrosis. After surgery, the patients were followed-up immediately after 3, 6, 12, 24, 36, and 48 months and X-ray images for EBRA-FCA measurements were taken. Axial caudal migration as well as the varus/valgus tilting of the prosthesis was determined. Possible influencing factors like BMI, age, diagnosis, gender or Harris Hip Score (HHS) on the migration of the stem were assessed.
Results
HHS increased significantly direct postoperatively (p < 0.001). At the second follow-up the average caudal migration was 0.42 ± 0.52 mm (range: 0.00–2.85 mm) (p < 0.001). A total of 14 patients underwent a caudal migration greater than 1.5 mm until 48 months. The initial varus and valgus tilts within the first 3 months were significant (p < 0.001). No correlations between BMI, age, diagnosis, gender or HHS and the migration as well as the tilting of the cementless short hip stem prosthesis were found.
Conclusions
Although initial axial caudal migration as well as tilting tendencies in varus or valgus position can be detected, there is no marked migration of the examined prosthesis after the first 48 months. Likewise, no aseptic early loosening was detected throughout the study period, which indicates good osseointegration of the short stem prosthesis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoprosthetic joint replacement surgery is the most frequently performed surgery in orthopedics in many western European countries. Each year over 1,000,000 primary hip arthroplasties are performed worldwide [1]. Excellent surgery results, demographic processes, and a change in lifestyle habits with decreasing physical activity as well as several other factors have led to an increase of hip joint replacement surgeries in younger patients. Because of the increasing lifespan, for those patients it is more likely to need a revision surgery. Therefore, it is important that the implanted prosthesis is increasingly bone preserving to make the revision surgery easier [2] and to have a better outcome for the patient. Due to the replacement of the natural hip joint with an artificial one, the transmitted forces on the femur will change [3, 4]. This leads to remodeling of the bone structure which in endoprosthetics is described as stress shielding. In areas with an increased load initiation, the bone density increases whereas a reduction of the transmitted forces results in bone resorption and osteolysis. Stress shielding may lead to aseptic loosening [5] which is next to other factors or problems like stem undersizing, periprosthetic fracture or via falsa a common reason for implant failure [6,7,8,9,10,11]. Therefore, adequate physiological load initiation is essential to preserve the bone structure for good osseointegration, stable implants, and also for potential further surgeries. To achieve this, short stem total hip arthroplasty (THA) appears to be a promising method [2, 12] as it is less traumatic and preserves more bone structure than conventional hip arthroplasty. Likewise, short stem THA is soft tissue sparing [13] and leads to a more physiological load initiation [3, 14]. There is a variety of different short stem types available [15, 16]. To evaluate the long-term performance of the different stem types, long-term clinical studies are required. However, as most studies cover only the short-term to mid-term period [15], other methods to evaluate their performance are needed. An established method to identify implants with a high risk of implant failure caused by aseptic loosening is to measure early migration of the femoral component [13, 17]. A validated method among others is the “Ein Bild Roentgen Analyse” femoral component analysis (EBRA-FCA). Therefore, the aim of this study was to measure the migration of the Metha® short stem prosthesis via EBRA-FCA to predict the future performance. Furthermore, we exploratively identified the possible influencing factors like BMI, age, diagnosis, gender or Harris Hip Score (HHS) on the migration of the femoral component.
Patients and methods
Demographic data
Between November 2009 and June 2013, unilateral short stem hip arthroplasty was performed with the cementless monoblock Metha® short stem prosthesis on 89 patients by 1 experienced surgeon. A positive vote was received from the local ethics committee for this retrospective study (file number 229/13). Inclusion criteria were at least four X-ray images of the patients [8], one immediately postoperative X-ray image, and a minimum follow-up time of 24 months.
Radiological examination
After surgery, patients were followed-up immediately (t1), after 3 (t2), 6 (t3), 12 (t4), 24 (t5), 36 (t6), and 48 (t7) months. X-rays (pelvis anteroposterior view and Lauenstein image) were taken during the follow-ups. The X-rays which were used for the measurement with EBRA-FCA software (Institute for Mathematics and Geometry at the Faculty of Civil Engineering, University of Innsbruck in Austria) [18] were obtained individually and anonymously from the digital X-ray image archive.
Clinical examination
In addition to X-ray follow-ups, the Harris Hip Score (HHS) [19] was assessed preoperatively (t0) and at t1, t2, t3, and till follow-up t4.
EBRA-FCA measurements
EBRA-FCA uses a series of at least four digitized standard anterior–posterior X-rays [8]. The first X-ray serves as a reference value. A migration of 1.5 mm after 2 years is described as a predictive value for later aseptic loosening of the implant by the authors of EBRA-FCA [7]. Using this threshold, EBRA-FCA predicts revision for aseptic loosening with a sensitivity of 69%, a specificity of 80%, and an accuracy of 79% [7]. Compared to RSA, the software has a specificity of 100% and a sensitivity of 78% for the detection of migration of over 1 mm [20]. The EBRA software which has been modified for a short stem prosthesis [17] is used to determine the migration of the femoral component of a hip endoprosthesis over time using digital X-ray series. For this purpose, the axial caudal migration as well as the angle between femur and prosthesis stem axis (varus/valgus position) is determined on the stem. Defined prosthesis and bone reference points are being marked and the reference points of the first X-ray image at t1 are compared with the follow-up images. As reference points we selected the center of the prosthesis head, the intersection between the prosthesis axis and the shoulder point of the prosthesis, the intersection between the tangents around the trochanter minor and the intersection between the prosthesis axis, and the most prominent point of the trochanter major [20] (Fig. 1). The recordings deemed by the program to be non-comparable are automatically excluded [7]. It is possible to determine the accuracy of the comparability limit of the X-ray images to each other. For this purpose, the comparability limit may get a value between 1 and 4 mm. The lower the selected value is, the greater the measurement accuracy. However, this also increases the likelihood for images to be excluded. The software manufacturers recommend a limit of 3 mm [18, 20]. This value was also used in this study. With a confidence limit of 95%, the measurement accuracy for determination of the caudal migration is described as + 1.5 mm to − 1.2 mm [20]. For measurement of the stem angulation, the accuracy was ± 0.4° in the 95% confidence interval [21]. Evaluation of the measured reference points and distances is effected by means of the independent EBRA-FCA program.
Statistics
The Kolmogorov–Smirnov test was used to analyse the normal distribution of the data. Possible influencing factors such as BMI, age, diagnosis, gender or HHS on the migration behavior of the prosthesis as well as pairwise comparisons of the migration behavior depending on the follow-up examination were investigated using the Kruskal–Wallis test and the Mann–Whitney U test. A significance level of p < 0.05 was considered statistically significant. Each analysis was performed using the SPSS version 26.0 software (IBM Corporation, New York, USA).
Results
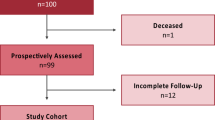
18 of the 89 patients were excluded due to the following problems: 8 had a follow-up time of less than 24 months, for 5 patients less than four X-rays were available and for another 5, the postoperative X-rays were not accepted by the software. This results in a total collective of 71 patients, 30 (42.2%) of these being female and 41 (57.8%) being male (Fig. 2). The mean age at the time of surgery was 56.8 ± 10.7 years (range: 27–78). The patients had a mean body mass index (BMI) of 27.6 ± 4.5 kg/m2 (range: 18–38). Indication for surgery was based on the diagnosis of primary coxarthrosis (n = 51; 72.0%), dysplasia coxarthrosis (n = 14; 20.0%) or femoral head necrosis (n = 6; 8.0%).
Clinical results
The HHS averaged 56.5 points (n = 71) at t0, 87.8 points (n = 71) at t1, 91.0 points (n = 63) at t2, 93.0 points (n = 63) at t3, and 92.0 points (n = 69) at t4. The change from t1 compared to t0 (p < 0.001) was highly significant.
Caudal migration of the Metha® short stem prosthesis
At the second follow-up after 3 months (t2, n = 63), the average caudal migration of the Metha® short stem prosthesis was 0.42 ± 0.52 mm (range 0.00–2.85 mm) (p < 0.001). The 6-month follow-up (t3, n = 63) showed a migration of 0.58 ± 0.76 mm (range 0.01–4.96 mm). After 12 months (t4; n = 69), the mean migration was 0.73 ± 0.99 mm (range 0.01–6.26 mm). After 24 months (t5; n = 63), the prosthetic stems showed an axial caudal migration of 1.01 ± 1.27 mm (range 0.05–8.23 mm). At the 36-month follow-up (t6; n = 54), there was a migration of 1.01 ± 1.27 mm (range 0.07–9.26 mm) and of 0.81 ± 0.64 mm (range 0.05–2.11 mm) after 48 months (t7; n = 22). A total of 12 patients underwent a caudal migration greater than 1.5 mm until the follow-up of 48 months—two already at 3 months (ID#22 and ID#42), three after 6 months (ID#12, ID#14 and ID#15), three more after 24 months (ID#16, ID#21 and ID#61), and four after 36 months (ID#39, ID#40, ID#43 and ID#69) (Table 1).
Tilting of the Metha® short stem prosthesis
Figure 3 shows the course of the valgus and varus tilts at the various follow-ups. After 3 months (t2) one patient (ID#68) of n = 63 patients showed increased valgization. The initial varus and valgus tilt within the first 3 months were statistically significant (p < 0.001). After 12 months (t4), one patient of n = 69 patients showed increased shift towards varus (ID#29) and one more patient with increased valgization (ID#54). After 24 months (t5), one more patient of n = 63 patients showed increased valgization (ID#28) and one more patient with increased varus (ID#50). At the 36-month follow-up (t6), there were six more of n = 54 patients with increased valgization ( ID#36, ID#37, ID#49, ID#63, and ID#66) and three more patients with increased varus (ID#44, ID#53, and ID#69). After 48 months (t7), there was a total of one of n = 22 patients with increased valgization (ID#12) and one patient with increased varus (ID#52) (Table 1). None of the follow-ups allowed establishing a correlation between BMI, age, diagnosis, gender or HHS, and the migration as well as the tilting of the Metha® short stem prosthesis.
Course of the valgus/varus change of the Metha® prosthesis within 48 months. An angle > 0° corresponds to a varus tilt, an angle < 0° to a valgus tilt. The black line marks the zero point, the red lines the limits > 5° or > − 5. Extreme values are shown as circles. *Asterisk indicates statistical significance of p < 0.001
Discussion
Short stem prostheses have been clinically proven for several years [10] as they reduce, among other things, the reactive bone remodeling process in the proximal femoral area [2, 12]. However, to be able to detect any aseptic loosening in the short stem endoprosthesis at an early stage and to be able to make any statements concerning successful treatment, EBRA can be used to detect axial stem migration as well as any valgus or varus tilting of the prosthesis [13, 17]. Therefore, within the scope of this study, the migration as well as the valgus or varus tilting of the Metha® short stem prosthesis was clinically and radiologically followed-up within the first 48 months by means of the EBRA-FCA method. Likewise, any other possible epidemiological influencing factors of the patients on the migration behavior of the prosthesis were taken into account.
We were able to show that the HHS significantly improved immediately after surgery at t1 compared to the preoperative recording at t0 and then continued to show very good clinical results until the last clinical follow-up t4 after 12 months. This result shows that the cohort had a good and pain-free quality of life after THA and throughout the 12-month clinical follow-up period. These findings are consistent with the previous studies that found continuously high HHS values for the entire cohort after the implantation of the Metha® short stem prosthesis throughout the follow-up period [22,23,24].
In a clinical study of the working group Kutzner et al., the influence of the valgus as well as varus stem position of a calcar guided short stem prosthesis was investigated with regard to periprosthetic bone density changes and axial caudal migration as well as tilting into valgus or varus position of the prosthesis. Using the EBRA method, it was found within a follow-up period of 2 years that the valgus stem position is accompanied by an increased initial migration of the prosthesis. However, the clinical outcome as well as the periprosthetic bone remodeling processes remained unaffected regardless of the position of the stem. In case of valgus stem position, the authors mention undersizing with insufficient fit and fill of the stem as the main cause of the axial caudal migration [25].
The philosophy of maximum fill thanks to maximized dimension of the short stem prostheses to achieve a good cortical fit and to maximize stress distribution over a wide range has been studied in detail in a previous study [11]. It could be shown that the entire cohort had a good fit and fill ratio (> 0.8) in the proximal area of the examined and maximally dimensioned Metha® short stem prosthesis and that the prosthesis thus could be wedged proximally and did not undergo excessive axial caudal migration in the entire collective. In addition, the authors were able to detect a connection between the preoperative femoral configuration and the axial caudal migration or tilting characteristics of the prosthesis. The “normal” as well as the “stovepipe” femoral configuration brought consistently good radiological results regarding fit and fill. Only the “champagne flute” femoral configuration occasionally caused high distal fit and fill ratio (> 0.8) and thus increased and, therefore, undesirable distal wedging of the implant. The authors came to the conclusion that the Metha® short stem prosthesis should, if possible, be implanted with maximum dimensions to achieve a locking of the implant as proximal as possible and thus proximal and physiological force application as far as possible. This recommendation particularly applied to the “champagne flute” femur configuration.
Regardless of the particular femoral configuration of the cohort of this study, the philosophy of maximized prosthesis size was applied throughout the collective to preclude in advance excessive prosthesis migration due to reduction of the primary stability caused by an undersized prosthesis [26]. Clinically, this could lead to early aseptic loosening and thus to a revision of the implant. Considering the results of our study, we notice that despite the maximized size of the prosthesis, there is nevertheless an incipient moderate, but significant axial caudal migration of the Metha® short stem prosthesis within the first 3 months. This could be explained by a reduced load initiation or a non-osseointegration of the implant in the proximal femur, which, therefore, would lead to an initial bone density reduction of the surrounding bone. In this case, an initial moderately axial migration of the prosthesis could occur until it has come to a secondary osteointegration of the implant. This decrease in bone density in the proximal femur directly after implantation of the Metha® prosthesis has also been demonstrated in the previously published studies [10, 27]. However, short stem prostheses show a generally more balanced bone remodeling behavior and thus a more physiological load transmission compared to straight stem prostheses [10, 28]. Nevertheless, in vivo long-term studies showing the advantages of short stem prostheses compared to straight stem prostheses have still to be carried out [29].
However, a progressive and excessive caudal migration of the Metha® short stem prosthesis does not occur during the follow-up period, so that there is indeed a certain “settling effect” and good osseointegration of the prosthesis. Axial caudal migration of the implant > 1.5 mm within the first 2 years is interpreted as a predictive value for possible early aseptic loosening of the implant [7]. In fact, individual patients of our collective were found to have caudal migration values > 1.5 mm within the first 24 months, which could ultimately lead to an increased risk of possible aseptic loosening of the implant. However, in our collective and within the 48-month follow-up period, no revision of a Metha® short stem prosthesis due to aseptic loosening nor any other reasons, like deep infection, dislocation or trauma had to be carried out. Thus we cannot confirm a generally valid correlation between initial caudal migration > 1.5 mm and early aseptic loosening.
Similar results can be demonstrated in the case of varus as well as valgus tilting of the Metha® short stem prosthesis. Initially, there is a significant incipient valgus as well as varus tilting of the prosthesis. However, an excessively progressive course cannot be demonstrated either, so that this tilting can also be interpreted as a “settling” of the prosthesis and it is possible that it only depends on the initial stem positioning within the femoral cortex.
Limitations
This study has some limitations. The RSA method definitely offers higher accuracy compared to the EBRA-FCA method. However, in contrast to the RSA method, the EBRA-FCA method is a less invasive procedure with sufficient specificity and accuracy to detect possible early loosening. Another limitation is the overlapping of the X-ray images, especially in the measurement of varus or valgus tilting. Due to different rotational positions of the femur during the radiological follow-ups, overlapping of the X-ray images may occur, which can then lead to measurement errors. However, to minimize this error as far as possible and to ensure a reproducible position, the patients were examined with the aid of a standardized X-ray record and using special positioning aids. Although this is a retrospective analysis, we do not see any study limitation here due to the fact that the X-ray examinations were each prospectively collected. In contrast, there is a limitation due to the failure of some subjects, due to the technical failure to use the images and the failure to follow-up. In view of the exact result evaluation and the continuous care of the patients, we consider the results to be nevertheless suitable and robust.
Conclusions
In general, no significant correlation between possible influencing factors such as BMI, age, diagnosis, gender or HHS, and a possible migration as well as the tilt of the Metha® short stem prosthesis could be demonstrated in this study. Although initial minor axial caudal migration as well as tilting tendencies in varus or valgus position of the Metha® short stem prosthesis can be detected within the collective, there is no marked migration of the Metha® prosthesis after the first 48 months. Likewise, no aseptic early loosening was detected throughout the study period, which indicates good osseointegration of the Metha® short stem prosthesis.
References
Pivec R, Johnson AJ, Mears SC, Mont MA (2012) Hip arthroplasty. Lancet 380:1768–1777. https://doi.org/10.1016/S0140-6736(12)60607-2
Wittenberg RH, Steffen R, Windhagen H, Bücking P, Wilcke A (2013) Five-year results of a cementless short-hip-stem prosthesis. Orthop Rev 5:e4. https://doi.org/10.4081/or.2013.e4
Gronewold J, Berner S, Olender G, Hurschler C, Windhagen H, von Lewinski G, Floerkemeier T (2014) Changes in strain patterns after implantation of a short stem with metaphyseal anchorage compared to a standard stem: an experimental study in synthetic bone. Orthop Rev 6:5211. https://doi.org/10.4081/or.2014.5211
Jahnke A, Fonseca Ulloa CA, Seeger JB, Rickert M, Jahnke GW, Ahmed GA, Ishaque BA (2018) Analysis of the elastic bending characteristics of cementless short hip stems considering the valgus alignment of the prosthetic stem. Clin Biomech 52:49–56. https://doi.org/10.1016/j.clinbiomech.2018.01.006
Roth A, Richartz G, Sander K, Sachse A, Fuhrmann R, Wagner A, Venbrocks R-A (2005) Verlauf der periprothetischen Knochendichte nach Hüfttotalendoprothesenimplantation. Abhängigkeit von Prothesentyp und knöcherner Ausgangssituation. Orthopade 34:334–344. https://doi.org/10.1007/s00132-005-0773-1
Streit MR, Haeussler D, Bruckner T, Proctor T, Innmann MM, Merle C et al (2016) Early migration predicts aseptic loosening of cementless femoral stems: a long-term study. Clin Orthop Relat Res 474:1697–1706. https://doi.org/10.1007/s11999-016-4857-5
Krismer M, Biedermann R, Stöckl B, Fischer M, Bauer R, Haid C (1999) The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J Bone Joint Surg Br 81:273–280
Kroell A, Beaulé P, Krismer M, Behensky H, Stoeckl B, Biedermann R (2009) Aseptic stem loosening in primary THA: migration analysis of cemented and cementless fixation. Int Orthop 33:1501–1505. https://doi.org/10.1007/s00264-008-0701-1
Ishaque BA, Stürz H, Basad E (2011) Fatigue fracture of a short stem hip replacement: a failure analysis with electron microscopy and review of the literature. J Arthroplasty 26:665.e17–20. https://doi.org/10.1016/j.arth.2010.05.021
Yan SG, Weber P, Steinbrück A, Hua X, Jansson V, Schmidutz F (2018) Periprosthetic bone remodelling of short-stem total hip arthroplasty: a systematic review. Int Orthop. 42:2077–2086. https://doi.org/10.1007/s00264-017-3691-z
Jahnke A, Engl S, Seeger JB, Basad E, Rickert M, Ishaque BA (2015) Influences of fit and fill following hip arthroplasty using a cementless short-stem prosthesis. Arch Orthop Trauma Surg 135:1609–1614. https://doi.org/10.1007/s00402-015-2302-y
von Lewinski G, Floerkemeier T (2015) 10-year experience with short stem total hip arthroplasty. Orthopedics 38:S51–S56. https://doi.org/10.3928/01477447-20150215-57
Kutzner KP, Kovacevic MP, Freitag T, Fuchs A, Reichel H, Bieger R (2016) Influence of patient-related characteristics on early migration in calcar-guided short-stem total hip arthroplasty: a 2-year migration analysis using EBRA-FCA. J Orthop Surg Res 11:29. https://doi.org/10.1186/s13018-016-0363-4
Kaipel M, Grabowiecki P, Sinz K, Farr S, Sinz G (2015) Migration characteristics and early clinical results of the NANOS® short-stem hip arthroplasty. Wien Klin Wochenschr 127:375–378. https://doi.org/10.1007/s00508-015-0756-0
van Oldenrijk J, Molleman J, Klaver M, Poolman RW, Haverkamp D (2014) Revision rate after short-stem total hip arthroplasty: a systematic review of 49 studies. Acta Orthop 85:250–258. https://doi.org/10.3109/17453674.2014.908343
Loppini M, Grappiolo G (2018) Uncemented short stems in primary total hip arthroplasty: the state of the art. EFORT Open Rev 3:149–159. https://doi.org/10.1302/2058-5241.3.170052
Schmidutz F, Graf T, Mazoochian F, Fottner A, Bauer-Melnyk A, Jansson V (2012) Migration analysis of a metaphyseal anchored short-stem hip prosthesis. Acta Orthop 83:360–365. https://doi.org/10.3109/17453674.2012.712891
Krismer M, Tschupik JP, Bauer R, Mayrhofer P, Stöckl B, Fischer M, Biedermann R (1997) Einzel-Bild-Röntgen-Analyse (EBRA) zur Messung der Migration von Hüftendoprothesen. Orthopade 26:229–236. https://doi.org/10.1007/PL00003378
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Biedermann R, Krismer M, Stöckl B, Mayrhofer P, Ornstein E, Franzén H (1999) Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Röntgen-Analyse-femoral component analysis. J Bone Joint Surg Br 81:266–272
Wilkinson JM, Hamer AJ, Elson RA, Stockley I, Eastell R (2002) Precision of EBRA-Digital software for monitoring implant migration after total hip arthroplasty. J Arthroplasty 17:910–916
Augustin L, Boller S, Bobach C, Jahnke A, Ahmed GA, Rickert M, Ishaque BA (2018) Development of periprosthetic bone mass density around the cementless Metha® short hip stem during three year follow up—a prospective radiological and clinical study. Int Orthop 62:579. https://doi.org/10.1007/s00264-018-4126-1
Boller S, Jahnke A, Augustin L, Ahmed G, Rickert M, Ishaque BA (2018) Age-related osseointegration of a short hip stem: a clinical and radiological 24 months follow-up. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-018-3082-y
Jahnke A, Engl S, Altmeyer C, Jakubowitz E, Seeger JB, Rickert M, Ishaque BA (2014) Changes of periprosthetic bone density after a cementless short hip stem: a clinical and radiological analysis. Int Orthop 38:2045–2050. https://doi.org/10.1007/s00264-014-2370-6
Kutzner KP, Freitag T, Donner S, Kovacevic MP, Bieger R (2017) Outcome of extensive varus and valgus stem alignment in short-stem THA: clinical and radiological analysis using EBRA-FCA. Arch Orthop Trauma Surg 137:431–439. https://doi.org/10.1007/s00402-017-2640-z
Fottner A, Woiczinski M, Kistler M, Schröder C, Schmidutz TF, Jansson V, Schmidutz F (2017) Influence of undersized cementless hip stems on primary stability and strain distribution. Arch Orthop Trauma Surg. 137:1435–1441. https://doi.org/10.1007/s00402-017-2784-x
Lerch M, von der Haar-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM (2012) Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop. 2012(36):533–538. https://doi.org/10.1007/s00264-011-1361-0
Epinette J-A, Brax M, Chammaï Y (2017) A predictive radiological analysis of short stems versus both shortened and long stems in primary hip replacement: a case-control study of 100 cases of Metha versus ABG II and Omnifit HA at 2–8 years’ follow-up. Orthop Traumatol Surg Res. 103:981–986. https://doi.org/10.1016/j.otsr.2017.07.014
Schnurr C, Loucif A, Patzer T, Schellen B, Beckmann J, Eysel P (2018) Short stem survival after osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 138:573–579. https://doi.org/10.1007/s00402-018-2892-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We thank Aesculap for the financial support for the EBRA software costs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jahnke, A., Wiesmair, AK., Fonseca Ulloa, C.A. et al. Outcome of short- to medium-term migration analysis of a cementless short stem total hip arthroplasty using EBRA-FCA: a radiological and clinical study. Arch Orthop Trauma Surg 140, 247–253 (2020). https://doi.org/10.1007/s00402-019-03315-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03315-3