Abstract
Background
Patients with developmental dysplasia of the hip (DDH) require special surgical considerations for total hip arthroplasty (THA). Despite the difficulties posed by the population’s anatomical abnormalities, few large evaluations of postoperative outcomes exist. This study seeks to characterize outcomes following primary THA among patients diagnosed with DDH.
Methods
A retrospective review was conducted at a tertiary care center on all THA patients between June 2011 and March 2018. Inclusion criteria for this study included any patient diagnosed with DDH undergoing primary THA. Baseline information, operative reports, and postoperative outcomes were pulled from the medical record.
Results
In total, 336 patients (385 hips) undergoing a THA between June 2011 and March 2018 were included. The average age was 52.6 ± 13.0 years and body mass index was 27.8 ± 6.0 kg/m2. Most patients were female (82%). The majority of hips (89%, n = 344) were Crowe type 1, followed by 2 (6.9%, n = 26), 3 (2.6%, n = 10), and 4 (1.3%, n = 5). Most hips were Hartofilakidis Class A (83%, n = 320), followed by Class B (15%, n = 59), then C (1.6%, n = 6). Mean follow-up was 24.8 months. Revision THA was required in 19 (4.9%) cases, with the most common indications being infection (2.1%) and periprosthetic fracture (1.0%). Readmission rates were 1.8% (7 hips) and 2.9% (11 hips) at 30-day and 90-day, respectively. The 30-day and 90-day ED visit rates were 1.3% (5 hips) and 2.1% (8 hips), respectively. No complications were seen following 344 (87%) THAs.
Conclusion
Despite their surgical complexity, DDH patients on average have notably low rates of revision and dislocation. Longer follow-up is needed to better assess outcomes after THA in this complex patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) encompasses a spectrum of abnormalities involving the developing hip, ranging from a located hip with dysplastic features to subluxation or irreducible dislocation [1]. Though dysplastic cases noted in infancy may be successfully treated with splints, such patients must be followed up with regular radiographs to detect the need for surgical management since enduring dysplasia will lead to degenerative joint disease in adulthood [2]. Radiographic evidence of dysplasia has been reported in 50–100% cases of hip osteoarthritis in patients under 60 years of age requiring total hip arthroplasty (THA) [3,4,5]. Malformations of the hip increases the mechanical load across the hip joint, resulting in non-physiologic compensatory mechanisms by the surrounding soft-tissues; indeed, such wear and tear of encompassing structures are detectable by ultrasound technology in symptomatic DDH patients [6].
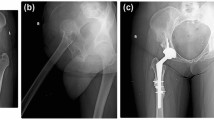
Preoperative planning for THA in patients with DDH requires special consideration of each individual’s unique anatomic abnormalities. Reconstructive decisions can be guided through the use of classification systems which categorize hips based on the degree of dysplasia and extent of anatomic deformities [7, 8]. The two most commonly used are the Crowe and Hartofilakidis classification systems. The one devised by Crowe and Ranawat et al. divides hips into four categories based on the percent subluxation of the femoral head from the acetabulum, calculated as the ratio of the distance between the inter-teardrop line and head–neck junction to the vertical height of the pelvis [7]. The classification system by Hartofilakidis et al. broadly divides hips into categories of dysplasia (A), indicating a femoral head located within the acetabulum despite some subluxation, low dislocation with the presence of a false acetabulum superior to the true acetabulum (B), and high dislocation (C), in which the femoral head is completely uncovered by the true acetabulum and positioned superiorly and posteriorly [9].
Studies have previously reported poorer implant survival rates following THA in patients with hip dysplasia than in the general population, partly explained by technical difficulties related to complex bone morphologies and negative prognostic factors such as young age [10, 11]. Commonly reported complications include aseptic loosening, postoperative dislocations, polyethylene wear, intraoperative femoral fractures, nerve injury, and nonunion of the femoral osteotomy [10, 12, 13]. However, implant survival rates, complication rates, and revision rates vary widely between studies, likely due to modest sample sizes and the tendency to focus on specific dysplasia classifications, implant type, and surgical techniques. The purpose of this study is to characterize outcomes following primary THA in a large cohort of patients diagnosed with DDH. Our hypothesis is that, on average, this group of DDH patients will demonstrate similar rates of complications, readmission and reoperation as those reported in the literature for primary THA done for any other etiology. However, we also hypothesize that hips with a higher severity dysplasia according to Crowe and Hartofilakidis classifications will be associated with higher complication, readmission, and reoperation rates than hips of lower severity despite presenting with similar comorbidity scores.
Methods
This study was conducted in accordance with our university Institutional Review Board. A query of all THA surgeries performed at a tertiary urban academic center between June 2011 and March 2018 was performed using Epic Caboodle version 15 (Verona, WI). Cases of developmental/congenital hip dysplasia were then identified with Microsoft SQL Server Management Studios 2017 (Redmond, WA) using a Boolean search of patients’ past medical history containing the following combination of phrases: DDH OR (Dysp* AND HIP) OR (Deform* AND HIP) OR (Congenital AND HIP).
A review of the electronic medical record was used to pull baseline demographic information, operative reports, and postoperative outcomes. Hip dysplasia was graded by two trained observers (L.S. and J.G.) based on preoperative radiographs according to both the Crowe and Hartofilakidis classifications. Both observers agreed on the same criteria prior to grading, and together graded the first ten set of randomly chosen radiographs to promote consistency. Both reviewers also independently reviewed a set of 30 randomly chosen radiographs in order to calculate interrater correlation. Additionally, for patients who reported a previous history of hip osteotomy, one surgeon (J.V.) reviewed the preoperative radiographs to classify the osteotomy as pelvic, femoral, or both.
All patients underwent a standardized preoperative and postoperative clinical pathway for their care episode that encompassed pain management and physical therapy [14]. Progressive weight bearing status was decided by the individual surgeon on a case-to-case basis.
For analysis, hips were grouped by severity, with Group A consisting of Crowe type 1, Group B of Crowe types 2–4, Group X of Hartofilakidis class A, and Group Y of Hartofilakidis classes B, C. These distinctions were chosen to ensure that higher severity groups (Groups B and Y) would not contain too low of a population for analyses. Range of motion scores at the preoperative and follow-up visits were noted if recorded.
Emergency department (ED) visits within 30 and 90 days as well as any hospital readmissions within the same intervals were noted. These intervals were chosen because of their relevance to payers’ bundled reimbursement models. Information was obtained for patients from the preoperative planning visit through the most recent visit and/or until the date of reoperation for a complication related to the initial surgery.
Failure endpoints were defined as surgical-related failures, which included any complication related to the implant such as dislocation (with or without subsequent reoperation), infection, aseptic loosening, and periprosthetic fracture. The endpoint used was the date that the patient initially presented with symptoms of the complication.
Statistical analysis
All statistical analyses were conducted with Stata statistical software (StataCorp). Kappa values were used to assess interobserver agreement. Differences in outcomes between Groups A and B as well as Groups X and Y were calculated using Fisher’s exact test. Differences in comorbidity scores and surgical times recorded between groups were assessed using t tests ANOVA. Simple regression using log-transformed surgical times as a predictor variable was used to assess the correlation between follow-up complications and length of surgery. Hazard ratios were also conducted to assess the impact of group classifications on survival of implants.
Results
The search of patient problem lists and surgical procedure names as described in the methods produced a list of 17,000 patients. After narrowing down the list through a search of past medical histories, 389 hips belonging to 340 patients were identified. Upon review of the medical record, three hips belonging to three patients were found to not have had a primary THA done (one hemiarthroplasty for femoral neck fracture, one conversion THA secondary to hemiarthroplasty for motor vehicle collision, and one periacetabular osteotomy). Another hip was found to have had a primary THA but for primary osteoarthritis. Thus, our sample included 385 hips belonging to 336 patients. Of these THAs, 7 patients (14 hips; 3.6%) had simultaneous bilateral THAs, 198 (44.9%) were performed on the right hip, and 173 (51.4%) were performed on the left hip. Notably, 42 patients underwent staged surgeries for the left and right hip.
Surgeries were performed by a total of 26 surgeons, with each surgeon operating on an average of just under 15 hips. At the time of surgery, the average age was 52.6 years and body mass index (BMI) was 27.8 kg/m2. The majority of patients were female (82%). Mean Charlson comorbidity index (CCI) and Elixhauser Comorbidity scores were 2.4 and − 0.64, respectively. Further information on demographics and co-morbidities information can be found in Tables 1 and 2.
The majority of hips (89%, n = 344) were Crowe–Ranawat Group 1, followed by Group 2 (6.9%, n = 26), Group 3 (2.6%, n = 10), and Group 4 (1.3%, n = 5). Hartofilakidis classifications were: A (83%, n = 320), followed by Class B (15%, n = 59), then C (1.6%, n = 6). Kappa values for interobserver agreement were 0.79 for Crowe classification and 0.76 for Hartofilakidis scores.
In total, 24 hips had undergone an osteotomy prior to surgery. Of these, 15 were performed when the patient was 8 years old or younger. The age at the first surgery for the 9 other patients ranged from 9 to 36 years. Based on a review of preoperative radiographs, 16 of the osteotomies were determined to be femoral, 6 were classified as pelvic, and 2 were classified as both.
Of the THAs, only six cases (1.6%) required concomitant osteotomies intraoperatively. Most of these cases (1.3%; n = 5) involved subtrochanteric shortening and one case (0.3%) involved a segmental osteotomy to correct for an existing excessive leg length discrepancy.
Intraoperative complications were seen in 22 cases (5.7%). The most common complication seen was femoral fractures (n = 11, 2.9%), followed by blood loss requiring transfusion (n = 2, 0.5%), and dislocation (n = 2, 0.5%). Inpatient complications were seen in 12.2% of patients (47 hips). The most common reasons for inpatient complications were related to postoperative hypotension, hyponatremia, and urinary retention (9 hips each). Other cases involved pulmonary embolism (4 hips) and/or hypoventilation, thrombocytopenia, bradycardia, acute kidney injury, hyperkalemia, and fever (1 instance of each). Some cases involved a combination of the complications listed. Transfusion of at least one unit of packed red blood cells was required in 42 cases (10.9%) during the hospitalization. One patient was found to have migration of the acetabular component on radiograph taken during the hospitalization on postoperative day 5, for which the patient underwent revision surgery. No serious inpatient complications resulting in death or permanent injury occurred.
Mean follow-up was 24.8 months. A total of 19 cases (4.9%) required revision THA, with the most common indication being infection (n = 8, 2.1%). Other indications for revision included periprosthetic fracture (n = 4, 1.0%), instability (n = 3, 0.78%), aseptic loosening (n = 3, 0.78%), and painful protrusion of hardware (n = 1, 0.3%). The average time of revision surgery was 61.7 weeks after the primary operation, with a range of 0.6–285.7 weeks. The case with the minimum time of 4 days to revision notably was a case of periprosthetic fracture that occurred during the patient’s hospitalization for the initial surgery. The post-discharge course was free of complications following 344 (87%) THAs. The 30-day and 90-day readmission rates were 1.8% (7 hips) and 2.9% (11 hips), respectively. The 30-day and 90-day ED visit rates were 1.3% (5 hips) and 2.1% (8 hips), respectively.
No significant difference was found in CCI or Elixhauser scores between Groups A (n = 344) and B (n = 41) (2.5 vs. 2.3, p = 0.411; 3.0 vs. 3.0, p = 0.466, respectively). Similarly, Groups X (n = 320) and Y (n = 65) reported statistically similar CCI and Elixhauser scores (2.5 vs. 2.4, p = 0.898; − 0.67 vs. − 0.50, p = 0.681, respectively). Group A had similar rates of previous osteotomies to Group B (4.8% vs 4.6%, p = 0.99), as did Group X and Group Y (4.8% vs. 4.7%, p = 0.99). Additionally, the proportion of those with a history of a previous osteotomy did not differ between those patients who developed surgical complications and those who did not (4.3% vs 4.9%, p = 0.99).
No statistically significant difference in intraoperative complication rates was seen in neither Groups A and B (4.2% vs. 11.6%, p = 0.053) nor Groups X and Y (4.15% vs. 9.52%, p = 0.107). Regarding inpatient complications, no difference was seen between Groups A and B or between Groups X and Y (37.4% vs 51.4%, p = 0.11 and 38.5% vs. 42.5%, p = 0.63, respectively).
The lower severity Groups (A and X) reported faster operative times both by Crowe (Δ40 min, p < 0.0001) and Hartofilakidis classifications (Δ24 min, p = 0.0025). The majority (88.9%) of patients in Group B experienced surgical times of great than 90 min, whereas the minority underwent surgeries lasting less than 60 min (11.1%). Within Group Y, the majority received surgeries longer than 90 min (58.6%), while the others experienced surgical times of between 60 and 90 min (31.0%) or below 60 min (10.3%). Length of surgical time in Group Y had no correlation with the likelihood of experiencing a follow-up complication; however, in Group B, longer surgical times were moderately associated with a lower risk of follow-up complication (p = 0.03).
Concerning survival, Group Y was found to have a hazard ratio of 3.017 when compared to Group X with p = 0.013 (95% CI: 1.26, 7.20). This was similar to the significant difference between Groups X and Y’s rates of surgical-related failure seen on Fisher’s exact test (4.6% vs. 13.3%, p = 0.017).
Group B was not found to have an increased hazard ratio for surgical failure compared to Group A (95% CI: 0.62, 5.39). On Fisher’s exact test, a non-significant difference was seen in the number of surgical-related failures between Groups A and B (5.6% vs 9.5%; p = 0.303).
A history of previous osteotomy made no difference in rates of follow-up complications experienced by Groups A and B, nor by Groups X and Y (p = 0.99 for both). Similarly, the presence of an osteotomy done concomitantly during the THA proved not to make a significant difference in the complication rates experienced by Groups A and B and Groups X and Y (p = 0.99).
Regarding reoperation rates, no difference was seen between either Groups A and B (5.6% vs. 4.7%, p = 0.99) or between Groups X and Y (4.6% vs 9.8%, p = 0.12).
Groups A and B reported statistically similar hospital readmission rates at both 30 and 90 days (1.9% vs. 0%, p = 0.99; 3.0% vs 2.7%, p = 0.39). Similarly, there was no difference between the groups in 30- and 90-day ED visit rates (1.3% vs. 2.4%, p = 0.46; 2.0% vs. 5.1%, p = 0.313). Groups X and Y mirrored these results in 30- and 90-day readmission rates (1.7% vs. 1.7%, p = 0.99; 2.8% vs. 3.6%, p = 0.511), as well as in 30- and 90-day ED visit rates (1.3% vs. 1.7%, p = 0.59; 2.1% vs. 3.6%, p = 0.418).
At final follow-up, there was one death unrelated to the THA that took place 53 months post-surgery.
Discussion
This study of 385 hips presents the largest THA outcomes study of developmentally dysplastic hips in the United States. At a mean follow-up time of 24.8 months, no postoperative complication was seen for the majority of hips (87%, n = 344), and revisions were required for only 4.9% (n = 19). Despite the complicated preoperative planning required for dysplastic hips, the complication rate were similar to lifetime risk of revision THA surgery for patients with osteoarthritis [15]. 30-day and 90-day readmission and ED visits were also low. These results are in line with a large database study using the Norwegian Arthroplasty Register, which found that after adjusting for patient variables, risk of revision in DDH patients is the same as in patients undergoing routine THA for idiopathic osteoarthritis, regardless of dislocation status [16].
Few other studies have compared outcomes across the spectrum of Crowe and Hartofilakidis classifications. When stratified by Crowe types, the more severe group in our study was found to have longer surgical times, suggesting more complicated surgeries; however, no statistically significant increase in hazard ratio for surgical-related failure was seen between groups. Furthermore, there were no differences in reoperation rates or readmission and ED visit rates at both 30 and 90 days. Though more severely dysplastic hips may pose more surgical difficulties, our results indicate that with proper treatment and management there was no greater risk of complications with this patient population. Interestingly, when divided by Hartofilakidis classification, a slightly significantly higher rate of surgical-related failures was seen in the higher severity group. However, no difference in intraoperative complications, reoperation rates, readmissions, and ED visits at both 30 and 90 days were seen between groups. This cannot be attributed to differences in comorbidities, as the comorbidity scores were not significantly different between groups.
Reported outcomes have historically been good in patients with mild or moderate dysplasia, but may vary in patients with more severe dysplasia. Cameron et al. reported that postoperative Harris hip scores of patients without DDH were similar to those of Crowe 1 patients, but significantly lower than those of Crowe 2–4 patients [17]. Crowe 4 patients also had significantly more complications than patients with lower Crowe grades. They concluded that Crowe grade is an important prognostic factor with respect to the number of postoperative complications. Mackenzie et al. found that Crowe 3 patients had the highest rates of loosening compared to Crowe 2 and Crowe 4 patients, although the sample size was small and the differences did not reach significance [18]. Numair et al. reported that in a cohort of Crowe 1, 2, and 3 patients, 83% had normal/nearly normal function and 82% had full/nearly full range of motion, as compared to 54% and 72%, respectively, for Crowe 4 patients [19]. Furthermore, they found that 15% of Crowe 4 hips had to be revised for loosening of the acetabular cup, as opposed to only 9% of the Crowe 1–3 hips, citing difficulties in achieving fixation in higher degrees of dislocation. High rates of loosening in these studies were attributed to the use of cement in acetabular reconstruction, and uncemented components are now the standard of care [10, 11, 18,19,20,21].
Our results also indicate that a previous history of osteotomy did not impact the rates of surgical-related failures seen. While osteotomies have been shown to delay the need for THA in dysplastic hips, such reconstructions may leave a residual angular deformity which could increase the technical skill required for a successful THA [22]. However, some argue that prior osteotomies may facilitate later implant fixation [23]. Chougle et al. correlated a significantly worse survival of the acetabular component after a previous Chiari osteotomy or shelf procedure [24]. However, conflicting evidence reported prior osteotomy as having no effect on the survivorship of THA in DDH patients, so further outcomes studies are needed [25].
Limitations to this study include underpowered analyses for severity group comparisons as well as limited follow-up time. There may exist inconsistencies in the grading of hips since two reviewers were used to evaluate preoperative radiographs. However, the high interrater reliability scores for the Crowe and Hartofilakidis grades indicated a substantial degree of interrater agreement for both types of classification. Also, these findings only apply to hips operated at this single U.S. institution. Surgical experience at other institutions may differ and thus our results are not generalizable to the entire DDH population. Finally, due to the retrospective and single-center nature of the study, it cannot be concluded that all complications that occurred were treated at our center and thus captured by the data.
Conclusions
Orthopedic surgeons face a number of challenges when operating on the dysplastic hip, emphasizing the importance of preoperative planning for each individual’s unique bony morphology. Despite the surgical complexities involved, in this largest U.S. single institution study of THAs undergone by DDH patients the average revision rate is low and comparable to primary THA for other diagnoses.
References
Kotlarsky P, Haber R, Bialik V, Eidelman M (2015) Developmental dysplasia of the hip: what has changed in the last 20 years? World J Orthop 6:886–901. https://doi.org/10.5312/wjo.v6.i11.886
Kubo H, Pilge H, Nepp K, Westhoff B, Krauspe R (2018) Development of unstable hips after treatment with the Tubingen splint: mid-term follow-up of 83 hip joints. Arch Orthop Trauma Surg 138:629–634. https://doi.org/10.1007/s00402-018-2882-4
Clohisy JC, Dobson MA, Robison JF, Warth LC, Zheng J, Liu SS, Yehyawi TM, Callaghan JJ (2011) Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Jt Surg 93:3–9. https://doi.org/10.2106/JBJS.J.01734
Weinsten SL, Mubarak SJ, Wenger DR, Developmental hip dysplasia and dislocation: part I. J Bone Jt Surg. 85 (2003)
Karimi D, Kallemose T, Troelsen A, Klit J (2018) Hip malformation is a very common finding in young patients scheduled for total hip arthroplasty. Arch Orthop Trauma Surg 138:581–589. https://doi.org/10.1007/s00402-018-2900-6
Jacobsen JS, Bolvig L, Holmich P, Thorborg K, Jakobsen SS, Soballe K, Mechlenburg I (2018) Muscle-tendon-related abnormalities detected by ultrasonography are common in symptomatic hip dysplasia. Arch Orthop Trauma Surg 138:1059–1067. https://doi.org/10.1007/s00402-018-2947-4
Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Jt Surg 61:15–23
Hartofilakidis G, Stamos K, Ioannidis TT (1988) Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br 70:182–186
Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N (1996) Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Jt Surg 78:683–692
Greber EM, Pelt CE, Gililland JM, Anderson MB, Erickson JA, Peters CL (2017) Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J Arthroplasty 32:S38–S44. https://doi.org/10.1016/j.arth.2017.02.024
Sanchez-Sotelo J, Berry DJ, Trousdale RT, Cabanela ME (2002) Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. J Am Acad Orthop Surg 10:334–344. https://doi.org/10.5435/00124635-200209000-00005
Wang D, Li L-L, Wang H-Y, Pei F-X, Zhou Z-K (2017) Long-term results of cementless total hip arthroplasty with subtrochanteric shortening osteotomy in crowe type IV developmental dysplasia. J Arthroplasty 32:1211–1219. https://doi.org/10.1016/J.ARTH.2016.11.005
Zeng W-N, Liu J-L, Wang F-Y, Zhang X, Fan H-Q, Chen G-X, Guo L, Duan X-J, Zhou Q, Yang L (2017) Total hip arthroplasty for patients with Crowe type IV developmental dysplasia of the hip: Ten years results. Int J Surg 42:17–21. https://doi.org/10.1016/J.IJSU.2017.04.029
Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD (2016) Early results of medicare’s bundled Payment initiative for a 90-day total joint arthroplasty episode of care. J Arthroplasty 31:343–350. https://doi.org/10.1016/j.arth.2015.09.004
Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, Cooper C, Carr AJ, Arden NK, Beard DJ, Price AJ, The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study., Lancet (London, England). 389 (2017) 1424–1430. https://doi.org/10.1016/S0140-6736(17)30059-4
Engesæter LB, Furnes O, Havelin LI (2008) Developmental dysplasia of the hip—good results of later total hip arthroplasty. J Arthroplasty 23:235–240. https://doi.org/10.1016/J.ARTH.2007.03.023
Cameron HU, Botsford DJ, Park YS (1996) Influence of the Crowe rating on the outcome of total hip arthroplasty in congenital hip dysplasia. J Arthroplasty 11:582–587
MacKenzie JR, Kelley SS, Johnston RC (1996) Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip. Long-term results. J Bone Joint Surg Am 78:55–61
Numair J, Joshi aB, Murphy JC, Porter ML, Hardinge K (1997) Total hip arthroplasty for congenital dysplasia or dislocation of the hip. Survivorship analysis and long-term results. J Bone Jt Surg 79:1352–1360
Sochart DH, Porter ML (1997) The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Jt Surg 79:1599–1617
Yang S, Cui Q (2012) Total hip arthroplasty in developmental dysplasia of the hip: Review of anatomy, techniques and outcomes. World J Orthop 3:42–48. https://doi.org/10.5312/wjo.v3.i5.42
Yuasa T, Maezawa K, Kaneko K, Nozawa M (2017) Rotational acetabular osteotomy for acetabular dysplasia and osteoarthritis: a mean follow-up of 20 years. Arch Orthop Trauma Surg 137:465–469. https://doi.org/10.1007/s00402-017-2636-8
Lack W, Windhager R, Kutschera HP, Engel A (1991) Chiari pelvic osteotomy for osteoarthritis secondary to hip dysplasia. Indications and long-term results. J Bone Joint Surg Br 73:229–234
Chougle A, Hemmady MV, Hodgkinson JP (2006) Long-term survival of the acetabular component after total hip arthroplasty with cement in patients with developmental dysplasia of the hip. J Bone Joint Surg Am 88:71–79. https://doi.org/10.2106/JBJS.D.02689
Migaud H, Putman S, Berton C, Lefevre C, Huten D, Argenson J-N, Gaucher F (2014) Does prior conservative surgery affect survivorship and functional outcome in total hip arthroplasty for congenital dislocation of the hip? A case-control study in 159 hips. Orthop Traumatol Surg Res 100:733–737. https://doi.org/10.1016/j.otsr.2014.07.016
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seo, L.J., Gabor, J., Novikov, D. et al. Outcomes in 385 developmental dysplastic hips requiring total hip arthroplasty. Arch Orthop Trauma Surg 139, 723–728 (2019). https://doi.org/10.1007/s00402-019-03143-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03143-5