Abstract
Introduction
Reverse shoulder arthroplasty shifts the rotational center of the shoulder joint caudally and medially to restore shoulder function in a rotator cuff deficient shoulder. Despite promising results in early- and mid-term follow-up, long-term loss in shoulder function has been described in the literature. A lack of exercise in elderly patients may be one reason for this loss in function. This study examines the functional benefits of physical therapy in the mid-term to long-term follow-up regarding the subjective and objective shoulder function.
Materials and methods
Twenty patients with a mean age of 73 years were included in this series. The study was performed as a single-center, prospective study. Initial indications for reverse shoulder arthroplasty were cuff tear arthropathy, failed anatomical shoulder arthroplasty, and fracture sequelae. The patients were clinically examined at a mean follow-up of 62 months using the Constant score (CS) and the DASH score for the operated and the non-operated shoulder. They were reevaluated using the same scores following a standardized physical therapy program of 6 weeks’ duration.
Results
The mean CS as well as the mean age- and gender-adjusted CS of the affected shoulder improved significantly from 53.5 points to 59.3 points, and 72.7–80.8%, respectively. The subcategories activities of daily living and range of motion of the CS improved significantly, whereas no significant improvement was observed for the subcategories pain and strength. Evaluating the contralateral shoulder, no significant change was observed for the age- and gender-adjusted CS and the CS as well as its subcategories. We found no significant difference in the CS comparing the different etiologies prior to physical therapy.
Discussion
Physical therapy plays an important role subsequent to reverse shoulder arthroplasty. It also has an effect in the mid-term to long-term follow-up regarding the range of motion as well as activities of daily living. However, physical therapy seems to have limited effect on the strength and the residual pain level.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1987 Paul Grammont designed the reverse Delta III prosthesis [1, 2], which has been modified over the years and is nowadays used for a variety of indications.
The primary indication for reverse shoulder arthroplasty is a massive, non-reparable defect of the rotator cuff with secondary arthritis of the glenohumeral joint (cuff tear arthropathy) [3,4,5,6] and an accompanying pseudoparalysis of the affected shoulder. Other indications that can be treated by implantation of a reverse shoulder prosthesis are loss of shoulder function due to secondary rotator cuff tears after anatomical shoulder arthroplasty [7, 8], failed treatment of humeral head fractures (fracture sequelae) [9,10,11], and even failed treatment of the primary implantation in cases of humeral head fractures [12, 13] with accompanying insufficiency or tears of the rotator cuff or decreased quality of the fractured tuberosities.
The biomechanical principle is a shift of the rotational center medially and the distalisation of the humerus leading to increased deltoid tension and lever arms. Due to these changes, the deltoid muscle is partially able to provide functional replacement of the rotator cuff muscles due to an increase in the deltoid moment arm and the muscular pretension [14, 15].
However, despite promising results in the early- and mid-term, a loss of function has been described for the long-term follow-up [3, 14, 16]. Therefore, other conservative and surgical treatment options should be considered prior to the implantation of a reverse shoulder prosthesis. Especially the indication for reverse shoulder arthroplasty in patients under the age of 60 years is considered closely.
The loss of shoulder function [3, 16] may be due to degenerative changes of the deltoid muscle, thus being irreversible. However, another factor might be the lack of exercise in elderly patients. A rehabilitation program following total shoulder arthroplasty is essential [17,18,19,20,21,22], but there is insufficient data regarding physical therapy in the mid-term to long-term follow-up following reverse shoulder arthroplasty.
With this regard, the present study examines the functional benefits of physical therapy in the mid-term to long-term follow-up regarding the subjective and objective shoulder function.
Materials and methods
Patients
Twenty patients (6 male, 14 female) with an average age of 73 years (range 58–84 years) at the time of examination were included in this series. The study was performed as a single-center, prospective study.
The patients were divided into three groups based on the underlying etiology for which they were treated. Group 1 consisted of nine patients (45%) suffering from cuff tear arthropathy, group 2 had four patients (20%) with revision after failed anatomical arthroplasty, and group 3 had seven patients (35%) suffering from fracture sequelae.
All patients received a reverse shoulder arthroplasty by means of implantation of a Delta III shoulder prosthesis or a Delta XTend shoulder prosthesis (DePuy International Ltd., Leeds, England).
Follow-up
The patients were examined at an average follow-up of 62 months (median 89 months, range 41–157 months) after implantation of the reverse shoulder prosthesis. The subjective outcome was evaluated using the DASH score [23] comprising questions about performing activities of daily living. The objective functional outcome of the operated shoulder as well as the contralateral side were assessed using the Constant score (CS) [24] comprising the four subsections range of motion (ROM), activities of daily living (ADL), pain, and strength. The age- and gender-adjusted Constant score [25] was additionally calculated. The strength subsection of the Constant score was measured with the arm abducted 90° in the scapular plane (IsoForceControl, MDS AG, Oberburg, Switzerland) and was scored as zero if the patient could not reach this position.
Subsequent to the examination, all patients took part in a standardized 6-week rehabilitation program including equipment-based training therapy, manual therapy, heat therapy, massage therapy, and electrotherapy. The goal was the strengthening of the glenohumeral and scapular stabilizing musculature, pain reduction, and improvement of the range of motion.
After completion of the physical therapy program the patients were reevaluated, again using the identical scores to assess the objective and subjective outcome.
The statistical evaluation was performed using SPSS software, vers. 21 (SPSS Inc., Chicago, Illinois) using the Wilcoxon signed-rank test and the Mann–Whitney U test.
Results
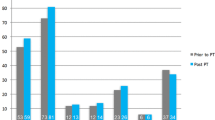
The mean Constant score improved significantly from 53.5 pts. (range 21–81 pts.) to 59.3 pts. (range 28–82 pts.; p = .014). The age- and gender-adjusted CS improved significantly from 72.7% (range 28–116%) to 80.8% (range 41–115%; p = .017) after rehabilitation (see Fig. 1).
For the contralateral shoulder a mean CS of 79.3 pts. (range 25–100 pts.) was reached prior to physical therapy and 79.6 pts. (range 42–92 pts.) after physical therapy (p = .87). The age- and gender-adjusted CS was 108.1% (range 88–137%) and 108.8% (range 61–133%) before and after the treatment, respectively (p = .79).
Concerning the subcategories of the CS for the affected shoulder, we noted a significant increase for the categories ADL from an average of 12.4 pts. to 14.3 pts. (p = .013) and ROM from 23.0 pts. to 26.2 pts. (p = .046). Statistically not significant were the results for the subcategories pain with an increase from 11.9 pts. to 13.1 pts. (p = .115) and strength with 6.2 pts. before and 6.0 pts. after physical therapy (p = .623).
The analysis of the subcategories of the CS for the contralateral side showed no significant difference before and after physical therapy (p > .05).
Comparing the results for different etiologies showed no significant difference in the functional values prior to physical therapy (p > .05). Following the rehabilitation program we observed a statistically significant difference for the age- and gender-adjusted CS with inferior results for the arthroplasty after fracture sequelae compared to cuff tear arthroplasty (p = .04) and revision after failed anatomical shoulder arthroplasty (p = .01).
We could not show a significant change in the subjective assessment of this trial. The DASH score improved from 37.1 pts. before physical therapy to 34.3 pts. after physical therapy (p = .12).
Discussion
Reverse shoulder arthroplasty is an important treatment option for patients suffering from cuff tear arthropathy as well as patients in need of surgical revision due to failed anatomical shoulder arthroplasty or fracture sequelae leading to good functional results [3, 4, 26, 27].
The mean Constant score of 53.5 pts. observed in this series with a mean follow-up of 62 months is comparable to the results published in the current literature. Sirveaux et al. [3] observed a mean CS of 65.5 pts. in a series of 80 patients with a mean follow-up of 44 months. In a study published in 2006 by Boileau et al. [9] the observed mean CS of 45 patients was 58 pts. at a follow-up of 40 months and in 2011 Cazeneuve et al. [28] published a series of 35 patients with a mean follow-up of 86 months and a mean CS of 53 points.
The glenohumeral joint biomechanics in shoulders with insufficiency of the rotator cuff is altered due to a loss of the centering forces of the rotator cuff, leading to a cranial migration of the humeral head [29]. In this situation, reverse shoulder arthroplasty is able to increase active abduction and forward flexion on the one hand and to decrease pain on the other [14].
The evaluation of the shoulder joint kinematics after RSA showed decreased glenohumeral motion but increased scapulothoracic motion during elevation [30, 31], suggesting an emphasized role of the periscapular musculature in postoperative rehabilitation. Another key point in postoperative physical therapy seems to be the strengthening of the deltoid and upper trapezius muscles, since these are the primary abductors of the shoulder [32,33,34,35]. The posterior deltoid fibers also play an important role in external rotation [36, 37].
Although rehabilitation programs for the postoperative treatment of reverse shoulder arthroplasty have been described [38], there is still a lack of consensus and data on the effectiveness of physical therapy in the mid-term to long-term follow-up.
A decrease in shoulder function in the mid-term to long-term follow-up, especially in range of motion, can be partially reversed by a standardized physical therapy program after reverse shoulder arthroplasty. This is confirmed by an increase in the ADL and ROM subcategories of the CS observed in this series. However, the physical therapy seems to have no effect on the residual pain level and the strength of the affected shoulder, which is reflected in the absence of significant changes in the other two CS subcategories as well as in the subjective DASH score.
Furthermore, a possible bias/placebo effect must be taken into consideration as generated by the attention of the physical therapist to the patient. However, this effect seems not to contort the present results as interpreted from the lack of improvement in the subjective subcategory pain of the CS as well as the lack of improvement in the subjective DASH score.
The average patient receiving a reverse shoulder arthroplasty is an elderly patient. The mean age in our series was 73 years at the time of examination. An improvement in shoulder function after physical therapy may be due to a lack of physical activity in this group of patients. However, we did not observe an improvement in the non-operated shoulder.
Determining to what extent this improvement of the shoulder function applies for the long-term follow-up and whether a repetition of the physical therapy is able to prevent a decrease in shoulder function has to be a purpose of future trials.
Limitations of this series are the small sample size with the subsequent small groups when dividing patients according to the underlying etiology, which is a bias and may lead to distortion of the results. The reason for the small sample size is the average age of the examined population. The recruitment was performed by phone. Owed to the age of the study population, some patients had died before reaching the minimum follow-up, others where simply satisfied with their shoulder function and not interested in performing physical therapy or visiting our outpatient department.
Another limitation of this series is the missing compare group to perform a matched-pair analysis. This is due to the reasons mentioned before. We were not able to recruit enough patients to generate a second, non-treatment group, mainly due to the inclusion criteria and the age of the patients.
The contralateral shoulder is a poor control, because it differs from the normal age- and gender-matched control shoulder due to the fact that the cuff tear arthropathy is often bilateral. However, in this series we observed an age- and gender-adjusted CS of 108% before and 109% after physical therapy for the contralateral shoulder, suggesting a normal, age-appropriate shoulder function.
For further research, a prospective, matched-pair analysis would be preferable. However, this study type was not selected for our analysis, due to the relatively small patient cohort with an implant survival time of more than 4 years due to the advanced age of the patients.
Conclusion
Physical therapy can help to improve certain objective and subjective aspects of the shoulder function in the mid-term to long-term follow-up after reverse shoulder arthroplasty. This applies to the range of motion and the use of the affected shoulder for activities of daily living, but it seems to have no effect on the residual pain level or on the strength of the affected shoulder.
The main limitation of this series is the missing control group for a matched-pair analysis, which is mainly due to the advanced age of the patients and the inclusion criteria.
References
Grammont P, Trouillod P, Laffay JP, Deries X (1987) Etude et réalisation d’une nouvelle prothèse d’épaule. Rheumatologie 39:407–418
Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16:65–68
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Jt Surg Br 86:388–395
Naveed MA, Kitson J, Bunker TD (2011) The Delta III reverse shoulder replacement for cuff tear arthropathy: a single-centre study of 50 consecutive procedures. J Bone Jt Surg Br 93:57–61. https://doi.org/10.1302/0301-620X.93B1.24218
Cuff D (2008) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Jt Surg 90:1244. https://doi.org/10.2106/JBJS.G.00775
Werner CML, Steinmann PA, Gilbart M, Gerber C (2005) Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Jt Surg Am 87:1476–1486. https://doi.org/10.2106/JBJS.D.02342
Flury MP, Frey P, Goldhahn J, Schwyzer H-K, Simmen BR (2011) Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure—midterm results. Int Orthop 35:53–60. https://doi.org/10.1007/s00264-010-0990-z
Levy JC, Virani N, Pupello D, Frankle M (2007) Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Jt Surg Br 89–B:189–195. https://doi.org/10.1302/0301-620X.89B2.18161
Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elb Surg 15:527–540. https://doi.org/10.1016/j.jse.2006.01.003
Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PAW (2008) Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 22:698–704. https://doi.org/10.1097/BOT.0b013e31818afe40
Kontakis G, Tosounidis T, Galanakis I, Megas P (2008) Prosthetic replacement for proximal humeral fractures. Injury 39:1345–1358. https://doi.org/10.1016/j.injury.2008.09.003
Merschin D, Stangl R (2015) Proximale Humerusfraktur im fortgeschrittenen Lebensalter. Unfallchirurg. https://doi.org/10.1007/s00113-015-0009-8
Kaisidis A, Pantos PG, Heger H, Bochlos D, Selimas S, Oikonomoulas V (2014) Reverse shoulder arthroplasty for the treatment of three and four part fractures of the proximal humerus in patients older than 75 years old. Acta Orthop Belg 80:99–105
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elb Surg 14:147S–161S. https://doi.org/10.1016/j.jse.2004.10.006
Terrier A, Reist A, Merlini F, Farron A (2008) Simulated joint and muscle forces in reversed and anatomic shoulder prostheses. J Bone Jt Surg Br 90–B:751–756. https://doi.org/10.1302/0301-620X.90B6.19708
Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G (2006) Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Jt Surg Am 88:1742–1747. https://doi.org/10.2106/JBJS.E.00851
Brems JJ (1994) Rehabilitation following total shoulder arthroplasty. Clin Orthop Relat Res 307:70–85
Brown DD, Friedman RJ (1998) Postoperative rehabilitation following total shoulder arthroplasty. Orthop Clin N Am 29:535–547
Pokorný D, Sosna A, Jahoda D, Pech J, Simková M, Szekeresová M (2000) Physical therapy after shoulder arthroplasty. Acta Chir Orthop Traumatol Cech 67:280–290
Boardman ND, Cofield RH, Bengtson KA, Little R, Jones MC, Rowland CM (2001) Rehabilitation after total shoulder arthroplasty. J Arthroplast 16:483–486. https://doi.org/10.1054/arth.2001.23623
Wilcox RB, Arslanian LE, Millett P (2005) Rehabilitation following total shoulder arthroplasty. J Orthop Sport Phys Ther 35:821–836
Mulieri PJ, Holcomb JO, Dunning P, Pliner M, Bogle RK, Pupello D, Frankle MA (2010) Is a formal physical therapy program necessary after total shoulder arthroplasty for osteoarthritis? J Shoulder Elb Surg 19:570–579. https://doi.org/10.1016/j.jse.2009.07.012
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29:602–608. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR (2005) Normalization of the Constant score. J Shoulder Elb Surg 14:279–285. https://doi.org/10.1016/j.jse.2004.10.009
Baulot E, Chabernaud D, Grammont PM (1995) Results of Grammont’s inverted prosthesis in omarthritis associated with major cuff destruction. Apropos of 16 cases. Acta Orthop Belg 61(Suppl 1):112–119
Mulieri P, Dunning P, Klein S, Pupello D, Frankle M (2010) Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Jt Surg Am 92:2544–2556. https://doi.org/10.2106/JBJS.I.00912
Cazeneuve JF, Cristofari DJ (2011) Long term functional outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res 97:583–589. https://doi.org/10.1016/j.otsr.2011.03.025
Neer CS, Craig EV, Fukuda H (1983) Cuff-tear arthropathy. J Bone Jt Surg Am 65:1232–1244
de Toledo JM, Loss JF, Janssen TW, van der Scheer JW, Alta TD, Willems WJ, Veeger DH (2012) Kinematic evaluation of patients with total and reverse shoulder arthroplasty during rehabilitation exercises with different loads. Clin Biomech (Bristol Avon). https://doi.org/10.1016/j.clinbiomech.2012.04.009
Walker D, Matsuki K, Struk AM, Wright TW, Banks SA (2015) Scapulohumeral rhythm in shoulders with reverse shoulder arthroplasty. J Shoulder Elb Surg 24:1129–1134. https://doi.org/10.1016/j.jse.2014.11.043
Walker D, Wright TW, Banks S, Struk AM (2014) Electromyographic analysis of reverse total shoulder arthroplasties. J Shoulder Elb Surg 23:166–172. https://doi.org/10.1016/j.jse.2013.05.005
Ekstrom RA, Donatelli RA, Soderberg GL (2003) Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther 33:247–258. https://doi.org/10.2519/jospt.2003.33.5.247
Ekstrom RA, Soderberg GL, Donatelli RA (2005) Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol 15:418–428. https://doi.org/10.1016/j.jelekin.2004.09.006
Farina D, Madeleine P, Graven-Nielsen T, Merletti R, Arendt-Nielsen L (2002) Standardising surface electromyogram recordings for assessment of activity and fatigue in the human upper trapezius muscle. Eur J Appl Physiol 86:469–478. https://doi.org/10.1007/s00421-001-0574-0
Phadke V, Camargo P, Ludewig P (2009) Scapular and rotator cuff muscle activity during arm elevation: a review of normal function and alterations with shoulder impingement. Braz J Phys Ther 13:1–9. https://doi.org/10.1590/S1413-35552009005000012
Reinold MM, Wilk KE, Fleisig GS, Zheng N, Barrentine SW, Chmielewski T, Cody RC, Jameson GG, Andrews JR (2004) Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sport Phys Ther 34:385–394. https://doi.org/10.2519/jospt.2004.34.7.385
Boudreau S, Boudreau ED, Higgins LD, Wilcox RB (2007) Rehabilitation following reverse total shoulder arthroplasty. J Orthop Sports Phys Ther 37:734–743. https://doi.org/10.2519/jospt.2007.2562
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
All authors were involved in treating and evaluating the patients. SU and SG were involved in data analysis and writing of the paper. SH and SP were involved in prove reading of the manuscript. All authors have reviewed and agree with the contents of the final draft of this article as submitted.
Corresponding author
Ethics declarations
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Stephan Uschok, Sebastian Herrmann, Stephan Pauly, Carsten Perka and Stefan Greiner declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Uschok, S., Herrmann, S., Pauly, S. et al. Reverse shoulder arthroplasty: the role of physical therapy on the clinical outcome in the mid-term to long-term follow-up. Arch Orthop Trauma Surg 138, 1347–1352 (2018). https://doi.org/10.1007/s00402-018-2977-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2977-y