Abstract
Introduction
Tibial tubercle osteotomy (TTO) is a well-established extensile approach to improve joint visualization and implant removal. Despite this, TTO is a challenging technique with a long learning curve and potential pitfalls. Complications are not infrequent, even if performing the correct surgical steps. Aim of this paper is to review the current literature about TTO, its safeness and reliability, and finally the complications rate.
Materials and methods
We performed a systematic review of the available English literature, considering the outcomes and the complications of TTO. The combinations of keyword were “tibial tubercle osteotomy”, “total knee arthroplasty”, “total knee revision”, “outcomes”, “complication” and “surgical approach”.
Results
From the starting 322 papers available, 26 manuscripts were finally included. Most of the papers show significant improvements in clinical outcomes, both in primary and in revision procedures. Radiographic fragment healing is close to 100%. Related complications can range from 3.8–20%.
Conclusion
TTO may be necessary to correct pathological tuberosity position or patella tracking. However, TTO is a challenging technique to improve the surgical approach during total knee arthroplasty. A strict surgical technique can lead to better results and to minimize complications. However, it is not clear if the improved outcome can outweigh the longer surgery and the higher risk of pitfalls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays total knee arthroplasty (TKA) is one of the most widely performed procedures in orthopedics practice, proving remarkably successful in providing pain relief and restoring joint function. Consequently, the requirement for revision total knee arthroplasty (RTKA) in the United States was projected to grow by 601% between 2005 and 2030 [1]. In addition, the rate of re-revisions is also expected to increase, with some studies showing a current figure in the range of 8–18% [2]. The results after primary knee arthroplasty are reasonably predictable and reproducible.
Revision knee arthroplasty is usually associated with worse results than after primary arthroplasty [3]. There are many causes of failure of a TKA and the need for revision. Determining the cause of failure is essential when planning a revision procedure, since this will determine which components require extraction and replacement; which surgical approach should be performed; whether the procedure can be performed as a one-stage or two-stage procedure; which type of implant should be used; and how the patient can be informed about the expected outcome [3]. Moreover, having a diagnosis before starting a revision is crucial. Revisions performed for undiagnosed pain have worse results [4].
Lombardi et al. [5] found aseptic loosening was the major reason of revision in terms of frequency (31.2%), followed by instability (18.7%), infection (16.2%), polyethylene wear (10.0%), arthrofibrosis (6.9%) and misalignment (6.6%). Other probable causes are osteolysis, patella-femoral or extensor mechanism problems and peri-prosthetic fracture. Regardless of the cause of failure, the key to the success of revision TKA is a safe surgical approach using an exposure that minimizes complications, allowing a correct management of soft tissues. Exposure of the knee may be difficult in RTKA. Common problems associated with repeat revisions are loss of bone stock, progressive scarring, deficits of the extensor mechanism, and stiffness. Therefore, technique modifications that focus on preservation of bone stock, maintenance of the extensor mechanism, and enhanced early mobilization bear importance are widely used. The underlying problem is frequently due to fibrous retraction of the patellar tendon, or the extensor mechanism. This makes eversion of the patella difficult and forced eversion may result in patellar ligament rupture, which may have profound consequences. Although, in most patients, a medial parapatellar approach (MPA) with complete synovectomy is sufficient, various surgical approaches can be used in these tricky situations, but occasionally, severe complications have been reported, mainly related to the loss of complete extension of the knee, due to the caused tissue fibrosis, or with vascular compromise of the patella, triggering a secondary necrosis. If additional exposure is needed, a quadriceps snip (QS) performed through the quadriceps tendon often provides the additional exposure required. The usefulness of this kind of approach is that it is simple and does not modify the postoperative rehabilitative protocol. Due to the risk of postoperative extensor lag, a V-Y quadricepsplasty is rarely indicated. In rare cases, in which additional exposure is needed in stiff knee or patella baja, or when removal of a cemented long-stemmed tibial component is required, a tibial tubercle osteotomy (TTO) may be used. Since TTO was first described by Dolin in the 1980s [6], it has widely become one of the exposures of choice for revision surgery; because of its low complications rate, it is useful in explantation and implantation, secure and protect the extensor mechanism, lower tourniquet time, and do not interfere with postoperative mobilization and weight bearing. Moreover, TTO has shown excellent clinical outcomes in a variety of patellofemoral problems. In general, TTO may be considered in cases of an excessive lateral position of the tuberosity (TT-TG > 20 mm) or patellar height abnormality (Caton-Deschamps index > 1.2) in patients with patellofemoral instability or to decrease stress at the patellofemoral joint in patients being treated for large focal defects of the patella or trochlea [7]. TTO represents a reliable option in this scenario, which includes several alternatives such as tuberosity anteriorization, distalization and anteromedialization [8].
However, TTO is not free from complications, such as problems with pain in the anterior side of the knee due to the impact of the osteosynthesis material, proximal migration of the anterior tibial tuberosity (ATT), fracture-avulsion of the ATT, fracture of the ATT, fracture of the tibial shaft, or loss of extensor mechanism function [9]. The TTO is typically 7–10 cm in length, with the coronal osteotomy made from the medial side [10, 11]. Proximally, the thickness should be approximately 1 cm, tapering distally to approximately 5 mm. This is performed with a small oscillating saw, which is also used to make a transverse cut at the distal aspect of the osteotomy. The proximal transverse cut is made parallel to the joint line with a small osteotome. Ideally, a proximal bony bridge is maintained to prevent migration of the tubercle during healing. Next, two large osteotomes are used to elevate the fragment of the tubercle, while maintaining the soft-tissue envelope laterally. The patella can then be everted and the knee flexed to complete the procedure. Finally, the knee is extended and the displaced fragment of tubercle is brought back to its anatomical location [12]. Several fixation methods of the ATT have been described, such as the synthesis with cerclage wire or screws, or the use of different sutures [13]. The aim of this paper is to evaluate the efficacy and safety of TTO as a useful surgical approach in difficult total knee arthroplasty, especially during revision surgery.
Materials and methods
We performed a systematic review of the available English literature to answer to two main research questions:
-
How TTO could improve clinical outcomes of TKA procedure?
-
What is the safety and rate of complications of tibial tuberosity osteotomy?
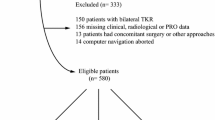
The Pubmed, Embase, Medline, Medscape, Google Scholar and Cochrane library databases were screened for relevant studies. The search strategy consisted of a combination of the following keywords: tibial tubercle osteotomy, total knee arthroplasty, total knee revision, outcomes, complications, and surgical approach. We included clinical studies with a follow-up greater than 12 months and with a cohort of patients greater than 10. Non-pertinent manuscripts were excluded. Exclusion criteria were in vitro studies, case report, expert opinion and review or meta-analysis. We carefully examined reference lists from previous reviews or meta-analysis not to miss pertinent papers. The search was limited to studies published in English. Two reviewers (S.B. and S.D.) independently screened the titles and abstracts from all identified articles to assess their appropriateness to the research focus. In case of conflict among reviewers, a collegial evaluation with remaining authors was performed. References from the identified articles were checked not to miss any relevant articles. Every titles and abstracts that met our keywords were examined. The flow diagram illustrates the review process (Fig. 1).
Results
A total of 322 articles were identified, 137 duplicates were removed. Among 44 eligible articles, we selected only whose responding to our inclusion criteria. During papers’ selection, no cases of conflict between two authors were reported. 26 manuscripts were finally included and fully evaluated. Table 1 summarizes clinical and radiographic outcomes and rate of complications after TTO in TKA. (Table 1).
How TTO could improve clinical outcomes of TKA procedure?
Most of papers show an improvement of all clinical parameters evaluated, as Range of Motion (ROM), Visual Analog Score (VAS) and several clinical evaluation scales. These achievements seem to be independent if patients underwent to a primary or revision surgery and regardless of which is the cause of the revision. Langen et al. enrolled 580 patients for a primary TKA and categorized them into three groups: control group undergoing MPA, neutral TTO group and valgus TTO group (valgus > 10°). They reported a significant improvement in terms of ROM, clinical and functional scores at 1 year postoperatively. Moreover, no significant differences were found among groups over time, neither in leg alignment at the end of follow-up. The classic medial parapatellar approach frequently used in TKA proved to be sometimes insufficient in difficult cases such as rheumatoid arthritis (RA) [14]. Eid et al. [15] reported twenty-three knees in 20 patients with end-stage arthritis and knee stiffness due to RA. TTO was performed as a step of surgical procedure, displaying a meaningful improvement of clinical scores. As said before, there are many technique modifications useful when an additional exposure is needed. Among these, quadriceps snip (QS) and TTO approaches are commonly used for complicated revision TKA [16]. Sun et al. [17] enrolled 58 patients undergoing a second-stage RTKA for infected TKA using one of these two surgical approaches. ROM and most clinical and functional parameters improved significantly in both the groups at final follow-up. There was a significant improvement in The Knee Society Score (KSS), Hospital for Special Surgery score (HSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores and maximum flexion compared to the preoperative status in both groups and they were comparable between the two groups. Moreover, the femorotibial alignment and patellar height also showed no differences between the two groups. These two procedures proved to be efficient as surgical approach in revision surgery. This is not the only paper where these techniques are compared. Bruni et al. [18] followed 81 patients with chronic prosthetic knee infections who were randomized to receive a TTO or QS for exposure at the time of reimplantation. Patients in the TTO group had a higher mean KSS and maximum knee flexion with a lower incidence of extension lag than the QS group. Lateral parapatellar approach (LPA) is rarely indicated but is useful in the severe valgus knee deformities where MPA could be insufficient. It promises direct exposure and release of the contracted lateral soft tissues and straightforward correction of the patellar mal-tracking. Chalidis et al. [19] studied 53 consecutive patients who had non-correctable grade II valgus deformity (> 10°) undergoing a primary TKA via LPA with a TTO over a 10-year period. Mean knee flexion, extension, clinical and functional scores improved significantly. Furthermore, the tibiofemoral angle changed from a preoperative median value of 11° (10–17) to a postoperative value of 3.75° (0–9) with a leg alignment restoration. Congruent patellar tracking was observed in all cases. The results of this study support the use of LPA with TTO during TKA for non-correctable valgus knee osteoarthritis (OA). The rationale is that knees with a valgus deformity need for a lateral retinacular release because the Q angle is higher than usual and the patella is frequently subluxed laterally. The release of lateral retinaculum is incorporated in the lateral approach and proper patella tracking can be effectively achieved. These findings were validated by Apostolopoulos [20]. Nikolopoulos et al. [21] compared MPA and LPA with a TTO for non-correctable valgus knee osteoarthritis OA. Although they did not find significant differences in terms of VAS, maximum flexion and functional scores, the two techniques appear to differ significantly in the degree of the deformity in the anatomical axis alignment, with the TTO Group patients suffering a significantly smaller degree of deformity. The author concluded that even though both techniques could provide excellent results, the use of a LPA combined with TTO may be highly beneficial in moderate to severe valgus deformities. Piedade et al. [22] divided their patients into two groups. In group A, primary TKAs were performed with a classic MPA without a tibial tubercle osteotomy, while in group B, patients underwent TKAs with LPA along TTO to improve surgical exposure. The decision to perform TTO was determined preoperatively during the clinical and radiological examinations. In this series, a lateral or anterolateral approach was routinely performed in cases of valgus knee to assist with ligament balancing. In 48% of these valgus knees, TTO was carried out, first, to obtain an adequate medial plateau exposure and to evert the patella and when limited ROM was identified preoperatively. Postoperative clinical outcomes demonstrate that there is no significant difference in terms of pain, ROM, International Knee Society score (IKS) and degree of knee malalignment correction whether TTO was used. However, it should be emphasized that patient selection and proper technical procedure have a significant role in postoperative results. Similarly Hay et al. [23] compared MPA and lateral subvastus approach (LSA) with TTO in 32 patients undergoing primary TKA. Mean knee flexion, VAS, ROM and clinical scores improve significantly but there was no difference between two groups. The difference in the incidence of patellar subluxation at 2 years was statistically significant. Finally, it would seem to be more appropriate to reserve this technique for patients with problems of patellar tracking. However, TTO could also facilitate the anteromedial approach in a stiff joint and allows modification of the patellar position by acting on the distal side of the extensor system. As reported by Tabutin et al. [24], this technique could be suitable both in primary and revision surgery. They examinated 20 patients and divided them into two groups. The author shows a significant improvement in clinical and functional scores in both groups, with a greater gain in the patellar index and clinical capacities in the primary arthroplasty subgroup. Nevertheless, as said before, TTO is mainly useful as further exposure in revision surgery. Chinzei et al. [25] compared two groups of patients undergoing, respectively, primary and revision TKA. TTO was performed in complicated primary TKA, that is, severe fixed valgus deformity of the knee, rheumatoid arthritis and problems of patella tracking. The reasons for revision TKA included infection and aseptic loosening. Overall knee flexion and extension, ROM and functional scores improved significantly. The most interesting finding is that clinical outcomes improved in both groups, but postoperative ROM is significatively better than before surgery only in revision one. TTO seems to be effective for revision surgery regardless the reason of reintervention itself. Punwar et al. [26] performed forty-two for single-stage revisions and two-stage infected revisions. Clinical scores improved significantly in both groups. Certainly, functional outcomes were better in single-stage group and especially patients with TTOs fixed at a second stage were slower to recover function compared with those in the single stage. However, this paper shows, as remarkable finding, how in two-stage revisions, sequential osteotomies do not decrease union rates. The osteotomy is usually performed through the anterior metaphyseal cancellous bone of the tibia but it can be extended into the intramedullary canal if tibial stem and cement removal are necessary. Furthermore, repeat osteotomy may be required in another RTKA. Chalidis et al. [27] assessed whether intramedullary extension of TTO or repeat osteotomy affected the healing rate in RTKA. Bone healing occurred in all the cases. The median healing time for the extramedullary osteotomy group was 12 weeks and for the intramedullary osteotomy group it was 21 weeks. Repeat osteotomy was not associated with delayed union. Reliable bone healing can be expected with intramedullary extension or repeat TTO in RTKA. However, intramedullary extension of the osteotomy prolongs the union time of the tibial tubercle.
What is the safety and rate of complications of tibial tuberosity osteotomy (TTO)?
Exposure in TKA, and especially in revision surgery, can be challenging. Protection of the distal extensor mechanism is vital to maintain good knee function. This is at risk with excessive release or retraction of the patellar tendon. Sun et al. [17] compared the results of revision total knee arthroplasty between TTO and QS approaches for infected TKA. They found patellar tendon partial avulsion was more commonly observed in the QS group than in the TTO group (five vs two cases). On the other hand, no cases of complication related directly to the osteotomy were seen in the TTO group. They did not observe any proximal migration, tibial plateau or shaft fracture during the follow-up. Bruni et al. [18] compared the same two techniques. The author observed no differences in the reinfection rate between the two groups at last follow-up and no patient had rupture of the extensor mechanism. Therefore, TTO increased in popularity and has been used for several years in difficult primary and revision arthroplasty where the patella cannot be retracted at 90° of knee flexion. Even though TTO improves exposure protecting extensor mechanism, this technique is burdened by some related complications. First, it is crucial to analyze tuberosity’s rate of union since tubercle avulsion and its proximal migration are the most common TTO-related complications. Skimming literature, rates of union seem to be quite superposable and comforting. Choi et al. [28] observed radiographic union in 46/51 TTOs (90.2%), Le Moulec et al. [29] in 59/63 (93.7%), Mendes et al. [30] in 64/67 (95.5%), Young et al. [31] in 41/42 (97.6%) and Zonnenberg et al. [32] found union was achieved in 22/22 TTOs (100%). Furthermore, these papers show comparable results in term of osteotomy’s time of union too, ranging from 11 to 17 weeks. Abbas et al. [33] performed 181 TTOs in 159 patients; the osteotomies were reduced to preoperative positions in 161 knees (89%). In 20 knees (11%), which was affected by significant preoperative patella baja and/or stiffness of the soft tissue envelope, proximal reduction, mean 14.2 mm, was surgically effected to obtain the correct length and tension of the extensor mechanism. However, this leads to flexion loss. Of the 181 TTOs, 23 (13%) were repeat osteotomies performed in 21 patients who required a further one or two re-revision knee arthroplasties. Radiographic union occurred in all osteotomies (100%), with an average duration of 11 weeks (range 6–20 weeks). No extensor mechanism failure or complications related to the suture material occurred. The number of patients who have had a previous RTKA with TTO and require another RTKA is constantly increasing. In these patients, a new osteotomy at the same bone area may be necessary. Chalidis et al. [27] evaluated 74 consecutive patients who underwent 87 TTOs during RTKA. Among these, 12 patients had repeat TTOs. The osteotomy was extramedullary in 57 knees and intramedullary in 30 knees. Bone healing occurred in all cases. The median union time for the first TTO was 15 weeks and for the repeat TTO was 21 weeks. The median healing time in extramedullary group was 12 weeks while in intramedullary group was 21 weeks. Avulsion of the proximal part of the tibial tubercle occurred in three knees and superior migration of the entire osteotomized fragment was noted in two knees. They found repeat osteotomy was successful without increasing the time to union or the incidence of tibial tubercle migration. They also assessed that intramedullary extension of the bone cut is associated with an increase in the union time. However, the good healing capacity of TTO indicates that it can be safely extended into the intramedullary canal to allow access for cement and tibial stem removal. When patella eversion is difficult, TTO can be useful in primary surgery too. Piedade et al. [22] retrospectively analyzed 1474 TKAs where TTO is performed in 126 cases. The decision to perform TTO was determined preoperatively during the clinical and radiological examinations, underlying the importance of a correct indication. They found some intraoperative complications related to the osteotomy, as tibial plateau fissures and tibial tubercle fractures, significatively more frequent in TTO group. They also assessed a higher rate of postoperative complications in TTO group but, among these, only skin necrosis was considerably more frequent. Consequently, the author could conclude, although TTO is necessary under certain clinical conditions, it cannot be considered entirely safe in primary TKA. However, patients affected by RA with advanced joint destruction, poor bone quality and knee stiffness, or patients with severely deformed valgus knees could need a further extension of surgical approach. Some recent papers [15, 20] demonstrated TTO is highly beneficial under specific indications and this technique could be considered a routine step improving clinical outcomes. However, it is not clear if the improved outcome can outweigh the longer surgical time and higher risk of early complications and revisions [34].
Discussion
The demand for total knee arthroplasty is growing rapidly because of the proven success of this procedure and an increase in the aging population. Consequently, the requirement for revision total knee arthroplasty is projected to grow. The success of a TKA depends on several factors ranging from patient-related factors, operative techniques, to postoperative rehabilitation. The surgical exposure, as part of the operative technique, is an important contributor to successful outcome. However, to this day, there is no agreement with respect to the surgical exposure of choice in difficult primary TKA and revision TKA [16, 17, 30, 35,36,37,38,39]. Patient-specific anatomies, such as strong valgus deformity of the knee, knee stiffness, poor bone stock, autoimmune conditions, concomitant diseases, are some aspects to be evaluated when considering the best surgical approach for TKA. Indeed, when poor bone quality is combined with knee stiffness, the functional range of motion after TKA may be compromised. In this case, the risk of patellar tendon detachment from its tibial insertion increases, even combined with patellar tendon’s fibrous retraction. To avoid it, different techniques have been used, and the extensor mechanism could be released distally at the tibial tubercle or proximally at the quadriceps tendon [15]. Among these techniques, TTO achieved satisfactory results during last decades, acting on the distal part of the extensor system to improve exposure, when scared tissue removal is not sufficient [10, 15, 17, 22, 24, 28]. The decision to use TTO for exposure could be taken intraoperatively if the patella cannot be retracted with the knee at 90° of flexion without risking patellar tendon avulsion. TTO can be used without regard to surgical approach performed. It can be associated both medial and lateral parapatellar approach improving clinical and radiological outcomes both in difficult primary and revision surgery. In this regard, Nikolopoulos et al. [21] reported that the anatomical axis is accurately restored only in 22–30% of valgus knees dealt with a standard medial approach, while the use of a LPA combined with TTO shows a significant improvement of anatomical axis restoration [21, 40, 41]. Two main clinical conditions can lead to the use of TTO in primary TKA: rheumatoid arthritis and severe valgus deformity. Indeed, more than one author have reported a comparison between a classic medial parapatellar approach and a lateral approach with TTO in the event of these two clinical presentations [15, 20, 21]. LPA can help anatomical axis restoration, as the contracted structures are easily accessed and, in severe cases, the patellar alignment may be achieved by displacing the osteotomised tubercle. Furthermore, the most commonly reported complications in patients with valgus deformities who undergo TKA are tibiofemoral instability (2 to 70%), recurrent valgus deformity (4–38%), postoperative motion deficits requiring manipulation (1–20%), wound problems (4–13%), patellar stress fracture or osteonecrosis (1–12%), patellar tracking problems (2–10%), and peroneal nerve palsy (1–4%) [20]. Most of the articles included show a reduction of the rate of these complications performing TTO. Nevertheless, many surgeons prefer not to routinely perform the osteotomy because of the perceived risk of nonunion, tibial tubercle migration, proximal tibial fracture or metalware prominence [19]. Therefore, revision represents the main scope of this technique. There are many parameters to be considered before performing revision total knee arthroplasty: the elapsed time between the index and revision procedure; the cause of implant failure; patient age at time of revision; partial or total revision of the implants. Consequently, determining the cause of failure is essential when planning a revision procedure. The main causes of failure are: loosening, instability, infection, malalignment, wear and complications patella-related. The distribution of these causes depends on time elapsed since primary surgery. Indeed, early revisions (< 2 years) were mostly performed for infection and instability, whereas late revisions (> 2 years) were mostly performed for polyethylene wear and loosening. Hardeman et al. [3] assessed that early revisions failed more frequently, aseptic revisions achieved significantly better knee scores and range of motion than septic revisions, but the pain and functional scores were similar. The performance of a TTO did not statistically influence the outcomes. Similar conclusions are reported by other authors [3, 27, 30, 42]. Mendes et al. [30] and van den Broeck et al. [42] both reported complications directly related to the TTO in 7% of their patients. However, the authors [30, 42] concluded that when adequate exposure cannot be obtained, step-cut TTO is a safe and reproducible procedure if strict attention is paid to technique and fixation. It does not compromise the functional results of TKA. Reliable bone healing can be expected with intramedullary extension or repeat TTO in revision TKA. However, intramedullary extension of the osteotomy prolongs the union time of the tibial tubercle [27]. Moreover, TTO seems to provide superior clinical outcomes than other surgical approaches, as QS, in two-stage RTKAs in prosthetic knee infections [18], with comparable complications. The findings confirm those reported by Mendes [30]. He concluded that TTO is an efficacious alternative for surgical exposure in two-stage RTKAs for prosthetic knee infections regarding clinical results, healing potential of the osteotomized fragment, and complication rates. As underlined by literature, most of complications occurred in early series, where the surgical technique was less standardized and the method of osteosynthesis never unanimous. Dolin [6] and Wolf et al. [39] reported major complications in the following cases: short osteotomy fragment (< 3 cm), insufficient fixation (with an only screw or stapling), or the absence of step-cut osteotomy. Whiteside and Ohl [11] gave the first contribution to standardize the surgical technique, reporting good outcomes and allowing further studies with lower complication rate. In conclusion, although further studies with larger groups of patients and a longer follow-up period is needed to better evaluate the outcomes and safety of TTO, it seems clear how this technique, under correct indications, could be a reliable option to increase exposure during total knee arthroplasty. It can be performed sequentially without increasing the risk of nonunion or fracture and is particularly effective in two-stage infected procedures where the osteotomy can be safely left unfixed between stages [26].
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007 Apr 89(4):780–785. https://doi.org/10.2106/JBJS.F.00222
Bae DK, Song SJ, Heo DB et al (2013) Long-term survival rate of implants and modes of failure after revision total knee arthroplasty by a single surgeon. J Arthroplasty 2013 28(7):1130
Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J (2012) Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1049–1056. https://doi.org/10.1007/s00167-011-1624-8
Piedade SR, Pinaroli A, Servien E, Neyret P (2009) Revision after early aseptic failures in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17:248–253
Lombardi AV Jr, Berend KR, Adams JB, (2014) Why knee replacements fail in 2013 patient, surgeon, or implant? Bone Joint J. 96-B (11 Supple A):101–104. https://doi.org/10.1302/0301-620X.96B11.34350
Dolin MG (1983) Osteotomy of the tibial tubercle in total knee replacement. A technical note. J Bone Joint Surg Am 65(5):704–706
Seth L, Sherman, Brandon J, Erickson GL, Cvetanovich, Peter N, Chalmers, Jack Farr II, Bernard R. Bach Jr, BJ Cole. Tibial tuberosity osteotomy: indications, techniques, and outcomes. (2014) Am J Sports Med, 42, 8 https://doi.org/10.1177/0363546513507423
DK Lee, JH Wang, SH Kang, JH Kim, R Haque, BH Lee. The clinical and radiological results of individualized surgical treatment depending on pathologic abnormalities in recurrent patellar dislocation: low recurrence rate, but unintended patella baja. (2016) Knee Surg Sports Traumatol Arthrosc https://doi.org/10.1007/s00167-017-4697-1
Denham RA, Bishop RE (1978) Mechanics of the knee and problems in reconstructive surgery. J Bone Joint Surg Br 60-B(3):345–352
Whiteside LA (1995) Exposure in difficult total knee arthroplasty using tibial tubercle osteotomy. Clin Orthop Relat Res 321:32–35
Whiteside LA, Ohl MD (1990) Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res 1990 260:6–9
Abdel MP, Della Valle CJ (2016) The surgical approach for revision total knee arthroplasty. Bone Joint J; 98-B(1 Suppl A):113–115. https://doi.org/10.1302/0301-620X.98B1.36315
Gonzalez-Solıs JMB, Dıez-Santacoloma I, Llorens AI (2016) Anterior tibial tubercle osteotomy using cerclage wire fixation in total knee replacement: a modification of the usual technique. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-016-1870-z
Trieb K, Schmid M, Stulnig T et al (2008) Long-term outcome of total knee replacement in patients with rheumatoid arthritis. Joint Bone Spine 75:163–166
Eid AS, Nassar WAM, Fayyad TAM (2016) Total knee replacement with tibial tubercle osteotomy in rheumatoid patients with stiff knee International Orthopaedics. (SICOT) 40:2289–2293. https://doi.org/10.1007/s00264-016-3167-6
James A, Rand MD, Ries GH, Landis AG, Rosenberg SH (2003) Intraoperative assessment in revision total knee arthroplasty. J Bone Joint Surg Am 85-A(Suppl 1):S26–S37
Sun Z, Patil A, Song EK, Kim HT, Seon JK, (2015) Comparison of quadriceps snip and tibial tubercle osteotomy in revision for infected total knee arthroplasty International Orthopaedics (SICOT). 39:879–885 https://doi.org/10.1007/s00264-014-2546-0
Bruni D, Iacono F, Sharma B, Zaffagnini S, Marcacci M (2013) Tibial tubercle osteotomy or quadriceps snip in two-stage revision for prosthetic knee infection? A randomized prospective study Clin Orthop Relat Res 471:1305–1318. https://doi.org/10.1007/s11999-012-2763-z
Chalidis BE, Ye K, Sachinis NP, Hawdon G, McMahon S (2014) Lateral parapatellar approach with tibial tubercle osteotomy for the treatment of non-correctable valgus knee osteoarthritis A retrospective clinical study. Knee 21:204–208. https://doi.org/10.1016/j.knee.2013.05.008
Apostolopoulos AP, Nikolopoulos DD, Polyzois I, Nakos A, Liarokapis S, Stefanakis G, Michos IV, (2011) Total knee arthroplasty in severe valgus deformity: Interest of combining a lateral approach with a tibial tubercle osteotomy Orthop Traumatol: Surg Res 96, 777–784. https://doi.org/10.1016/j.otsr.2010.06.008
Nikolopoulos DD, Polyzois I, Apostolopoulos AP, Rossas C, Moutsios-Rentzos A, Michos IV, (2011) Total knee arthroplasty in severe valgus knee deformity: comparison of a standard medial parapatellar approach combined with tibial tubercle osteotomy Knee Surg Sports Traumatol Arthrosc. 19:1834–1842 https://doi.org/10.1007/s00167-011-1474-4
Piedade SR, Pinaroli A, Servien E, Neyret P (2008) Tibial tubercle osteotomy in primary total knee arthroplasty: a safe procedure or not? Knee 15:439–446. https://doi.org/10.1016/j.knee.2008.06.006
Hay GC, Kampshoff J, Kuster MS, TRIAL (2011) Lateral subvastus approach with osteotomy of the tibial tubercle for total knee replacement a two-year prospective, randomised, blinded controlled. J Bone Joint Surg [Br] 92-B:862–866. https://doi.org/10.1302/0301-620X.92B6
Tabutin J, Morin-Salvo N, Torga-Spak R, Cambas PM, Vogt F, (2011) Tibial tubercule osteotomy during medial approach to difficult knee arthroplasties Orthop Traumatol: Surg Res 97, pp 276–286 https://doi.org/10.1016/j.otsr.2011.01.007
Chinzei N, Ishida K, Kuroda R, Matsumoto T, Kubo S, Iguchi T, Chin T, Akisue T, Nishida K, Kurosaka M, Tsumura N, (2014) Tibial tubercle osteotomy with screw fixation for total knee arthroplasty. Orthopedics. 37(4): e367–e373
Punwar SA, Fick DP, Khan RJK (2017) Tibial tubercle osteotomy in revision knee arthroplasty. J Arthroplast 32:903e907. https://doi.org/10.1016/j.arth.2016.08.029
Chalidis BE, Ries MD (2009) Does repeat tibial tubercle osteotomy or intramedullary extension affect the union rate in revision total knee arthroplasty? A retrospective study of 74 patients. Acta Orthop 2009 80(4):426–431. https://doi.org/10.3109/17453670903110683
Choi HM, Burke D, Malchau H, Kwon YM (2012) Utility of tibial tubercle osteotomy in the setting of periprosthetic infection after total knee arthroplasty International Orthopaedics. (SICOT) 36:1609–1613. https://doi.org/10.1007/s00264-012-1541-6
Le Moulec YP, Bauera T, Klouchea S, Hardy P, (2014) Tibial tubercle osteotomy hinged on the tibialis anterior muscle and fixed by circumferential cable cerclage in revision total knee arthroplasty. Orthop Traumatol: Surg Res 100 539–544
Mendes MW, Caldwell P, Jiranek WA (2004) The results of tibial tubercle osteotomy for revision total knee arthroplasty J Arthroplast 19 2 https://doi.org/10.1016/j.arth.2003.08.013
Young CF, Bourne RB, Rorabeck CH (2008) Tibial tubercle osteotomy in total knee arthroplasty surgery. J Arthroplast Vol 23 No 3 https://doi.org/10.1016/j.arth.2007.02.019
Zonnenberg CBL, Van den Bekerom MPJ, de Jong T, Nolte PA, (2014) Tibial tubercle osteotomy with absorbable suture fixation in revision total knee arthroplasty: a report of 23 cases Arch Orthop Trauma Surg. 134:667–672 https://doi.org/10.1007/s00402-014-1950-7
Abbas AMI, Williams RLL, Khan WS, Ghandour A, Morgan-Jones RL (2016) Tibial crest osteotomy in extensile knee exposure—a modified, low-energy, suture technique J Arthroplast 31: 383–388. https://doi.org/10.1016/j.arth.2015.08.030
Hirschmann MT, Hoffmann M, Krause R, Jenabzadeh RA, Arnold MP, Friederich NF (2010) Anterolateral approach with tibial tubercle osteotomy versus standard medial approach for primary total knee arthroplasty: does it matter? BMC Musculoskelet Disord 11:167
Younger AS, Duncan CP, Masri BA (1998) Surgical exposures in revision total knee arthroplasty. J Am Acad Orthop Surg 6(1):55–64
Della Valle CJ, Berger RA, Rosenberg AG (2006) Surgical exposures in revision total knee arthroplasty. Clin Orthop Relat Res 446:59–68
Barrack RL, Smith P, Munn B, Engh G, Rorabeck C (1998) The ranawat award: comparison of surgical approaches in total knee arthroplasty. Clin Orthop Relat Res 356(8):16–21 Surg Am 65):1087–1098
Barrack RL (1999) Specialized exposure for revision total knee arthroplasty: quadriceps snip and patellar turndown. Instr Course Lect 48:149–152
Wolf AM, Hungerford DS, Krackow KA, Jacobs MA (1989) Osteotomy of the tibial tubercle during total knee replacement: a report of twenty-six cases. J Bone Joint Surg Am 71(6):848–852
Karachalios T, Sarangi PP, Newman JH (1994) Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg [Br] 76:938–942
Stern SH, Moeckel BH, Insall JN (1991) Total knee arthroplasty in valgus knee. Clin Orthop Relat Res 273:5–8
van den Broek CM, van Hellemondt GG, Jacobs WCH, Wymenga AB (2006) Step-cut tibial tubercle osteotomy for access in revision total knee replacement. Knee 13:430–434. https://doi.org/10.1016/j.knee.2006.07.003
Langen S, Gaber S, Zdravkovic V, Giesinger K, Jost B, Behrend H (2016) Lateral subvastus approach with tibial tubercle osteotomy for primary total knee arthroplasty: clinical outcome and complications compared to medial parapatellar approach (2016. Eur J Orthop Surg Traumatol 26:215–222. https://doi.org/10.1007/s00590-015-1718-y
Segur JM, Vilchez-Cavazos F, Martinez-Pastor JC, Macule F, Suso S, Acosta-Olivo C (2014) Tibial tubercle osteotomy in septic revision total knee arthroplasty. (2014) Arch Orthop Trauma Surg 134:1311–1315. https://doi.org/10.1007/s00402-014-2064-y
RADULESCU R, BADILA A, NUTIU O, JAPIE I, TERINTE S, RADULESCU D, MANOLESCU R (2013) Extended exposure in difficult total knee arthroplasty using tibial tubercle osteotomy MAEDICA. J Clin Med 2013 8(4):380–383
Choi HR, Kwon YM, Burke DW, Rubash HE, Malchau H (2012) The outcome of sequential repeated tibial tubercle osteotomy performed in 2-stage revision arthroplasty for infected total knee arthroplasty. J Arthroplast 27 8. https://doi.org/10.1016/j.arth.2012.03.016 2012
Wishart AMP, Huegli RW, Amsler F, Friederich NF, Hirschmann MT (2012) Anterolateral approach using tibial tubercle osteotomy for total knee arthroplasty: can we predict failure? Int Orthop 36:2485–2490. https://doi.org/10.1007/s00264-012-1693-4
Ries MD, Richman JA, (1996) Extended tibial tubercle ostetomy in total knee arthroplasty. J Arthroplasty 11 8: 964–967
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human and animal participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Divano, S., Camera, A., Biggi, S. et al. Tibial tubercle osteotomy (TTO) in total knee arthroplasty, is it worth it? A review of the literature. Arch Orthop Trauma Surg 138, 387–399 (2018). https://doi.org/10.1007/s00402-018-2888-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2888-y