Abstract
Introduction
3T MRI has become increasingly available for better imaging of interosseous ligaments, TFCC, and avascular necrosis compared with 1.5T MRI. This study assesses the sensitivity and specificity of 3T MRI compared with arthroscopy as the gold standard.
Patients and methods
Eighteen patients were examined with 3T MRI using coronal T1-TSE; PD-FS; and coronal, sagittal, and axial contrast-enhanced T1-FFE-FS sequences. Two musculoskeletal radiologists evaluated the images independently. Patients underwent diagnostic arthroscopy.
Results
The classifications of the cartilage lesions showed good correlations with the arthroscopy findings (κ = 0.8–0.9). In contrast to the arthroscopy, cartilage of the distal carpal row was very good and could be evaluated in all patients on MRI. The sensitivity for the TFCC lesion was 83%, and the specificity was 42% (radiologist 1) and 63% (radiologist 2). For the ligament lesions, the sensitivity and specificity were 75 and 100%, respectively, with a high interobserver agreement (κ = 0.8–0.9).
Discussion
3T MRI proved to be of good value in diagnosing cartilage lesions, especially in the distal carpal row, whereas wrist arthroscopy provided therapeutic options. When evaluating the surgical therapeutical options, 3T MRI is a good diagnostic tool for pre-operatively evaluating the cartilage of the distal carpal row.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) has become an important diagnostic tool in the evaluation of wrist pain. In particular, MRI is a widely used diagnostic tool for the evaluation of avascular necrosis, occult fractures, infections, neoplasms, cartilage, intracarpal ligaments, and triangular fibrocartilage [1,2,3]. An imaging evaluation of the wrist is challenging for the radiologist, because the structures are small and have a complex anatomy. Some investigators have reported an image quality that is sufficient for diagnostic purposes when imaging the wrist with a low-field-strength (i.e., 0.5T or less); however, most magnetic resonance (MR) imagers prefer a high-field-strength (i.e., 1T or 1.5T) [4]. MRI at 3T has become increasingly available for clinical use and provides a better imaging of the interosseous ligaments and the triangular fibrocartilage complex compared with 1.5T MRI [5,6,7].
The purpose of our study was to compare high-resolution 3T MR images of the wrist with the intraoperative findings obtained by arthroscopy for detection of triangular fibrocartilage injuries, cartilage damage, avascular necrosis, and intrinsic ligaments.
Patients and methods
Eighteen patients were examined, and MRI was performed with a 3T imaging system using coronal T1-TSE; PD-FS; and coronal, sagittal, and axial contrast-enhanced T1-FFE-FS sequences with a 1.5-mm slice thickness. A custom-made dedicated bilateral phased-array surface coil with 2 × 2 elements (total area 5 × 10 cm) on each side was used with the 3T system.
The MR images were evaluated retrospectively by two musculoskeletal radiologists working independently. Both radiologists were blinded to the findings presented in the surgery reports, but they knew the clinical symptoms from the patient documents.
The pathology of the cartilage surfaces of the proximal and distal carpal rows was classified according to the Outerbridge and Recht classification [8]. The signal change with a Recht Score of 1 was very difficult to describe. With high-resolution MRI differentiation, the grades of 2–4 were possible. Lesions of the TFCC were classified according to Palmer, and osteonecrosis in the plain radiographs were classified according to Lichtman. The existence of ligament lesions and synovialitis was also analysed.
Patients underwent subsequent arthroscopy of the wrist by board certified hand surgeons. Wrist arthroscopy was performed under an axillary block or general anaesthesia using standard small joint arthroscopes (diameter 2.4 mm) with 30° viewing angles (Karl Storz, Tuttlingen, Germany) and distraction of the wrist via finger traps. The radiocarpal joint was examined using the 3/4 dorsal compartment portal. The 6R portal was used as a second portal, especially for repair of the TFCC or to obtain a probe. The midcarpal joint was inspected through a portal either radial or ulnar to the fourth compartment. Evaluation of the midcarpal joint was not possible for three patients. The wrist cartilage at the fossa lunata, scaphoidea, lunate, and triquetrum was assessed using the Outerbridge classification.
Lesions of the TFCC were assessed using the Palmar classification. The wrist arthroscopy also detected ligament lesions of the scapholunate ligament. For osteonecrosis of the lunate, the Bain and Begg classification based on the number of articular surfaces of the lunate and adjacent articulation, which are non-functional, was used, but this was not possible in all cases because of the failure to perform arthroscopy of the midcarpal joint in three cases.
The MR findings were compared to the arthroscopic findings, and the sensitivity and specificity of the MRI were compared with the findings from arthroscopy. The 95% confidence intervals were calculated from standard statistical tables for binomial data.
Weighted kappa values (κ), sensitivity, specificity, and positive and negative predictive values were calculated. The interobserver agreement was calculated.
Results
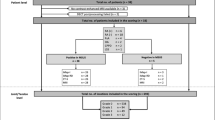
Eighteen patients, 6 females and 12 males, with an average age of 34.8 years (range 17–51 years) were examined. In all patients, the indication for arthroscopy and MR imaging was chronic wrist pain (Table 1). The initial radiological diagnostics included plain radiographs, and then, 3T MRI was done for specification. In three patients, there was a suspicion of a scapholunate ligament lesion, and in four patients, Kienböck’s disease was suspected.
After performing high-resolution MRI, lesions of the TFCC were detected in 12 patients by radiologist 1 (MRI 1) and in 10 patients by radiologist 2 (MRI 2) (Table 2). Among these lesions, 4 (MRI 1) and 3 (MRI 2) were classified as traumatic lesions, whereas 8 (MRI 1) and 6 (MRI 2) were classified as degenerative lesions according to the Palmer classification. According to the arthroscopy, 6 TFCC lesions were detected, 2 of which were traumatic lesions, and 4 of which were degenerative lesions (Fig. 1; Table 2).
Lesions of the scapholunate ligament were detected in three cases by both radiologists. With our MRI sequences, we are able to distinguish the different parts of the SL ligament. We measured with a voxel size of 0.28 × 0.28 × 1.5 mm, and this small slice thickness and high spatial resolution allowed us to also describe the dorsal partial ruptures of the SL ligament. During arthroscopy, scapholunate ligament ruptures were detected in three cases and in one additional case. Lesions of the lunotriquetral ligament could not be detected with arthroscopy or MRI (Table 2).
In the plain radiographs that were graded according to Lichtman, two patients were graded 3b, one was graded as 2, and one was graded as 4. In the MRI findings, four patients demonstrated avascular necrosis. According to MRI 1, two were graded as 4, one was graded as 3b, and one was graded as 1. According to MRI 2, two were graded as 4, one was graded as 3b, and one was graded as 2 (Table 2). By wrist arthroscopy and grading according to Bain and Begg (*of limited value because evaluation of the midcarpal joint was not possible in three patients), one patient was graded as 1. This patient was later treated with a proximal row carpectomy. Two patients were treated with an arthrodesis and one with a proximal row carpectomy, graded as 2b, 4* and one.
The sensitivity and specificity for the TFCC lesions for the first radiologist (MRI 1) were 83 and 42%, respectively, with a positive predictive value of 42% and a negative predictive value of 83%.
Concerning the ligament lesions, the sensitivity and specificity were 75 and 100%, respectively, with a positive predictive value of 100% and a negative predictive value of 93%.
For the second radiologist (MRI 2), the sensitivity and specificity for the TFCC lesions were 83 and 63%, respectively, with a positive predictive value of 45% and a negative predictive value 63%.
Concerning the ligament lesions, the sensitivity and specificity were 75 and 100%, respectively, whereas the positive predictive value was 21% and the negative predictive value was 100%.
They detected contrast enhancement and thinning of the TFCC and also degenerated cartilage with grade 4 thinning, which was highly reproducible in high-resolution 3T MRI.
Concerning the detection of Kienböck’s disease, the sensitivity and specificity were 100% for both observers. The interobserver agreement between the radiologists in MRI was very high in all parameters (κ = 0.8–0.9).
Detection of osteoarthritis in the radiocarpal and midcarpal joints was frequently seen by either arthroscopy or MRI. High-resolution MRI showed a very good correlation to arthroscopy (κ = 0.8–0.9) for both observers. The cartilage pathologies on 3T MRI were classified according Recht [9]. The signal change for a Recht score 1 was very difficult to describe. With high-resolution MRI, differentiation grades of 2–4 were possible.
Arthroscopy failed in the evaluation of the distal carpal cartilage row in three cases, because the anatomy was not assessable. Unlike in the arthroscopy, the cartilage of the distal carpal row was very good and could be evaluated in all patients in MR images (Table 3).
Discussion
MRI has become an important and standard diagnostic tool for evaluating pathologies of the wrist and hand. MRI has been shown to have a high degree of accuracy for investigating the interosseous ligaments, especially the scapholunate ligament, avascular necrosis, occult fractures, infections, neoplasms, cartilage, and triangular fibrocartilage, and it has the benefit of being non-invasive [1,2,3, 10,11,12]. However, arthrography was found to be more accurate than MRI, especially when assessing the lunotriquetral ligament and triangular fibrocartilage [13, 14]. CT and MR arthrography have a very high degree of accuracy for diagnosing tears of the SLL, LTL, and TFCC, with both of these methods being more accurate than the conventional MRI. [15].
Arthroscopy of the wrist joints allows direct inspection of the articular cartilage and the interosseous ligaments, and may yield a diagnosis in 70% or more of cases [16, 17]. Arthroscopy has been found to be superior to arthrography for detecting intraarticular pathologies, especially in the investigation of chronic wrist pain and TFCC tears [18,19,20]. When comparing arthroscopy with 1.5T MRI and with specific wrist coils, MRI achieved a sensitivity of 80–90% [21,22,23], and diagnosis of TFCC injuries demonstrated a sensitivity of 86% and a specificity of 82% with MRI when compared with arthroscopic findings [2]. Meier et al. demonstrated a correlation of 93.6% in detecting TFCC lesions with MRI arthrography and arthroscopy; other measures included a sensitivity of 94%, specificity of 89%, positive predictive value of 91%, and negative predictive value of 93% [19]. In a prospective study of 43 patients with chronic wrist pain, the sensitivity and specificity of MRI compared with arthroscopy were 0.8 and 0.7 for triangular fibrocartilage complex pathology, 0.37 and 1.0 for the scapholunate ligament, and 0 and 0.97 for the lunotriquetral ligament, respectively [24]. Arthroscopy and arthrotomy have been compared with an error rate for arthroscopy of 6%, but the patients undergoing arthrotomy were not representative of the total number of patients studied [25].
Several studies reported that MRI was unsatisfactory for diagnosing TFCC injuries and that it was inferior to arthroscopy or arthrography [24, 26,27,28,29]. However, this depends on the slice thickness, which is normally 3 mm in a clinical 1.5T setting, as well as the resulting partial volume effect and the low spatial resolution. Therefore, a reliable MR technique for accurate diagnosis of TFCC injuries is desirable.
MRI evaluation of the wrist presents special challenges for the radiologist, because the clinically important structures of the wrist are small and have a complex anatomy with an inadequate contrast between them and the surrounding structures [30]. Actually, a field strength of 1.5T has been the reference standard for clinical MR systems and has been used for virtually all MR applications [5,6,7]. A field strength of 1.5T with a specific wrist coil can create very good images when carefully performed and when the slices are not too thick. Recently, a higher field strength, such as 3T, is becoming increasingly available for clinical use.
3T magnetic resonance imaging demonstrates a linear increase in the signal-to-noise ratio (SNR) compared with lower field strength imagers, which, in turn, allows for incremental increases in the spatial resolution without a substantial sacrifice in time [6]. For small joints with small ligaments and thin cartilage surfaces, 3T offers significant improvements in the diagnostic ability with improvements in accuracy when compared with 1.5T [5,6,7, 31].
The visibility of various small anatomical structures, such as the triangular fibrocartilage complex, intercarpal cartilage, median, and ulnar nerves, was rated significantly higher at 3T than at 1.5T [5, 31, 32]. Examinations performed with 3T MRI also showed a better detection of the carpal ligaments [15, 32]. Furthermore, images obtained at 3T allowed microscopic analysis of the bone structure, and differences in the structure of the spongy bone between normal and markedly osteoporotic subjects were well depicted [33].
Comparing the diagnostic performance of 3T and 1.5T MRI with regard to the detection of cartilage lesions showed that with optimised high-resolution sequences, the detection of cartilage lesions is better at 3T than at 1.5T [8, 34,35,36].
Image comparison of high-resolution MRI of the wrist and finger joints in patients with rheumatoid arthritis revealed a better quality at higher field strengths in evaluations of the extent of bone oedema, synovitis, and identification of small bone erosions. The image quality of T1-weighted images was rated 14–22% better at 3T compared with 1.5 T. Moreover, the rating for the T2-weighted images acquired at 3T was one point better in the five-point scale used in that study [37].
Correlating 1.5T and 3T MRI with wrist arthroscopy in patients with ulnar-sided wrist pain demonstrated a sensitivity of 85% and a specificity of 75% at 1.5T MRI compared with the arthroscopy, whereas 3T wrist MRI had a sensitivity of 94% and a specificity of 88% [7].
The sensitivity, specificity, and accuracy of 3T wrist MRI for the TFCC were consistently higher compared with those of 1.5T wrist MRI. This trend suggested that 3T wrist MRI provides improved capability for detection of TFCC injuries. However, given the available sample size, the confidence intervals around the point estimates are wide and overlapping. Therefore, the authors concluded that further studies are needed to confirm or refute the results of the estimated sensitivity, specificity, and accuracy parameters.
High-resolution MRI proved to be of very good value compared with diagnostic arthroscopy as the gold standard. With high interobserver agreement, lesions of the TFCC could be detected with a high sensitivity of 83%. The specificity of this method was moderate with 63%. Nevertheless, until now, arthroscopy is the gold standard for detection of TFCC lesions and determination of therapeutic options [38]. The high diagnostic reliability is based on a thorough examination that includes complementary clinical and radiological procedures [39].
Concerning the detection of ligament lesions and cartilage damage, high-resolution MRI demonstrated a high sensitivity and specificity of 75 and 100%.
A comparison of 3T MRI and arthroscopy demonstrated a 3T MRI sensitivity of 86% for detection of TFCC tears, 89% for detection of scapholunate tears and 82% for detection of lunatotriquetral tears. The MRI specificity for the detection of tears was 100%. The MR arthrography sensitivity for the detection of ligament and TFCC tears was 100% [40]. MRI at 3T was sensitive and specific for the detection of wrist ligament tears. MR arthrography showed a greater sensitivity for ligament evaluation, but it could result in false-positive findings because of micro perforations [40].
For ligament lesions, especially for carpal instability, arthroscopy allows for direct inspection of all anatomical details, joint surfaces, degree of ligament tears, and facilitates decisions for appropriate treatments to repair or reconstruct a lesion [41]. For ligament lesions, especially for carpal instability, arthroscopy allows direct inspection of all anatomical details (except the palmar SL and LT ligaments or dorsal joint surfaces), the degree of ligament tears and facilitates the decision for appropriate treatment to repair or reconstruct a lesion [41]. The role of arthroscopy in SL instability is clear and proven, especially in diagnosing pre-dynamic and dynamic instability [41, 42]. The other role is an assessment of the articular cartilage of the radiocarpal and midcarpal joints [41].
For LT instability, arthroscopy can assess the LT ligament, mobility in the LT-joint, grading of the instability, and rule out other causes [41].
Arthroscopy is currently the gold standard for confirming and consolidating the diagnosis of the underlying cause of carpal instability by staging the extent of hypermobility and the degree of secondary articular cartilage wear [41]. Another advantage of the arthroscopy is the potential for taking tissue probes [43]. Using additional video documentation, assessment of TFCC lesions, as well as its tension, was improved [44].
On the contrary, some authors think that in spite of the advantages that 3T MRI has over 1.5T MRI, using 1.5T MRI with dedicated wrist coils is mostly sufficient [45, 46]. However, MRI is most often conducted without wrist coils in clinical practice [47].
Further improvement with 7T wrist MRI, which provides excellent diagnostic images of the wrist, is actually used only for research [45]. 7T MRI with increased spatial resolution is available and promising tools for an improved visualisation of the ulnocarpal complex [48].
Wrist arthroscopy is the ‘‘gold standard’’ in the diagnosis of TFCC injuries, intraarticular pathologies, and especially investigation of chronic wrist pain [45, 49]. It allows an accurate assessment of the TFCC, and especially distinguishes whether a lesion is traumatic or degenerative [45]. There are several techniques to evaluate the TFCC during wrist arthroscopy, including the trampoline [50], the hook [51] and needle tests [52]. Furthermore, arthroscopy provides the opportunity for therapeutic interventions.
We appreciate that our study shows limitations. First, the study group is a small patient series. Second, the study group includes patients with heterogeneous causes of chronic wrist pain, and the collective is divided into several small subgroups, and thus, general recommendations cannot be given. In addition, the influence of the surgeon’s experience in the results of arthroscopy cannot be estimated.
In summary, high-resolution MRI could be of good value for the evaluation of intrinsic ligaments and cartilage damage. In contrast, wrist arthroscopy provides the opportunity for therapeutic interventions and the treatment of TFCC. Both methods of evaluation complement each other. For example, in patients with chronic wrist pain, especially before carpal row carpectomy, 3T MRI could be a good diagnostic tool to evaluate the cartilage.
References
Daunt N (2002) Magnetic resonance imaging of the wrist: anatomy and pathology of interosseous ligaments and the triangular fibrocartilage complex. Curr Probl Diagn Radiol 31(4):158–176
Totterman SM, Miller RJ, McCance SE, Meyers SP (1996) Lesions of the triangular fibrocartilage complex: MR findings with a three-dimensional gradient-recalled-echo sequence. Radiology 199(1):227–232
Totterman SM, Seo GS (2001) MRI findings of scapholunate instabilities in coronal images: a short communication. Semin Musculoskelet Radiol 5(3):251–256
Savnik A, Malmskov H, Thomsen HS, Bretlau T, Graff LB, Nielsen H, Danneskiold-Samsoe B, Boesen J, Bliddal H (2001) MRI of the arthritic small joints: comparison of extremity MRI (0.2 T) vs high-field MRI (1.5 T). Eur Radiol 11(6):1030–1038
Saupe N, Prussmann KP, Luechinger R, Bosiger P, Marincek B, Weishaupt D (2005) MR imaging of the wrist: comparison between 1.5- and 3-T MR imaging–preliminary experience. Radiology 234(1):256–264
Amrami KK, Felmlee JP (2008) 3-Tesla imaging of the wrist and hand: techniques and applications. Semin Musculoskelet Radiol 12(3):223–237
Anderson ML, Skinner JA, Felmlee JP, Berger RA, Amrami KK (2008) Diagnostic comparison of 1.5 Tesla and 3.0 Tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg Am 33(7):1153–1159
Link TM, Stahl R, Woertler K (2007) Cartilage imaging: motivation, techniques, current and future significance. Eur Radiol 17(5):1135–1146
Stehling C (2011) Scoring systems to semiquantitatively grage cartilage pathology with MRI. In: Link T (ed) Cartilage Imaging. Springer, New York. doi:10.1007/978-1-4419-8438-8_8
Saupe N, Pfirrmann CW, Schmid MR, Schertler T, Manestar M, Weishaupt D (2007) MR imaging of cartilage in cadaveric wrists: comparison between imaging at 1.5 and 3.0 T and gross pathologic inspection. Radiology 243(1):180–187
Zanetti M, Saupe N, Nagy L (2007) Role of MR imaging in chronic wrist pain. Eur Radiol 17(4):927–938
Zlatkin MB, Rosner J (2006) MR imaging of ligaments and triangular fibrocartilage complex of the wrist. Radiol Clin North Am 44(4):595–623
Shionova K, Nakamura R, Imaeda T, Makino N (1998) Arthrography is superior to magnetic resonance imaging for diagnosing injuries of the triangular fibrocartilage. J Hand Surg Br 23(3):402–405
Gundry CR, Kursunoglu-Brahme S, Schwaighofer B, Kang HS, Sartoris DJ, Resnick D (1990) Is MR better than arthrography for evaluating the ligaments of the wrist? In vitro study. AJR Am J Roentgenol 154(2):337–341
Lee YH, Choi YR, Kim S, Song HT, Suh JS (2013) Intrinsic ligament and triangular fibrocartilage complex (TFCC) tears of the wrist: comparison of isovolumetric 3D-THRIVE sequence MR arthrography and conventional MR image at 3 T. Magn Reson Imaging 31(2):221–226
Adolfsson L (1994) Arthroscopic diagnosis of ligament lesions of the wrist. J Hand Surg Br 19(4):505–512
Adolfsson L, Povlsen B (2004) Arthroscopic findings in wrists with severe post-traumatic pain despite normal standard radiographs. J Hand Surg Br 29(3):208–213
Cooney WP (1993) Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg 18(5):815–822
Meier R, Schmitt R, Krimmer H (2005) Wrist lesions in MRI arthrography compared with wrist arthroscopy. Handchir Mikrochir Plast Chir 37(2):85–89
Vanden Eynde S, De Smet L, Fabry G (1994) Diagnostic value of arthrography and arthroscopy of the radiocarpal joint. Arthroscopy 10(1):50–53
Zlatkin MB, Chao PC, Osterman AL, Schnall MD, Dalinka MK, Kressel HY (1989) Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology 173(3):723–729
Cerofolini E, Luchetti R, Pederzini L, Soragni O, Colombini R, D’Alimonte P, Romagnoli R (1990) MR evaluation of triangular fibrocartilage complex tears in the wrist: comparison with arthrography and arthroscopy. J Comput Assist Tomogr 14(6):963–967
Pederzini L, Luchetti R, Soragni O, Alfarano M, Montagna G, Cerofolini E, Colombini R, Roth J (1992) Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy 8(2):191–197
Johnstone DJ, Thorogood S, Smith WH, Scott TD (1997) A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg Br 22(6):714–718
Rettig ME, Amadio PC (1994) Wrist arthroscopy. Indications and clinical applications. J Hand Surg Br 19(6):774–777
Morley J, Bidwell J, Bransby-Zachary M (2001) A comparison of the findings of wrist arthroscopy and magnetic resonance imaging in the investigation of wrist pain. J Hand Surg [Br] 26(6):544–546
Shionova K, Nakamura R, Imaeda T, Makino N (1998) Arthrography is superior to magnetic resonance imaging for diagnosing injuries of the triangular fibrocartilage. J Hand Surg [Br] 23(3):402–405
Kato H, Nakamura R, Shionoya K, Makino N, Imaeda T (2000) Does high-resolution MR imaging have better accuracy than standard MR imaging for evaluation of the triangular fibrocartilage complex? J Hand Surg [Br] 25(5):487–491
Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange R, Osterman AL, Bednar JM, Taras JS, Culp RW (2002) Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol 178(2):419–422
Smith DK (1995) MR imaging of normal and injured wrist ligaments. Magn Reson Imaging Clin N Am 3(2):229–248
Stehling C, Langer M, Bachmann R, Kraemer S, Kooijman H, Heindel W, Vieth V (2009) Three-Tesla magnetic resonance imaging of the wrist: diagnostic performance compared to 1.5-T. J Comput Assist Tomogr 33(6):934–939
Lenk S, Ludescher B, Martirosan P, Schick F, Claussen CD, Schlemmer HP (2004) 3.0 T high-resolution MR imaging of carpal ligaments and TFCC. Rofo 176(5):664–667
Ludescher B, Martirosian P, Lenk S, Machann J, Dammann F, Schick F, Claussen C, Schlemmer H (2005) High-resolution magnetic resonance imaging of trabecular bone in the wrist at 3 tesla: initial results. Acta Radiol 46(3):306–309
Masi JN, Sell CA, Phan C, Han E, Newitt D, Steinbach L, Majumdar S, Link TM (2005) Cartilage MR imaging at 3.0 versus that at 1.5 T: preliminary results in a porcine model. Radiology 236(1):140–150
Wong S, Steinbach L, Zhao J, Stehling C, Ma CB, Link TM (2009) Comparative study of imaging at 3.0 T versus 1.5 T of the knee. Skeletal Radiol 38(8):761–769
Stehling C, Bachmann R, Langer M, Nassenstein I, Heindel W, Vieth V (2009) High-resolution magnetic resonance imaging of triangular fibrocartilage complex lesions in acute wrist trauma: image quality at different field strengths. J Comput Assist Tomogr 33(4):579–583
Wieners G, Detert J, Streitparth F, Pech M, Fischbach F, Burmester G, Ricke J, Backhaus M, Bruhn H (2007) High-resolution MRI of the wrist and finger joints in patients with rheumatoid arthritis: comparison of 1.5 Tesla and 3.0 Tesla. Eur Radiol 17(8):2176–2182
Spies CK, Prommersberger KJ, Langer M, Muller LP, Hahn P, Unglaub F (2015) Instability of the distal radioulnar joint: treatment options for ulnar lesions of the triangular fibrocartilage complex. Unfallchirurg 118(8):701–717. doi:10.1053/jhsu.2000.6467
Spies CK, Muller LP, Oppermann J, Hahn P, Unglaub F (2014) Instability of the distal radioulnar joint—an overview of clinical and radiological procedures regarding their efficacies. Handchir Mikrochir Plast Chir 46(3):137–150
Magee T (2009) Comparison of 3-T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. AJR Am J Roentgenol 192(1):80–85. doi:10.2214/AJR.08.1089
Lindau TR (2016) The role of arthroscopy in carpal instability. J Hand Surg Eur 41(1):35–47
Chennagiri RJ, Lindau TR (2013) Assessment of scapholunate instability and review of evidence for management in the absence of arthritis. J Hand Surg Eur 38(7):727–738
Low S, Herold A, Eingartner C (2014) Standard wrist arthroscopy: technique and documentation. Oper Orthop Traumatol 26(6):539–546
Low S, Pillukat T, Prommersberger KJ, van Schoonhoven J (2013) The effect of additional video documentation to photo documentation in wrist arthroscopies on intra- and interobserver reliability. Arch Orthop Trauma Surg 133(3):433–438
Kirchberger MC, Unglaub F, Muhldorfer-Fodor M, Pillukat T, Hahn P, Muller LP, Spies CK (2015) Update TFCC: histology and pathology, classification, examination and diagnostics. Arch Orthop Trauma Surg 135(3):427–437
Sachar K (2012) Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am 37(7):1489–1500
Hahn P, Hausler A, Bruckner T, Unglaub F (2012) Quality rating of MRI regarding TFCC lesions in the clinical practice. Handchir Mikrochir Plast Chir 44(5):310–313
Nobauer-Huhmann IM, Pretterklieber M, Erhart J, Bar P, Szomolanyi P, Kronnerwetter C, Lang S, Friedrich KM, Trattnig S (2012) Anatomy and variants of the triangular fibrocartilage complex and its MR appearance at 3 and 7T. Semin Musculoskelet Radiol 16(2):93–103
Slutsky DJ, Nagle DJ (2008) Wrist arthroscopy: current concepts. J Hand Surg Am 33(7):1228–1244
Hermansdorfer JD, Kleinman WB (1991) Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am 16(2):340–346
Atzei A (2009) New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur 34(5):582–591
Unglaub F, Muller LP, Oppermann J, Hahn P, Spies CK (2014) Push-off needle test for traumatic triangular fibrocartilage complex lesions. J Hand Surg Am 39(7):1448–1449
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Ochman, S., Wieskötter, B., Langer, M. et al. High-resolution MRI (3T-MRI) in diagnosis of wrist pain: is diagnostic arthroscopy still necessary?. Arch Orthop Trauma Surg 137, 1443–1450 (2017). https://doi.org/10.1007/s00402-017-2747-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2747-2