Abstract
Introduction
Arthroscopic resection of dorsal wrist ganglia has become a well-accepted practice. However, there is a paucity of results on occult ganglia in the literature. The purpose of this study is to evaluate the subjective outcomes of occult dorsal wrist ganglion cysts resected arthroscopically, and to identify and examine intraarticular findings and relate them to pre-operative MRI findings and histologies.
Materials and methods
In 39 patients, 40 wrists were treated with arthroscopic resection of an occult dorsal wrist ganglion. Radio-carpal arthroscopy and mid-carpal arthroscopy were performed, and a capsular window overlying both compartments at the level of the scapholunate interval was created. The motivation to undergo operation for all patients was pain at rest and on load. In a retrospective study by telephone interview, patients were asked for pain reduction and satisfaction with the operation. 30 patients could be reached after 28.5 months on average.
Results
29 of the 30 patients were content with the operation. Reduction of pain at rest and on load was significant. MRI was performed pre-operatively in all the cases and could confirm the presence of a ganglion in 31 cases. Intraoperatively, ganglion structures were identified in 25 cases. Histology showed ganglion tissue or myxoid degeneration in 12 of 26 taken samples. Histology was positive in the cases without intraoperative visualization of typical ganglion structures and without confirmation by MRI.
Conclusion
The results of this study confirm that a high patient satisfaction can be achieved for arthroscopic treatment of occult dorsal wrist ganglia, which seem especially amenable for arthroscopic treatment. Furthermore, the results suggest that arthroscopic resection of a dorsal capsular window can be indicated if the complaints and the clinical findings are typical for dorsal wrist ganglion, even though MRI findings may be negative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since first described by Osterman and Raphael [1], arthroscopic resection of dorsal wrist ganglia has become a well-accepted practice [2–9]. As advantage over open techniques, the minimal invasive procedure with low complication rate and low post-operative morbidity, less post-operative pain, and faster recovery are discussed [2, 10–15]. The possibility to assess accompanying joint pathology is considered as another advantage [1, 16]. A lower recurrence rate, then, in open resection has been advocated by several authors, which still needs to be proven. Even though arthroscopic ganglion resection has so far shown promising results, questions remain concerning adequate identification and treatment of pathologic tissues, such as capsule, synovial tissue, and the ganglion stalk. The inconsistent identification of the so-called ganglion cyst stalk [1, 7, 9] suggests that its importance has been overrated. Most authors routinely perform a mid-carpal arthroscopy in addition to radio-carpal arthroscopy. However, the necessity of mid-carpal arthroscopy and the size and localization of the capsular window are still discussed. These questions arise especially in the treatment of occult ganglia. Geissler [12] and Slutsky and Nagle [17] pointed out that occult ganglia were particularly amenable to arthroscopic excision. However, no results are reported in the literature.
The purpose of this study is to evaluate the subjective outcomes of occult dorsal wrist ganglion cysts resected arthroscopically, and to identify and examine intraarticular findings and relate them to -pre-operative MRI findings and histologies.
Patients and methods
From 2007 to 2010, 110 arthroscopic resections of dorsal wrist ganglia were performed at our institute. Eighteen patients were excluded, because of additional interventions and non-ganglion-related symptoms. Excision of the intraosseous part of a ganglion or resection of an additional palmar ganglion, as well as open decompression of the median nerve was no exclusion criteria. From the remaining 92 ganglion resections, 40 were performed for occult ganglia in 39 patients. The definition of an occult dorsal ganglion being that it was clinically neither visible in neutral nor in flexed position of the wrist. Of the 40 patients, 26 were female and 14 male. The mean age at the time of operation was 29.3 (12–55) and median 28 years. In five patients, additional interventions were performed: one carpal tunnel release and in four patients, the intraosseous part of the ganglion in the lunate was opened and curetted under arthroscopic assistance. Four patients presented with recurrences operated elsewhere, two after open, and two after arthroscopic resection. Retrospectively in all the 40 cases, the following data from the patients’ records were collected: pre-operative diagnostics, intraoperative findings, and histology. The aim of this study was not to compare pre- and post-operative functional outcome, but to find out about efficacy of treatment. Since the patients did not have a visible ganglion, they sought treatment not with the desire to remove the ganglion, but to alleviate pain. Therefore, a telephone interview was conducted to find out about pain reduction and satisfaction with the operation. Thirty patients were available for the interview, for which written consent was obtained. Ten patients could not be reached. Patients were asked for reason for the intervention, length of pre-operative symptoms, pre- and post-operative pain on the numeric rating skala, satisfaction with the procedure, and whether they would undergo the operation again. Recurrence was suspected if the pre-operative symptoms reoccurred after a painfree interval.
Statistical analysis was performed using the SPSS software (version 18.0). Significance was set at a p value less than or equal to 0.5.
Technique
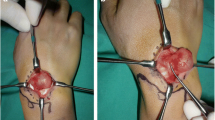
Wet arthroscopy was performed under vertical traction with Chinese finger traps. Axillary block and tourniquet were used. Two portals were used as standard access to the radio-carpal joint. A 2.4 mm arthroscope with 30° angle of vision was first placed in the 3–4 portal to examine the joint overall. Frequently, this portal does not permit clear visualization of the capsular fold at the scapholunate interval, and therefore, the arthroscope was moved to the 6-R portal. From here, a good view onto the dorsal capsule and capsular fold at the scapholunate ligament can be obtained. The exact technical details of arthroscopic ganglion resection and of arthroscopically assisted curettage of intraosseous ganglion are described elsewhere [18, 19]. Intraarticular visualization of ganglion structures was always attempted. If the radio-carpal findings were inconspicuous mid-carpal arthroscopy from the UMC portal was performed to visualize the dorsal capsule at the scapholunate interval. A capsular window of the dorsal capsule at the level of the scapholunate interval overlying both joints was created with a 2.5 mm shaver until the extensor tendons were visible. When no ganglion structures were visible, capsular thickening was a common finding. Sometimes, intraarticular emptying of the ganglion contents could be visualized on creating the capsular window. (Figure 1a–d). The arthroscopy portals were each closed by a single stitch. A soft well-padded dressing was applied and the patients were allowed to mobilize the wrist immediately, but were advised to avoid strenuous exercise for 3 weeks.
a Left wrist of a 15-year-old patient. Dry arthroscopy. View from UMC portal onto dorsal capsule at the level of the SL-interval in the upper part head of capitate, in the middle scaphoid, in the lower part lunate, and to the right thickened dorsal capsule. b Same view as in 1a, more towards the dorsal capsule. While creating the capsular window, the ganglion becomes visible within the capsular structure. c Same view as in 1b. Intraarticular emptying of the ganglion contents. d Same view as in 1b and c, in the depth of the capsular window, the ECRB-tendon is visible
Results
Clinical results
Patients reported about pre-operative complaints for a mean time of 36.2 (2–276) months. Reason for the intervention was pain for all of the 40 patients. Pain at rest was reported pre-operatively by 17 patients with 2.7 (0–8) on the numeric rating scala (NRS), which decreased to a mean of 0.3 (0–6) on the NRS post-operatively. Only three patients stayed with a mild degree of pain at rest post-operatively. All patients had pain on load at 7.4 (4–10) on the NRS pre-operatively, which decreased to 2.3 (0–8) post-operatively. Fifteen patients kept some post-operative pain on load, and 11 less then 3.5 on the NRS. The reduction in pain was statistically significant.
A pre-operative limitation of wrist mobility was reported by 22 patients. Post-operatively, four reported minor remaining limitation. Twenty patients complained of a reduction in grip strength pre-operatively which remained in four patients post-operatively. A limitation in ADL was reported by 29 patients pre-operatively, whereas only 6 had some remaining limitations post-operatively, mainly in sports activities.
When asked for remaining complaints, in general, including pain, limited wrist motion, grip strength, and reduced ADL, 8 of the questioned 30 patients reported to have some complaints. Compared with the pre-operative situation, these complaints were slightly less and unchanged each in four cases.
One patient reported to have dorsal wrist pain after a painfree interval of 13 months. In this case, recurrence has to be suspected. However, this patient was content and felt no need for reinvestigation. There was no complication. Overall, patient satisfaction was high. The operation was rated as very good by 26 patients and good by 3 patients, and 1 patient was discontent. Correspondingly, 29 of the 30 questioned patients would have the same operation again.
The one discontent patient had high pain levels pre-operatively with 7 and 10 for pain at rest and on load, reduced to post-operative 6 and 8, respectively. The pre-operative clinical presentation had been typical for dorsal ganglion, which was proven by MRI and histology. Intraoperatively, no ganglion structures but capsular thickening had been visible.
The four patients with removal of intraosseous part of the ganglion rated the operation as very good, so did three of the four patients with recurrence, one of them rated the operation as good.
There were three patients treated with typical complaints for occult ganglion, that are dorsal wrist pain on extension and flexion and tenderness over the dorsal scapholunate ligament on palpation, where no ganglion could be visualized by MRI or intraoperatively nor could it be proven by histology. Two of these patients reported to be completely painfree after the intervention, one could not be questioned. No complication occurred.
Diagnostics
When asked which movement elicitated the dorsoradial wrist pain, 24 patients found it on hyperextension and hyperflexion of the wrist, five patients on hyperextension only, and one on hyperflexion only. In all the cases, a pain on palpation of the dorsal scapholunate ligament could be elicited.
In all the cases, wrist X-rays were performed. In four cases, a radially situated lunate cyst was found and proven to be the intraosseous part of the ganglion by MRI. In all the 40 cases, an MRI was carried out pre-operatively, with the intention to confirm a ganglion and to exclude a lunate malacia. Ganglion proof was successful in 31 cases, the typical image being either a small rounded collection of liquid in the dorsal part of the scapholunate ligament or protruding from there into the joint, however, still remaining intraarticular (Fig. 2). Of the nine MRI’s without ganglion proof dorsal synovitis and capsular thickening over the scapholunate ligament was seen in six cases. Three MRI’s were considered normal.
Typical MRI finding of an occult dorsal wrist ganglion: The T2 sequence shows the ganglion as hyperintense structure. In the axial view with scaphoid (S), lunate (L), and triquetrum (T), the ganglion is situated on the scapholunate ligament within the joint capsule, below the level of the extensor tendons
Intraoperative findings
In all 40 interventions, radio- and mid-carpal portals were used. Intraoperative visualization of ganglion structures was successful in 25 cases, 13 radio-carpal, 11 mid-carpal, and one in both parts of the joint. In six cases, synovitis and capsular thickening were present over the scapholunate interval, twice radio-carpal and four times mid-carpal. In the 15 cases without visualization of ganglion structures, capsular thickening was found in five cases. Among the three cases with negative MRI and six cases where MRI showed only capsular thickening, ganglion structures were visible in five cases.
The intraoperative testing of the scapholunate ligament was inconspicuous in 36 cases, showed grade II and III laxity as described by Geissler in 2 cases each.
Histology
During 26 of the 40 interventions, tissue samples were collected from the ganglion structure or the conspicuous capsular region. In 12 cases, histology was positive with proof of ganglion structure or myxoid degeneration. Of the 26 samples, 15 were taken from visible ganglion structures, 7 of these being positive, and 5 were positive in the remaining 11 samples taken without visualization of ganglion structures.
MRI findings, intraoperative findings, histology, and patient content are shown for each case in Table 1.
Discussion
The results of this study show that arthroscopic treatment of occult dorsal wrist ganglia gives good results with high patient satisfaction, as has been described for the arthroscopic resection of visible ganglia [2–9]. The author agrees that occult ganglia are especially amenable for arthroscopic treatment, as has been suggested by Geissler [12] and Slutsky and Nagle [17]. An open approach for this intraarticular pathology does not seem adequate. As intraoperative finding thickening of the dorsal capsule overlying the scapholunate interval is a pathologic correlate if typical ganglion structures cannot be visualized. However, this does not seem to be a consistent finding. The presented results give evidence that recurrences and intraosseous ganglia can successfully be treated in this way.
The design of this study differs from the other studies on the arthroscopic treatment of dorsal wrist ganglia in performing the follow-up by telephone interview. Most studies report the patients’ motivation to undergo treatment as a mixture of aesthetic appearance, pain, and limited wrist movement [2, 4, 8]. The patients of this study group did not have a visible ganglion and sought treatment with the primary desire to alleviate pain. Therefore, a telephone interview was considered adequate to find out about pain reduction and satisfaction with the operation. The aim of this study was not to compare pre- and post-operative functional outcome, but to find out about efficacy of treatment. Of course, the retrospective questioning about pre-operative complaints has to be seen critically. However, the young patients had no problems recalling the pre-operative situation.
The study group is otherwise typical and comparable to the other publications on visible ganglia with 65 % of female patients and a mean age of 29 years. With 28.5 months, this study is among those with a rather long follow-up [3, 4, 8, 15]. A higher follow-up rate than 75 % would have been desirable.
Another limitation of this study is that the rate of recurrence can only be estimated. Only one patient had typical symptoms after a painfree interval. However, no MRI examination was initiated, since the patient was content. In the studies on arthroscopic ganglion resections, recurrence rates of 0.5 % [3] to 12.3 % [4] are described. There does not seem to be a correlation between recurrence and the intraoperative identification of a so-called ganglion stalk or ganglion structures, which has been discussed repeatedly. Edwards and Johansen [3], Chen et al. [2], and Rizzo et al. [8] identified a ganglion in 10, 13, and 29 % and have recurrence rates of 0.5, 7 and 5 %, respectively. In how far size and location of the capsular window can be related to the incidence of recurrence remains unclear.
High patient satisfaction is reported in nearly all studies on arthroscopic ganglion resection ranging from 96.5 to 100 % [2, 6, 7]. This result can be confirmed by this study with 97 % patient satisfaction, which is due to the important reduction in pain. Already in 1976, Angelides and Wallace [20] postulated that occult ganglia were more painful than visible ganglia, so did Cardinal et al. 1994 [21]. No explanation for this has been found until today.
Post-operative treatment differs in the literature. A soft dressing without immobilization as used in this study is also recommended by Nishikawa et al. [7] and Gallego and Mathoulin [4] with early physiotherapy. Most other authors prefer immobilization for 1 week and avoidance of strenuous activity for 4–6 weeks [2, 8, 12, 13].
In about 8 % (0–16.7 %) of open procedures complications, such as infection, impaired wound healing, neuroma, lesion of nerves, blood vessels, and tendons, reduction of wrist motion and grip strength are described [13, 21, 22]. Rizzo et al. [8] reported on transitional wrist stiffness in 25 % of their arthroscopically treated patients. For the arthroscopic procedure, the same risks are described as for open procedures, however, at a lower rate of 2.5 % (0–6.7 %) [2, 3, 6, 8, 13, 14]. Recent publications give evidence that the complication rate of arthroscopic procedures may have been underestimated so far [23].
Diagnosis of ganglia, may they be visible in neutral wrist position or only in the flexed wrist, is simple. X-ray of the wrist seems indicated in every case to exclude intraosseous parts of the ganglion. In occult ganglia spontaneous dorsal wrist pain, pain on load and wrist extension and flexion as well as an explicit pain on palpation of the dorsal scapholunate ligament seem typical. The authors think that in these cases, an occult ganglion should be suspected and MRI with contrast media is indicated to search for the ganglion and, at the same time, exclude avascular necrosis of the lunate. However, occult ganglia cannot be proven by MRI in every case, as shown in this study, where 31 of 40 cases had positive MRI. Cardinal could prove an occult ganglion by MRI in 11 of 14 suspected cases [21]. Vo et al. [24] reported on 10 positive MRI’s in 14 cases. In a study of Goldsmith and Yang [25], 16 of 20 cases could be proven by MRI. The remaining four cases were confirmed by operation and histology. It is plausible that the occult ganglia are not detected by MRI escaping a slice, because of their small size. This study shows that capsular thickening and synovitis localized over the scapholunate interval may be an indirect proof of an occult ganglion.
The rate of intraoperative visualization of ganglion structures of 63 % in this study compares with the reports for visible ganglions, which differ between 10 and 100 % [1–4, 6–8, 15]. The intraoperative finding of thickened capsular tissue in this study in 15 % of cases is lower than described by Edwards and Johansen [3] and Chen et al. [2] with 84 and 73 %, respectively. Kim et al. [17] also describe the capsular thickening as typical, especially in the cases, where no ganglion structures can be visualized, however, without giving numbers. There is no comment on the capsular findings by other authors.
The necessity of mid-carpal arthroscopy and the size and location of the capsular window are discussed controversially and are considered to have direct influence on the rate of recurrence. Geissler [12] performed radio-carpal arthroscopy and stressed the importance of complete resection of the dorsal capsule at the level, where it is attached to the dorsal part of the scapholunate ligament, where he created a capsular window of 1 cm2. Most authors use Geissler’s technique [4, 6, 8, 14], but describe an additional mid-carpal portal. Nishikawa et al. [7] use a radio-carpal portal and create a capsular window only when no ganglion structures can be visualized. The same procedure is described by Kang et al. [13], however, without creating a capsular window at all. Edwards and Johansen [3] and Chen et al. [2] performed radio- and mid-carpal arthroscopy, creating a capsular window as described by Geissler, the former often enlarging the window to overly the radio- and mid-carpal joint just as described by the authors of this study, the latter using an additional intrafocal cystic portal, which on critical read seems to be much of the capsular window as described by Geissler. The high rate of mid-carpal ganglion structures of 75 % reported by Gallego and Mathoulin [4] and that of mid-carpal capsular thickening in 73 % described by Edwards and Johansen [3] compare with the findings of this study with equal numbers for radio- and mid-carpal ganglion structures and suggest that it is necessary to perform mid-carpal arthroscopy, especially since complete investigation of intraarticular pathology should be aimed at [16].
Comments on the incidence of scapholunate instability in relation to arthroscopic ganglion resection in the literature are sparse and diverse. They reach from no instability [8] in 41 cases to 4 cases of grade I and II instabilities and three of grade III and IV instabilities in 64 cases [17], similar to the findings in this study. Edwards and Johansen [3] found in their series instabilities of grade I twice, grade II 22 times, grade III 20 times, and grade IV once. The differing incidence cannot be explained. Scapholunate instability has been described as consequence of resection of a dorsal wrist ganglion [26–28], hypothesizing that the scapholunate ligament was weakened by the resection. On the other hand, scapholunate pathology is considered as etiologic factor of dorsal ganglia. It can be said that the present data confirm a relation of scapholunate instability grade I and II with dorsal wrist ganglia. It can be suspected that a higher intercarpal laxity contributes to ganglion formation, but the significance of the arthroscopic findings remains unclear, since the incidence in the general population is not known. Regardless of which came first, the ganglion or the scapholunate pathology, there is an association between ganglion formation and/or ganglionectomy and scapholunate instability.
Histology is hardly mentioned in the literature and can be found only for open ganglion resection. In 1997, Osterwalder et al. [29] performed histologies in 66 of 83 operations, 74.2 % being positive. Steinberg and Kleinmann [30] had 85.7 % positive findings in 18 of 21 cases and Goldsmith and Yang [25] 80 % in 16 of 20 examined cases. In this study, tissue samples were taken during 26 of the 40 operations, 46 % being positive. In this context, the high patient satisfaction in the two cases, where ganglion structures could neither be found pre-operatively by MRI nor intraoperatively nor be proven by histology, is very interesting. It shows that given the typical clinical presentation spontaneous dorsal wrist pain can be effectively treated by a dorsal capsular window, the hypothesis being that the pain is due to an early stage of ganglion formation.
References
Osterman AL, Raphael J (1995) Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin 11:7–12
Chen AC, Lee WC, Hsu KY, Chan YS, Yan LJ, Chang CH (2010) Arthroscopic ganglionectomy through an intrafocal cystic portal for wrist ganglia. J Arthrosc Rel Surg 26:617–622
Edwards SG, Johansen JA (2009) Prospective outcomes and associations of wrist ganglion cysts resected arthroscopically. J Hand Surg Am 34:395–400
Gallego S, Mathoulin C (2010) Arthroscopic resection of dorsal wrist ganglia: 114 cases with minimum follow-up of 2 years. J Arthroscopic Rel Surg 26:1675–1682
Ho PC, Griffiths J, Lo WN, Yen CH, Hung LK (2001) Current treatment of ganglion of the wrist. Hand Surg 6:49–58
Luchetti R, Badia A, Alfarano M, Orbay J, Indriago I, Mustapha B (2000) Arthroscopic resection of dorsal wrist ganglia and treatment of recurrences. J Hand Surg Br 25:38–40
Nishikawa S, Toh S, Miura H, Arai K, Irie T (2001) Arthroscopic diagnosis and treatment of dorsal wrist ganglion. J Hand Surg Br 26:547–549
Rizzo M, Berger RA, Steinmann SP, Bishop AT (2004) Arthroscopic resection in the management of dorsal wrist ganglions: results with a minimum 2-year follow-up period. J Hand Surg Am 29:59–62
Shih JT, Hung ST, Lee HM, Tan CM (2002) Dorsal ganglion of the wrist: results of treatment by arthroscopic resection. Hand Surg 7:1–5
Chloros GD, Wiesler ER, Poehling GG (2008) Current concepts in wrist arthroscopy. Arthroscopy 24:343–354
Culp RW (1999) Complications of wrist arthroscopy. Hand Clin 15:529–535
Geissler WB (1998) Arthroscopic excision of dorsal wrist ganglia. Tech Hand Up Extrem Surg 2:196–201
Kang L, Akelman E, Weiss AP (2008) Arhroscopic versus open dorsal ganglion excision: a prospective, randomized comparison of rates of recurrence and of residual pain. J Hand Surg Am 33:471–475
Singh D, Culp RW (2002) Arthroscopic ganglionectomy. J Hand Surg Am 2:33–38
Kim JP, Seo JB, Park HG, Park YH (2013) Arthroscopic excision of dorsal wrist ganglion: factors related to recurrence and postoperative residual pain. J Arthroscopic Rel Surg 29:1019–1024
Langner I, Krueger PC, Merk HR, Ekkernkamp A, Zach A (2012) Ganglions of the wrist and associated triangular fibrocartilage lesions: a prospective study in arthroscopically-treated patients. J Hand Surg Am 37:1561–1567
Slutsky DJ, Nagle DJ (2008) Wrist arthroscopy: current concepts. J Hand Surg Am 33:1228–1244
Borisch N (2014) Arthroscopic resection of dorsal wrist ganglia. Handchir Mikrochir Plast Chir 46:307–314
Borisch N (2016) Arthroscopic resection of dorsal wrist ganglion cysts. Oper Orthop Traumatol PMID:27074739 (Epub ahead of print)
Angelides AC, Wallace PF (1976) The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg 1:228–235
Cardinal E, Buckwalter KA, Braunstein EM, Mih AD (1994) Occult dorsal carpal ganglion: comparison of US and MR imaging. Radiology 193:259–262
Hwang JJ, Goldfarb CA, Gelberman RH, Boyer MI (1999) The effect of dorsal carpal ganglion excision on scaphoid shift test. J Hand Surg Br 24:106–108
Ahsan ZS, Yao J (2012) Complications of wrist arthroscopy. Arthroscopy 28:855–859
Vo P, Wright T, Hayden F, Dell P, Chidgey L (1995) Evaluating dorsal wrist pain: MRI diagnosis of occult dorsal wrist ganglion. J Hand Surg Am 20:667–670
Goldsmith S, Yang SS (2008) Magnetic resonance imaging in the diagnosis of occult dorsal wrist ganglions. J Hand Surg E 5:595–599
Clay NR, Clement DA (1988) The treatment of dorsal wrist ganglia by radical excision. J Hand Surg Br 13:187–191
Crawford GP, Taleisnik J (1983) Rotatory subluxation of the scaphoid after excision of dorsal carpal ganglion and wrist manipulation—a case report. J Hand Surg 8:921–925
Duncan KH, Lewis RC (1988) Scapholunate instability following ganglion cyst excision. Clin Orthop 228:250–253
Osterwalder JJ, Widrig R, Stober R, Gächter A (1997) Diagnostic validity of ultrasound in patients with persistent wrist pain and suspected occult ganglion. J Hand Surg Am 22:1034–1040
Steinberg BD, Kleinman WB (1999) Occult scapholunate ganglion: a cause of dorsal radial wrist pain. J Hand Surg Am 24:225–231
Acknowledgments
I am much indebted to Corinna Linde for conducting the patient interviews and for collecting the data from the patient files.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author certifies that she has no financial or personal relationship with other people or organizations that could in appropriately bias this work. The named author declares that she has no conflicts of interest to disclose.
Funding
This research received no specific grant from any funding agency in the public, commercial, or non-profit sectors.
Rights and permissions
About this article
Cite this article
Borisch, N. Arthroscopic resection of occult dorsal wrist ganglia. Arch Orthop Trauma Surg 136, 1473–1480 (2016). https://doi.org/10.1007/s00402-016-2539-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2539-0