Abstract
In the last two decades, the number of patients with indication for diagnosis and treatment of different pathology with wrist arthroscopy has increased significantly.
The best understanding of dorsal and volar cysts physiology allowed the use of video surgery as an important therapeutic tool. We reviewed the literature on arthroscopic resection of volar wrist ganglion. The publication dates ranged from 2001 to 2012. Only one was a prospective randomized study; the authors compared the open resection and arthroscopic resection. All of the other studies were level IV of evidence. We will describe arthroscopic technique for treating volar ganglion of the wrist. Arthroscopic resection of volar wrist ganglion was performed under sedation and local anesthesia in the portal and joint. The portal sites used for the radiocarpal joint are routinely 3–4, 4–5, and 1–2. Between 2007 and 2012, we performed 31 surgeries of arthroscopic resection of volar wrist ganglion. There were 23 female and 8 male patients. The average age was 38 years. Two patients have a volar intraosseous ganglion of lunate bone. In these cases, we also used a volar radial portal.
As complications, we observed transient paresthesia of superficial radial nerve with spontaneous regression in one patient, two volar hematomas, and one recurrence.
The video surgery started to be a gold pattern in the diagnosis and treatment of intra-articular pathologies. This chapter contains video.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Ganglia are the most common soft tissue tumors of the hand [1]. They are mucin-filled cysts which may be uni- or multi-lobulated and are closely associated with either the wrist joint or tendon sheath. It is now widely accepted that dorsal and volar wrist ganglions have similar path mechanisms and arise from mucinous degeneration of the capsular and ligament structures around the joint [2, 3]. Volar wrist ganglion is the second most common mass in the wrist, arising via a pedicle from the radio scaphoid/scapholunate interval, scaphotrapezial joint, or the metacarpotrapezial joint, in that order of frequency [4]. They usually appear between the flexor carpi radialis tendon and the flexor pollicis longus tendon. Microscopically, the pedicle contains a tortuous lumen, connecting the cyst to the underlying joint [5]. The presence of this connection is supported by the intraoperative and arthrographic findings that demonstrated movement of intra-articular contrast from the radiocarpal joint into the ganglia in 85% of patients with a volar wrist ganglion. As contrast does not appear to travel from the cyst into the joint, a one-way valve mechanism has been postulated [6].
Frequently, they are benign, well characterized, and easily diagnosed.
In the last 20 years, the wrist arthroscopy has advanced, since diagnosing the therapeutic procedures in the treatment of disease in the joint. The arthroscope makes it easy to visualize the small structures and allows evaluating the locals where through open technique would be more difficult and would cause more lesions. However, it is a less invasive with less morbidity. The video surgery started to be a gold tool to diagnose and treat intra-articular pathologies.
About two decades ago, Osterman and Raphael [7] described the technique for the treatment of the dorsal carpal ganglion. In the beginning, there was a lot of skepticism with this technique; however, it has become a routine procedure. Throughout the last few years, the arthroscopic treatment of volar carpal ganglion cyst has become more popular.
Clinical Picture
The most common reason for referral is a lump that appears on the palm side of the wrist in the wrist crease just below the thumb. Some patients may be concerned about potential malignancy. Usually, the symptoms include pain in the wrist, poor activity or palpation of the mass, decreased range of motion, and decreased grip strength.
Sometimes, they may change in size over time but are usually 1–2 cm. The skin above the cyst is unchanged, and there is no associated warmth or erythema (Fig. 49.1). Sometimes occur paresthesias from compression of the ulnar or median nerves or their branches [8]. The mass itself is compressible. It will be “rubbery” in consistency and generally movable. Transillumination of a lump in the usual anatomical location will confirm a fluid-filled cyst.
Routinely a wrist X-ray evaluation is indicated to rule out preexisting osseous lesions. An ultrasound imaging study of the wrist is also examined to confirm the diagnosis, as well as to localize the ganglion (Fig. 49.2).
The MRI of soft tissue masses of the wrist is useful to differentiate them. Ulnar volar ganglions are associated with tears of triangular fibrocartilage complex. An MRI in some circumstances helps to locate the stalk, other lesions, and in the diagnosis of occult ganglia.
Revision of Literature
There is a real deficit of studies of higher methodological quality, and there is a necessity for more studies to ensure the best prediction of outcomes in wrist arthroscopy [9].
We reviewed the literature on arthroscopic resection of volar wrist ganglion [28]. The publication dates ranged from 2001 to 2012 (Table 49.1). Only one was a prospective randomized study; the authors compared the open resection and arthroscopic resection. All of the other studies were level IV of evidence [10,11,12,13,14,15,16,17]. A total of 232 wrists were submitted to an arthroscopic resection. The same operative technique described by Ho et al. [18, 19] was used by all authors. One author included an intrafocal cystic portal [13].
The mean age of patients described in eight articles was 40.45 years. All reported a major incidence in women with a female: male ratio of 3:1. Of nine articles, the follow-up ranged from 12 to 56 months with a mean of 23.82 months.
There were 14 recurrences. The recurrence rate ranged from 0% to 20% with mean of 6.03%.
There were 16 (6.89%) related complications. No connection of the complication with the ganglion was described in six wrists [18, 19]. Volar hematoma was described in three patients [20, 21]. Partial lesions of the median nerve were reported in two articles [12, 21], two lesions of a branch of the radial artery [10, 11], and neuropraxis of the superficial radial nerve [10, 13, 19]. Osterman (in the 65th Annual Meeting of the American Society for Surgery of the Hand 2010) and Langner et al. [14] did not report any complications. No patient had loss of arc range of motion.
In a study of five patients of Rocchi et al. [10], the recurrence and complications were higher for midcarpal ganglions.
Recently, Langner et al. reported that patients with volar painful ganglions of the wrist and a positive ulnocarpal stress test are highly associated with TFCC abnormalities [14].
Treatment
Indications and Contraindications
Despite a natural history of spontaneous regression [15], volar ganglion cyst of the wrist can sometimes require a surgical excision. Both surgical and nonsurgical treatments are available. Although aspiration and percutaneous sclerotherapy using 75% hypertonic glucose have been used for dorsal ganglion treatment, there isn’t report of its for volar ganglion [29]. Recent series have documented enhanced treatment success using various aspiration techniques after three separate treatments. However, recurrence rates exceeding 40% can still be expected. The most definitive management remains excision [22].
The literature with regard to recurrence rates demonstrates that open volar ganglion surgery is challenging. In principal, complete removal of the ganglion base is required to avoid recurrence. The cases of recurrence are often due to incomplete ganglion stalk resection, which is greater on the volar aspect due to the more complex volar anatomy. The risks of complication are also common, reaching rates >20% in some studies [16, 17]. The causes are proximity of the superficial palmar branch of the radial artery, the terminal branches of the superficial radial nerve, and the palmar cutaneous branch of the median nerve [10, 11]. Contraindications for arthroscopic management of volar ganglions are a history of wrist trauma with deformity, stiff joint, and advanced instability degenerative disease of the wrist.
Arthroscopic Technique
Because of the volar tilt of the distal radius, the volar capsule and ligaments of the radiocarpal joint are more accessible to arthroscopic instrumentation than the dorsal structures. Arthroscopic gangliectomy has the advantage of avoiding extensive dissection, scarring, and potential damage to structures. Other advantages are reduced postoperative pain and the time of return of function compared with open resection [11].
The results of the arthroscopic management of volar ganglions were originally presented in 2001 [23] by Ho et al. [9]. However, Ho et al. only described the detailed technique in 2003 [18].
Some surgeons perform the procedure by block anesthesia, but in general, we use sedation or local anesthesia in the portal and joint. The patient lies supine.
A tourniquet is applied to the arm and inflated after exsanguinations with an esmarch rubber.
The arm is fixed to an arm table and the elbow flexed to 90° with the wrist in vertical traction using double disposable plastic finger traps placed in the second and fourth or second and third fingers.
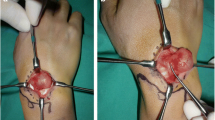
Portal sites are palpated and marked. The portal sites used for the radiocarpal joint are routinely 3–4, 4–5, and 1–2 (Fig. 49.3).
Using a syringe with a 25 × 7 mm needle, the radiocarpal joint is initially distended. Approximately, 5 ml of Bupivacaine is injected through the skin and subcutaneous tissues into the joint through 3–4 portals. We use a 40 × 8 mm needle with an outflow in portal 6U, in all cases.
Over the portals, a short skin is made, and the spreading of soft tissue with a hemostat exposes the joint capsule. This maneuver provokes extraversion of anesthetic from outside of joint. This maneuver is particularly important when the 1–2 portal is being created, to avoid injury to the radial artery and the radial nerve (Fig. 49.4).
We use a 2.4 mm arthroscope with a 30° visual angle, with irrigation fluid instilled by pump infusion.
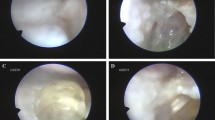
The 3–4 portals give a better view. Through the 3–4 portals, the scope allows inspection of the volar radial side wrist ligaments, where the volar ganglion usually has its stalk. Frequently, synovial and capsular abnormalities were seen at the interval between the radioscaphocapitate (RSC) and long radiolunate (LRL) ligaments or between LRL and short radiolunate (SRL) ligaments [24] (Fig. 49.5).
The 1–2 portal is also the best for instrumentation, although it has been associated with a higher risk of damaging the radial artery and sensory branch of the radial nerve [12, 21].
A 2.0- to 2.9-mm arthroscopic shaver is then introduced through 1–2 portal to deride the region. However, ganglia or their stalks cannot be observed arthroscopically in most cases. When this situation occurs, a fingertip gentle external pressure is maintained over the ganglion (Fig. 49.6). This maneuver will result in synovial and capsular bulging at the site. The shaving is performed until a hole of about 1 cm is observed in the interligamental interval. Do not use too much suction to prevent blistering and to be able to observe the mucinous liquid outlet into the radiocarpal joint (Fig. 49.7, Videos 49.1 and 49.2). Be careful that the shaver must not be advanced too anteriorly into the volar aspect of the wrist joint. A maneuver untimely could damage the important structures volar to the joint. We did not attempt to remove the ganglion wall or more of the joint capsule than was necessary to induce the gush of mucinous content. A small palmar capsulectomy defect resulted at the RSC-LRL or LRL-SRL interligamental interval after the operation, enable the flexor pollicis longus tendon can be seen, and care must be taken not to damage it with the shaver (Fig. 49.8, Videos 49.3 and 49.4).
(a) Arthroscopic image showing interligamental interval after the operation permit the flexor pollicis longus tendon can be seen. (b) Arthroscopic image showing interligamental interval after the operation permit the flexor pollicis longus tendon can be seen. (c) Arthroscopic image showing interligamental interval after the operation permit the flexor pollicis longus tendon can be seen
Sometimes, we can see the mucinous liquid leakage through the portal and running down in the skin (Fig. 49.9).
The shaver was also used for trimming capsular lesion, partial tear of the scapholunate ligament, lunotriquetral ligament, volar radioscaphocapitate ligament, and triangular fibrocartilage complex (TFCC).
The ganglions that arise from the distal wrist crease are likely to originate in the scaphotrapezium-trapezoid (STT) joint or other component of the midcarpal joint (Fig. 49.10). In these situations, a finger trap applied an extra-distraction on thumb. Two extra portals are performed. The first, the radial midcarpal portal (RMC), which is located 1 cm distal to the 3–4 portals and in line with the radial margin of the third metacarpal, is performed. The second, the STT portal, is located just to the ulnar side of the extensor pollicis longus tendon, at the level of the articular surface on the distal pole of the scaphoid (Fig. 49.11). The ganglia resection is difficult because of the narrow space. Two cases of arthroscopic resection of scaphotrapeziotrapezoidal (STT) joint ganglia utilizing the STT-U and STT-R portals were described with no recurence observed after 50 months of follow-up [30].
In 2012, Yamamoto et al. reported sonography-assisted arthroscopy. With this technique, they can identify ganglia, vessels, nerves, tendons, and the blade shavers can be identified and guided to the lesion. The advantage is to avoid vascular, nerve, and tendon injuries. Unfortunately, they did not report the number of patients and if they have less complications [25].
Chen et al. [13] described a volar ganglia resection through an intrafocal cystic portal. They performed an additional puncture wound with guidance from the light source of the arthroscopy, which was introduced through the 3–4 portals, over the ganglion cyst, followed by a gentle introduction of the oscillating shaver. The objective is to remove all the residual ganglionic tissue, as well as the connecting stalk. In our opinion, because of the proximity of median nerve and radial artery, this is a very dangerous procedure.
In all cases, the tourniquet is deflated before ending the intervention to check for any potential vascular injury.
During the procedure, if a TFCC lesion is identified, this will be graded according to the Palmer classification [26] and the treatment will be made according to what can be found in another specific chapter in this book.
At completion of the procedure, single stitches are made to close the portal sites, and the wrist is protected with a bandaging. Patients are advised to move their wrists when the pain permits. The stitches are removed within 1 week. Sports and heavy manual activity should be avoided for 3 months.
Our Experience
Between 2007 and 2012, we performed 31 surgeries of arthroscopic resection of volar wrist ganglion. There were 23 female and 8 male patients. The average age was 38 years. Two patients have a volar intra-osseous ganglion of lunate bone. In these cases, we also used a volar radial portal.
As complications, we observed transient paresthesia of superficial radial nerve with spontaneous regression in one patient, two volar hematomas, and one recurrence. We used the Allen test in postoperative period and we did not observe failure of blood to diffuse into the hand.
One patient had a volar radiocarpal ganglion confirmed by ultrasound testing, but the procedure was converted to open surgery because the mass was a lipoma.
We never used a needle passing through the ganglion into the joint to identify the interval between the ligaments because of the proximity of the radial artery.
We insert the scope through the 3–4 portals for inspection of the stalk. Therefore, the scope is changed to be introduced through an additional 4–5 portals and volar ganglion was debrided through the radioscaphocapitate (RSC) ligament and long radiolunate (LRL) ligament using a resector inserted from the 3–4 portals. The 1–2 portal is created only when we cannot remove the ganglion through 3–4 and 4–5 portals.
Because of the proximity of the gates 3–4 and 1–2 can have difficulties performing the triangulation technique with optical and blade shaver in the first procedures.
Sometimes, we introduce a Kelly clamp inside the wrist through the 3–4 portals until the palmar capsular defects. The clamp is open and we can observe the mucinous fluid entering inside of the radiocarpal joint.
After the end of procedure, fragments of synovial tissues were collected on the occasion of an endoscopic procedure and were sent to histologic study with the purpose of proving the resection of the ganglion. Our good results were confirmed by others authors that concluded the athroscopic resection is a safe and useful technique [31].
Postoperative Rehabilitation
At completion of the procedure, single stitches are made to close the portal sites, and the wrist was protected with a bandaging.
Patients are advised to move their wrists when the pain permits. The stitches are removed within 1–2 weeks. If the patient shows stiffness or swelling during this time, a therapy program should be started. Heavy manual activity should be avoided for 2 months.
Complications
Wrist arthroscopy is a fairly safe procedure with a low rate of complications. The main complication would be recurrence. One pseudoaneurysm of radial artery was described in a patient with history of hemophilia [32]. Other complications described in the literature [27] include wrist stiffness, cartilage injury, thermal burn, reflex sympathetic dystrophy, infection, tendon, nerve, and vessel injury.
References
Nelson CL, Sawmiller S, Phalen GS. Ganglions of the wrist and hand. J Bone Joint Surg. 1972;54(7):1459–64.
Angelides AC. Ganglions of the hand and wrist. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green’s operative hand surgery. 4th ed. New York: Churchill Livingstone; 1999. p. 2171–83.
Watson HK, Rogers WD, Ashmead D IV. Reevaluation of the cause of the wrist ganglion. J Hand Surg Am. 1989;14:812–7.
Greendyke SD, Wilson M, Shepler TR. Anterior wrist ganglia from the scaphotrapezial joint. J Hand Surg Am. 1992;17(3):487–90.
Tophoj K, Henriques U. Ganglion of the wrist—a structure developed from the joint. Acta Orthop Scand. 1971;42(3):244–50.
Andren L, Eiken O. Arthrographic studies of wrist ganglions. J Bone Joint Surg Am. 1971;53(2):299–302.
Osterman AL, Raphael J. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin. 1995;11:7–12.
Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999;7(4):231–8.
Fernandes CH, Meirelles LM, Raduan Neto J, Santos JBG, Faloppa F, Albertoni WM. Characteristics of global publications about wrist arthroscopy: a bibliometric analysis. Hand Surg. 2012;17(3):311–5.
Rocchi L, Canal R, Pelaez J, et al. Results and complications in dorsal and volar wrist ganglia arthroscopic resection. Hand Surg. 2006;11:21–61.
Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg. 2008;42:253–9.
Rhyou I, Kim HJ, Suh BG, Chung C, Kim KC. Arthroscopic resection of volar ganglion of the wrist joint. J Korean Soc Surg Hand. 2010;15(3):136–42.
Chen ACY, Lee WC, Hsu KY, Chan YS, Yuan LJ, Chang CH. Arthroscopic ganglionectomy through an intrafocal cystic portal for wrist ganglia. Arthroscopy. 2010;26(5):617–22.
Langner I, Krueger PC, Merk HR, Ekkernkamp A, Zach A. Ganglions of the wrist and associated triangular fibrocartilage lesions: a prospective study in arthroscopically-treated patients. J Hand Surg Am. 2012;37:1561–7.
Rosson JW, Walker G. The natural history of ganglia in children. J Bone Joint Surg. 1989;71(4):707–8.
Jacobs LGH, Govaers KHM. The volar wrist ganglion: just a simple cyst? J Hand Surg Br. 1990;15(3):342–6.
Dias J, Buch K. Palmar wrist ganglion: does intervention improve outcome? A prospective study of natural history and patient reported treatment outcomes. J Hand Surg Br. 2003;28:172–6.
Ho PC, Lo WN, Hung LK. Arthroscopic resection of volar ganglion of the wrist: a new technique. Arthroscopy. 2003;19(2):218–22.
Ho PC, Law BKY, Hung LK. Arthroscopic volar wrist ganglionectomy. Chir Main. 2006;25:221–30.
Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg. 2004;9(2):159–64.
Mathoulin C, Massarella M. Therapeutic interest of wrist arthroscopy about 1000 cases. Chir Main. 2006;25:145–60.
Chung KC, Murray PM. Hand surgery update V. Rosemont: American Society for Surgery of the Hand; 2011. p. 791.
Ho PC, Griffiths J, Lo WN, Yen CH, Hung LK. Current treatment of ganglion of the wrist. Hand Surg. 2001;6(1):49–58.
Mathoulin C. Resection of volar ganglia. In: Geissler WB, editor. Wrist arthroscopy, vol. 215. New York: Springer; 2005. p. 182–4.
Yamamoto M, Kurimoto S, Okui N, Tatebe M, Shinohara T, Hirata H. Sonography-assisted arthroscopic resection of volar wrist ganglia: a new technique. Arthrosc Tech. 2012;1(1):31–5.
Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594–606.
Wolfe SW, Pederson WC, Hotchkiss RN, Kozin SH. Wrist arthroscopy. In: Green’s operative hand surgery. 6th ed. Philadelphia: Churchill Livingstone; 2010. p. 738–9.
Fernandes CH, Miranda CD, Dos Santos JB, Faloppa F. A systematic review of complications and recurrence rate of arthroscopic resection of volar wrist ganglion. Hand Surg. 2014;19(3):475–80.
Pires FA, Santos JBGD, Fernandes CH, Nakashima LR, Faloppa F. Sclerotherapy With 75% Hypertonic Glucose to Treat Dorsal Synovial Cysts of The Wrist. Acta Ortop Bras. 2021 Mar-Apr;29(2):101–04.
Ho LC, Cabello ÁP, Wai PFY, Pak CH, (2020) Arthroscopic Resection of Wrist Scaphotrapeziotrapezoidal (STT) Joint Ganglia. Journal of Wrist Surgery 09 (05):440–45 .
Oliveira RK, Brunelli JPF, Bayer LR, Aita M, Mantovani G, Delgado PJ, (2019) Artrhoscopic Resection of Volar Wrist Ganglion: Surgical Technique and Case Series. Revista Brasileira de Ortopedia 54 (06):721–30.
C. Clerico, M. Benatar, C. Dumontier, (2014) Radial artery pseudoaneurysm: A rare complication after arthroscopic treatment of a volar wrist ganglion in a hemophilia patient. Chirurgie de la Main 33 (5):361–63.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Electronic Supplementary Material
Arthroscopic video showing mucinous liquid outlet into the radiocarpal joint (MP4 34996 kb)
Arthroscopic video showing mucinous liquid outlet into the radiocarpal join (MP4 2656 kb)
Arthroscopic video showing interligamental interval during the operation permit the flexor pollicis longus tendon can be seen (MP4 13939 kb)
Arthroscopic video showing interligamental interval during the operation permit the flexor pollicis longus tendon can be seen (MP4 5963 kb)
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fernandes, C.H., Miranda, C.D.O. (2022). Arthroscopic Management of Volar Ganglions. In: Geissler, W.B. (eds) Wrist and Elbow Arthroscopy with Selected Open Procedures. Springer, Cham. https://doi.org/10.1007/978-3-030-78881-0_49
Download citation
DOI: https://doi.org/10.1007/978-3-030-78881-0_49
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78880-3
Online ISBN: 978-3-030-78881-0
eBook Packages: MedicineMedicine (R0)