Abstract
Purpose We analyzed anterior cruciate ligament reconstruction (ACLR) patients in order to evaluate degenerative changes and the effect of meniscal insufficiency at mid-term follow-up.
Methods
Sixty subjects (40 patients at 5.9 years after ACLR, 20 healthy controls) underwent 3T MRI. Quantitative cartilage T2 mapping and morphological Whole Organ Magnetic Resonance Imaging Score (WORMS) evaluation were performed. Self-reported questionnaires were used for subjective clinical evaluation. Based on the meniscal status at ACLR, further subdivision within each compartment (lateral and medial) was made: menisci intact and menisci insufficient.
Results
The ACLR subjects showed significantly elevated T2 values and higher WORMS scores compared to the control group. T2 values of the anterior lateral femoral subcompartment were significantly higher in menisci insufficient group compared to the control group. In both compartments significantly higher WORMS scores were observed in the menisci insufficient group compared to the menisci intact group.
Conclusions
ACLR knees exhibit cartilage matrix and morphological degeneration at mid-term follow-up. Lateral meniscal insufficiency noted at ACLR presents a higher risk of developing degenerative changes than does the medial meniscus insufficiency; however, this difference may not be detected clinically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament (ACL) is an important stabilizer and loss of its function leads to knee instability [1]. Untreated instability may cause further articular injury and may lead to early osteoarthritis (OA), therefore anterior cruciate ligament reconstruction (ACLR) is often recommended [1]. The main goal of ACLR is to restore function and stability, allowing the patient to return to normal activities [2]. Although ACLR restores knee stability, 50–70 % of ACLR patients develop radiological changes of OA at 10–15 years after ACL rupture [1]. This suggests multifactorial etiology of OA in ACLR patients [3].
ACL rupture is a knee injury involving strong compressive forces and is frequently associated with damage to other joint structures [4]. Especially association of ACL injury and meniscus tears has been well established [5]. Recent studies have focused on quantitative cartilage evaluation after ACLR [6–9].
The objective of this study was to evaluate cartilage matrix and morphological degeneration at mid-term follow-up in ACLR knees. Moreover, a longitudinal effect of menisci status at ACLR was studied in order to evaluate its effect on degenerative changes. The primary hypothesis was that ACLR knees would exhibit more degenerative changes than healthy controls and the secondary hypothesis was that meniscal insufficiency is an important risk factor in the development of degenerative changes.
Materials and methods
Subjects
The National Medical Ethics Committee approved the study (date of issue: 19.8.2014, registration number: 135/08/14) and informed consent was obtained from the subjects after the nature of the study had been fully explained. Forty ACLR patients (26 males) and twenty healthy volunteers (11 males) were recruited for the study (Table 1). The inclusion criteria for the ACLR group were (1) 16–45 years at ACLR; (2) body mass index (BMI) of 18.5–30; (3) preoperative sports activity of at least 4 on Tegner scale. Exclusion criteria were (1) concomitant collateral ligament disruption, (2) concomitant posterior cruciate ligament injury, (3) MR contraindication and (4) total meniscectomy. The healthy control subjects were matched to the ACLR group according to age, sex, BMI and level of sports activity (Table 1). The inclusion criteria for the control group were (1) IKDC score of at least 95 and (2) no history indicative of any knee joint disorder.
Surgically treated subjects were invited from the 3-year period (years 2008–2010). Twenty-three subjects underwent transtibial and seventeen underwent anteromedial portal ACLR. ACLR procedures were performed by two senior orthopedic surgeons with the same perioperative procedure and same graft type (semitendinosus-gracilis tendon graft), all patients underwent same rehabilitation program. Average time from the ACL injury to the ACLR was 2.1 ± 2.5 years.
Subjective clinical evaluation
Following questionnaires were presented to the study subjects at the MR examination; Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee Subjective Knee Form (IKDC), Lysholm, Tegner scale and RAND-36 Health Survey [10–14].
Imaging Studies
Preoperative knee radiographs
In the ACLR group, we determined the degree of preoperative OA based on the Kellgren-Lawrence grading system on anteroposterior and lateral radiographs taken at the time of ACLR [15].
MR protocol
MR examinations were performed as a single time intervals capture by using a 3.0 T imager (Magnetom® Trio, Siemens, Erlangen, Germany) with an 8-channel transmit-receive knee coil (Invivo, Gainesville, Florida, USA). To minimize the changes of different loading conditions, subjects were instructed to avoid sport activities 1 day prior the MR examination and were scanned after resting at least half an hour. Imaging protocol included proton density (PD) turbo spin echo (TSE) fat saturation (FS) images in the sagittal plane (2230/29 [TR ms/TE ms], 16 cm field of view [FOV], 3 mm/1 mm [slice thickness/interslice gap], 512 × 512 matrix, 120° flip angle [FA], 2 signals acquired) and in the coronal plane (2540/35 [TR ms/TE ms], 15 cm FOV, 3 mm/1 mm [slice thickness/interslice gap], 384 × 384 matrix, 150° FA, 2 signals acquired). PD TSE images were obtained in the sagittal plane (2000/29 [TR msec/TE ms], 16 cm FOV, 3 mm/1 mm [slice thickness/interslice gap], 512 × 512 matrix, 120° FA, 2 signals acquired) and in the axial plane (2230/29 [TR ms/TE ms], 15 cm FOV, 3 mm/1 mm [slice thickness/interslice gap], 512 × 512 matrix, 140° FA, 2 signals acquired). T2 maps were obtained in the sagittal plane (1000/13.8; 27.6; 41.4; 55.2; 69.0; 82.8 [TR ms/TE ms], 16 cm FOV, 3 mm/1 mm [slice thickness/interslice gap], 384 × 384 matrix, 180° FA, 1 signal acquired). Average time from the ACLR to the MR examination was 5.9 ± 0.8 years.
Quantitative cartilage evaluation
T2 maps were derived using processing package (MapIt, Siemens Medical Solutions, Erlangen, Germany). Image analysis was performed with a Leonardo® workstation (Siemens Medical Solutions, Erlangen, Germany).
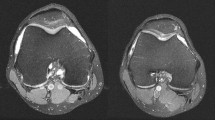
Knee joint cartilage was manually segmented in accordance with previously reported papers and five compartments were defined: lateral femoral, medial femoral, lateral tibial, medial tibial and patella [7, 8]. These were subdivided into subcompartments with regard to the menisci in a fashion of the regional subdivision used in WORMS (Fig. 1) [16]. Patella was subdivided in the superior and inferior pole. In each subcompartment the zonal (deep zone—adjacent to the subchondral bone; superficial zone—adjacent to the articular surface) T2 values were obtained by undertaking an ROI (Range Of Interest) analysis [8]. Each ROI was manually defined with multiple marker points on two consecutive midsagittal slices in each compartment. The T2 value of each ROI (mean 172 pixels; range 47–573) was expressed as the mean value of two consecutive slices measurements.
Sagittal T2 map showing the division of the lateral (a) and medial (b) compartment into subcompartments. sP superior patella, iP inferior patella, aLF anterior lateral femoral, cLF central lateral femoral, pLF posterior lateral femoral, aLT anterior lateral tibial, cLT central lateral tibial, pLT posterior lateral tibial, cMF central medial femoral, pMF posterior medial femoral, aMT anterior medial tibial, cMT central medial tibial, pMT posterior medial tibial
Semi-quantitative MR assessment
Whole Organ Magnetic Resonance Imaging Score (WORMS) system was used in the assessment of morphologic degeneration. The final WORMS scores were tabulated and graded in accordance with the paper published by Peterfy et al. [16].
Assessment of the menisci
To evaluate the effect of the meniscal injury at the time of ACLR we have reviewed the arthroscopy records of the patients. Within the medial and lateral compartment we have divided patients according to the meniscal status in two groups: menisci intact and menisci insufficient. In the menisci insufficient group all patents with signs of meniscal injury were included despite the lesion location and the following treatment. In both compartments the groups did not differ significantly in age, follow-up time, BMI at ACLR and BMI at MR examination.
Statistical analysis
Unpaired t test was used to compare continuous and Mann–Whitney U test was used to compare categorical variables between two groups. Analysis of variance (ANOVA) was used to assess meniscal status inter-group cartilage T2 values. Post hoc comparisons were made with Bonferroni correction. Pearson correlation coefficient was calculated to evaluate correlation. Significance was set at P < 0.05. Statistical analysis was performed with SPSS v.17.0 (SPSS Inc., Chicago, Illinois, USA).
Results
Preoperative radiographs
Nine patients showed radiographic signs of OA. In transtibial group four patients were assigned grade 1, in anteromedial portal group four patients were assigned grade 1 and one patient was assigned grade 2.
Transtibial vs. anteromedial portal technique
No significant differences in preoperative OA were observed between patients undergoing different ACLR technique. Furthermore, at mid-term follow-up no significant differences in subjective clinical evaluation or degeneration changes were observed between these two groups of patients.
ACLR group vs. control group
Subjective clinical evaluation
Control group showed significantly higher scores than the ACLR group in the knee-specific instruments and RAND-36 items (Table 1).
Semi-quantitative MR assessment
In the control group 14 subjects showed no abnormalities, hence had a total combined WORMS score of 0. However, only two subjects in the ACLR groups showed no abnormalities. Table 2 shows WORMS scores of the ACLR group versus control group.
Quantitative cartilage evaluation
The ACLR group showed significantly elevated T2 values compared to the control group in four subcompartments (Fig. 2).
Cartilage MR relaxation time quantification of the ACLR group versus control group. ACLR anterior cruciate ligament reconstruction, aLF anterior lateral femoral subcompartment, pLF posterior lateral femoral subcompartment, pMF posterior medial femoral subcompartment, cMT central medial tibial subompartment, sup. superficial
Meniscal status subdivision and inter-group comparison
Subjective clinical evaluation
In both compartments (lateral and medial) no significant differences were found between the menisci insufficient and menisci intact group.
Semi-quantitative MR assessment
23 patients showed meniscal lesions at the time of the ACLR. 16 patients showed medial meniscus lesions, 9 patients showed lateral meniscus lesions and 2 patients showed lesions in both menisci. Table 3 shows subdivision of patients according to the specific compartment meniscal status at ACLR and WORMS scores.
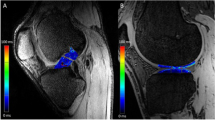
Quantitative cartilage evaluation
In 4 subcompartments significant differences were observed when dividing groups according to the meniscal status. Figure 3 shows cartilage T2 values according to the meniscal status in the lateral and medial compartment.
Cartilage MR relaxation time quantification according to meniscal status a in the lateral femorotibial joint (LFTJ) and b in the medial femorotibial joint (MFTJ). aLF anterior lateral femoral subcompartment, pLF posterior lateral femoral subcompartment, pMF posterior medial femoral subcompartment, cMT central medial tibial subompartment, sup. superficial, asterisk significant at P < 0.05
Correlations
No significant correlations were observed between demographic characteristics (age and BMI) and degenerative changes or between subjective clinical evaluation and degenerative changes. In the ACLR group T2 values of only one subcompartment showed significant correlations with WORMS: deep and superficial zone of the anterior lateral femoral subcompartment showed significant correlation with lateral compartment cartilage, lateral and patellofemoral compartment total, and total combined WORMS score.
Discussion
In this study a quantitative and semi-quantitative evaluation of the ACLR knees was employed to characterize degenerative changes and to evaluate the effect of meniscal lesions at mid-term follow-up.
The focus of most papers evaluating knee cartilage in ACLR patients has been on the early postoperative cartilage matrix changes [7–9, 17]. Only one study reported a follow-up with 11 years after ACL injury; however, T2 mapping sequences were limited to the lateral compartment at the site of initial bone bruise [5]. In our study cartilage evaluation of all 3 compartments was performed with the time from the ACLR of 5.9 years. With longer follow-up time we proposed the differences between ACLR patients and controls would be more pronounced than in the previous papers, since a process of cartilage degeneration is accelerated at 5–7 years after ACL injury [5]. Most of the previous studies have shown prolongation of the cartilage relaxation time over the follow-up time after ACLR [5, 18, 19]. In our study cartilage relaxation time prolongation was observed in four subcompartments. Interestingly, the anterior lateral femoral subcompartment was the only subcompartment in our study in which higher T2 values were associated with meniscal status. This is consistent with a previous study that found significantly elevated T 1ρ values in the anterior lateral femoral subcompartment in patients with associated lateral meniscal tears compared to the respective regions in the contralateral knee [8].
In primary OA morphological degeneration is seen predominantly in the medial compartment; however, in ACLR patients equal distribution between both femorotibial compartments is observed [20]. Injury mechanism has been proposed as the underlying cause for this, since ACL rupture predominantly inflicts trauma in the lateral compartment [20]. Similar observation has been made in our study with ACLR group showing equal distribution of morphological degeneration changes between compartments. However, when the ACLR group was sub-analyzed according to the meniscal status at ACLR significant differences were observed between compartments. In the lateral compartment significantly higher scores in WORMS features of cartilage, osteophytes, total compartment and total WORMS were observed in menisci insufficient group compared to menisci intact group. However, this was not the case in the medial compartment, where menisci insufficient group showed significantly higher scores in only one WORMS feature—osteophytes. It is well established that meniscus insufficiency increases the risk of knee OA both in isolation and in combination with an ACL rupture [3]. However, the results of our study suggest that lateral meniscus insufficiency in ACLR patients presents higher risk of developing morphological degeneration than does the medial meniscus insufficiency.
Despite the differences in WORMS scores between the menisci intact and menisci insufficient group, no such differences were found for subjective clinical evaluation and cartilage relaxation time. Similarly Li et al. reported no significant differences in clinical evaluation between subjects with intact and insufficient menisci [17]. Observation for the cartilage relaxation time is in agreement with the study by Hirose et al.; however, other studies reported longer cartilage relaxation times in patients with insufficient menisci than in patients with intact menisci [6, 17, 19]. Moreover, we found no correlation between WORMS menisci score and cartilage relaxation times, a finding that is consistent with previous studies [17, 18]. Studies report good correlation between T2 values and WORMS in OA knees; however, in our study this finding was observed only in the anterior lateral femoral subcompartment [21].
There are few limitations to the study. Firstly, only preoperative radiographs were obtained; thus, direct longitudinal MR evaluation of degeneration changes could not have been performed. Secondly, the arthroscopic records were reviewed retrospectively and more attentive arthroscopic exploration may have been undertaken in prospective study. The incidence of medial meniscus tears at the time of ACLR rupture varies from 25 to 45 %; and for the lateral meniscus from 31 to 62 % [5]. Similar rate for the medial meniscus was observed in our study; however, lower rate was observed for the lateral meniscus than in the previous studies. The lower rate may have been attributed to the fact that the arthroscopic records were reviewed retrospectively; however, good association between meniscal status at ACLR and WORMS menisci score was observed in both compartments, which suggests accuracy of arthroscopic records. Thirdly, clinical evaluation with only self-reported questionnaires was performed without objective clinical evaluation or evaluation of clinical knee laxity. Finally, the range of time between ACL injury and ACLR is quite large and both chronic and acute ACLR were included in the study.
In conclusion, the present study showed cartilage matrix and morphological degeneration of ACLR knees at mid-term follow-up. Meniscal lesions noted at ACLR contribute to morphologic degeneration with lateral meniscus insufficiency presenting a higher risk of cartilage matrix and morphologic degeneration than does the medial meniscus insufficiency.
References
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36(7):1275–1282. doi:10.1177/0363546508314721
Ichiba A, Kishimoto I (2009) Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg 129(3):409–415. doi:10.1007/s00402-008-0786-4
Øiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37(7):1434–1443. doi:10.1177/0363546509338827
Bolbos RI, Link TM, Ma CB, Majumdar S, Li X (2009) T1rho relaxation time of the meniscus and its relationship with T1rho of adjacent cartilage in knees with acute ACL injuries at 3 T. Osteoarthr Cartil 17(1):12–18. doi:10.1016/j.joca.2008.05.016
Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S (2012) Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med 40(2):276–285. doi:10.1177/0363546511423380
Chu CR, Williams AA, West RV, Qian Y, Fu FH, Do BH, Bruno S (2014) Quantitative magnetic resonance imaging UTE-T2* mapping of cartilage and meniscus healing after anatomic anterior cruciate ligament reconstruction. Am J Sports Med 42(8):1847–1856. doi:10.1177/0363546514532227
Su F, Hilton JF, Nardo L, Wu S, Liang F, Link TM, Ma CB, Li X (2013) Cartilage morphology and T1ρ and T2 quantification in ACL-reconstructed knees: a 2-year follow-up. Osteoarthritis Cartilage 21(8):1058–1067. doi:10.1016/j.joca.2013.05.010
Theologis AA, Haughom B, Liang F, Zhang Y, Majumdar S, Link TM, Ma CB, Li X (2014) Comparison of T1rho relaxation times between ACL-reconstructed knees and contralateral uninjured knees. Knee Surg Sports Traumatol Arthrosc 22(2):298–307. doi:10.1007/s00167-013-2397-z
Bae JH, Hosseini A, Wang Y, Torriani M, Gill TJ, Grodzinsky AJ, Li G (2015) Articular cartilage of the knee 3 years after ACL reconstruction. Acta Orthop 86(5):605–610. doi:10.3109/17453674.2015
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Hays RD, Sherbourne CD, Mazel RM (1993) The RAND 36-Item health survey 1.0. Health Econ 2(3):217–227
Demirdjian AM, Petrie SG, Guanche CA, Thomas KA (1998) The outcomes of two knee scoring questionnaires in a normal population. Am J Sports Med 26(1):46–51
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29(5):600–601
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16(4):494–502
Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, Kothari M, Lu Y, Fye K, Zhao S, Genant HK (2004) Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage 12(3):177–190. doi:10.1016/j.joca.2003.11.003
Li H, Chen S, Tao H, Chen S (2015) Quantitative MRI T2 relaxation time evaluation of knee cartilage: comparison of meniscus-intact and -injured knees after anterior cruciate ligament reconstruction. Am J Sports Med 43(4):865–872. doi:10.1177/0363546514564151
Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, Ma CB, Majumdar S (2011) Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1{rho} and T2-initial experience with 1-year follow-up. Radiology 258(2):505–514. doi:10.1148/radiol.10101006
Hirose J, Nishioka H, Okamoto N, Oniki Y, Nakamura E, Yamashita Y, Usuku K, Mizuta H (2013) Articular cartilage lesions increase early cartilage degeneration in knees treated by anterior cruciate ligament reconstruction: T1ρ mapping evaluation and 1-year follow-up. Am J Sports Med 41(10):2353–2361. doi:10.1177/0363546513496048
Swärd P, Kostogiannis I, Neuman P, Von Porat A, Boegård T, Roos H (2010) Differences in the radiological characteristics between post-traumatic and non-traumatic knee osteoarthritis. Scand J Med Sci Sports 20(5):731–739. doi:10.1111/j.1600-0838.2009.01000.x
Joseph GB, Baum T, Carballido-Gamio J, Nardo L, Virayavanich W, Alizai H, Lynch JA, McCulloch CE, Majumdar S, Link TM (2011) Texture analysis of cartilage T2 maps: individuals with risk factors for OA have higher and more heterogeneous knee cartilage MR T2 compared to normal controls–data from the osteoarthritis initiative. Arthritis Res Ther 13(5):R153. doi:10.1186/ar3469
Acknowledgment
We acknowledge radiological technicians at our institution for direct technical assistance, including help with patients and equipment. We acknowledge M. Števanac for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Snoj, Ž., Zupanc, O. & Salapura, V. Retrospective quantitative cartilage and semi-quantitative morphological evaluation at 6 years after ACL reconstruction. Arch Orthop Trauma Surg 136, 967–974 (2016). https://doi.org/10.1007/s00402-016-2463-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2463-3