Abstract
Femoroacetabular impingement (FAI) has been suggested as a major cause of primary hip osteoarthritis (PHOA). We assessed the prevalence of FAI detected radiographically in a cohort that underwent total hip replacement (THR) for PHOA. Two radiologists independently assessed the retrospective preoperative radiographs (AP pelvis and lateral) of 82 subjects <55 years of age scheduled for THR. Subjects were categorized as: definite FAI, no FAI, and not possible to exclude FAI. Definite FAI was present in 36 % of subjects. FAI is common in young subjects undergoing THR for PHOA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) has been proposed as a common cause of hip pain in young adults and an important cause of primary hip osteoarthritis (PHOA). The pathomechanical process is consequent to subtle deformities of the hip joint, leading to repeated abnormal bony contact and a sequence of articular damage, pain, and ultimately radiographic OA [1, 2].
Current literature describes two main types of FAI: cam and pincer-type impingement. Cam impingement is characterized by a bony prominence at the femoral head–neck junction. With hip flexion or internal rotation, the cam lesion is forced against the acetabular rim, potentially leading to cartilage avulsion and damage [3, 4] (Fig. 1a). In contrast, pincer impingement involves acetabular overcoverage of the femoral head. Impingement occurs at the limit of hip movement as the femoral head is forced against the protruding acetabulum, leading to circumferential labral injury and cartilage damage [2–4] (Fig. 1b). Cam impingement is more commonly found in younger athletic males, while pincer impingement occurs typically in middle-aged females [3, 5]. Often, patients present with features of both impingement types [6].
a Cam impingement; b pincer impingement. Reproduced with permission from Stafford and Witt [4]. The anatomy, diagnosis, and pathology of femoroacetabular impingement
FAI has been reported mainly in the orthopedic, rehabilitation, and sports medicine literature with limited reporting in rheumatology journals [7]. The clinical findings include groin pain associated with hip rotation, sitting position, or sports activities or limited range of motion [6]. On physical examination, a positive “impingement test” reproduces the groin pain when the hip is flexed to 90 ° with internal rotation and adduction [6]. Although most orthopedic centers in North America and Europe offer surgical options for FAI to address hip pain [8], there are limited data on the epidemiology of FAI. We have assessed the prevalence of FAI in a young cohort that underwent total hip replacement (THR) for PHOA.
Materials and methods
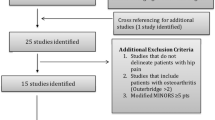
This retrospective study, approved by the University of British Columbia Clinical Research Ethics Board, used a Joint Replacement Service database to identify subjects aged <55 years, who received a THR between January 2007 and December 2008 for PHOA. Exclusion criteria included hip infection, rheumatoid arthritis, fracture, congenital/developmental hip dysplasia, and other causes of secondary hip OA.
Preoperative radiographs (AP pelvis and lateral views) closest in time to the THR were retrieved for each subject. Two radiologists assessed radiographs using a scoring tool based on a literature review [6, 9–11] (Tables 1 and 2). Each subject was categorized into one of three groups: definite FAI, no FAI, or not possible to exclude FAI. The latter group included subjects in whom the degenerative changes made it difficult to discern radiographic features of FAI. In cases of definite FAI, subjects were further categorized as having cam, pincer, or mixed-type impingement. Interobserver variability was resolved by consensus. Univariate statistical analysis was performed.
Results
Overall 470 THR cases were identified and assigned a numeric identifier (ID) using a random number generator; 82 subjects were then selected from a ranked list of these randomly assigned IDs. Seven of the 82 subjects were excluded due to the lack of preoperative radiographs (N = 3), duplication (N = 3), suspected secondary OA (N = 2), or poor quality radiographs (N = 1). Of 75 subjects, 49 (65 %) were male. The mean age was 49.5 ± 4.7 years. Preoperative AP radiographs were available for all 75 subjects, but only 52 subjects (69 %) had lateral films available.
Definite FAI was present in 27 (36 %) subjects and no FAI in 25 (33 %) subjects. In 23 (31 %) subjects, FAI could not be excluded due to advanced osteoarthritis. Thus, of those that could be adjudicated clearly, 27 of 52 (52 %) had FAI and 25 of 52 (48 %) did not. Of the 27 subjects with FAI, 5 cam-type-, 13 pincer-type-, and 9 mixed-type cases were identified. There was a male predominance in cam-type features (70 % males vs. 0 % females) and a female predominance in pincer-type features (100 % of females vs. 75 % of males).
Discussion
Results of this study of younger adults who underwent THR suggest that FAI is common in this patient group. These findings add to the limited epidemiologic data available on the burden of FAI. The prevalence rates reported to date span a wide range, reflecting differences in the populations sampled, imaging modality used, and the criteria used to define FAI [5, 12–14].
Ochoa et al. [15] studied subjects (mean age 32 years) who presented to an army medical center with hip-related complaints. At least one radiographic FAI finding was present for 135 of 155 subjects (87 %), with radiographic signs of FAI including herniation pits, pistol grip deformity, center-edge angle, alpha angle, and crossover sign. Unlike in the study of Ochoa et al., where 60 % of the sample population were Tönnis grade 0 and 28 % were Tönnis grade 1, our study evaluated subjects with end-stage OA undergoing THR. Given the joint degeneration seen in advanced OA, some of the radiographic signs were not as apparent, which may explain our lower numbers of subjects with FAI. Tanzer and Noiseux [17] conducted a prospective study involving 200 consecutive patients undergoing THR. Of the 200 patients, 125 (62 %) had PHOA, and all patients in this subset had a pistol grip deformity detected radiographically. Tanzer and Noiseux’s population was similar to that of our study, but our prevalence of FAI was lower. This may be explained by presence of osteophytes in advanced OA that appear like pistol grip deformities. Furthermore, our careful assignment of subjects with osteophytes and questionable FAI to the “not possible to exclude FAI” group, may have contributed to lower numbers in the “definite FAI” group.
In another study, Kim et al. [16] assessed FAI in two groups who previously had hip arthroscopy for early OA. Group I consisted of patients with no radiographic OA but with degenerative changes of the labrum and cartilage on magnetic resonance (MR) arthrograms, while group II was composed of patients with early radiographic OA. Six of 21 (29 %) subjects in group I and 12 of 22 (56 %) subjects in group II showed radiographic evidence of FAI. The findings of Kim et al. are comparable to our figures. Our sampled populations were similar in that the subjects had hip OA that required a surgical procedure. They too used preoperative radiographs but had additional imaging from MR arthrography. More recently, in a cross-sectional population-based study that included 3,620 subjects (36.7 % male, 63.2 % female), Gosvig et al. reported the prevalence of hip OA to be 9.5 % in men and 11.2 % in women [13]. Among these subjects with hip OA, 71 % of males and 36.6 % of females had a concomitant hip malformation associated with FAI [13]. Of interest, new data are also emerging on the prevalence of cam-type deformities in asymptomatic individuals. Reichenbach et al. obtained MRI studies for 244 asymptomatic males (mean age 19.9 years) and found an overall prevalence of cam-type deformities to be 24 % [12]. The authors attributed this high prevalence of FAI in asymptomatic males to MRI imaging for its ability to better detect FAI signs.
The heterogeneity—including patient populations evaluated, imaging modalities used, and definitions for FAI—of the studies described above makes it challenging to compare prevalence figures [12–17]. From the radiographs that we could accurately assess, 27 of 52 subjects (52 %) had FAI, a number lower than that reported by Ochoa et al. [15] and Tanzer and Noiseux [17] but closer to the findings of Gosvig et al. [13] and Kim et al. [16]. Our sample of 52 subjects with both AP and lateral films available is one of the limitations of our study. For example, sample size precludes comparative analyses between different FAI types or patient subgroups. However as described, the substantial heterogeneity in patient populations where FAI prevalence has been estimated as well as differences in imaging modalities used and definitions for FAI warrants on-going epidemiologic studies of FAI. One limitation of our study’s retrospective design was the inability to assure standardized technique and views for the radiographs assessed. This is important since incorrect positioning or radiographic technique may affect the accuracy of interpretation [6]. In addition, the lack of lateral view radiographs for 23 of the 75 (31 %) eligible subjects made it difficult to discern cam impingement features. This may explain why we observed more pincer cases despite reports that mixed-type impingement is the most common. Our gender distribution for impingement type, however, was consistent with previous literature [5, 12–14]. Moreover, many of the subjects had radiographic end-stage OA, which made it difficult to exclude FAI (e.g., it was challenging to distinguish an osteophyte from a pistol grip deformity).
The high frequency of FAI in PHOA has resulted in the interest in FAI as a primary cause and as a potentially surgically remediable condition. Further epidemiological studies including longitudinal studies given the cross-sectional nature of many previous studies, as well as the development of standardized radiologic criteria for identifying presence of bony abnormalities, are required to clarify the relationship between hip impingement and PHOA. Longitudinal studies would also be valuable in elucidating the percentage of asymptomatic individuals showing FAI radiographic signs who develop symptomatic hip OA and require THR in the future.
References
Leunig M, Beaule PE, Ganz R (2009) The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res 467:616–622
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87(7):1012–1018
Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 466:264–272
Stafford G, Witt J (2009) The anatomy, diagnosis and pathology of femoroacetabular impingement. Br J Hosp Med 70(2):72–77
Hack K, Di Primio G, Rakhra K, Beaule PE (2010) Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am 92:2436–2444
Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR 188:1540–1552
Reid GD, Reid CG, Widmer N, Munk PL (2010) Femoroacetabular impingement syndrome: an underrecognized cause of hip pain and premature osteoarthritis? J Rheumatol 37(7):1395–1404
Crawford JR, Villar RN (2005) Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br 87(11):1459–1462
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ et al (2008) A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90(Suppl 4):47–66
Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P et al (2009) Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res 467:666–75
Bardakos NV, Villar RN (2009) Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br 91-B:162–169
Reichenbach S, Juni P, Werlen S, Nuesch E, Pfirrmann CW, Trelle S et al (2010) Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res 62:1319–1327
Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A (2010) Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am 92:1162–1169
Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P (2008) The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol 49:436–441
Ochoa L, Dawson L, Patzkowski JC, Hsu JR (2010) Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res 468:2710–2714
Kim YC, Hwang DS, Lee CH, Kwon ST (2006) Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res 456:128–132
Tanzer M, Noiseux N (2004) Osseous abnormalities and early osteoarthritis. Clin Orthop Relat Res 429:170–177
Acknowledgments
This study received support from the Canadian Institutes of Health Research (#PAL-98735) and the Canadian Arthritis Network
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The corresponding author (JE) has full control of all primary data and agrees to allow the journal to review the data if requested.
Ms Lung received the Philip Rosen Award for Best Clinical Presentation at the 2010 Annual Meeting of the Canadian Rheumatology Association and a Canadian Institutes of Health Research Summer Student Salary Award.
Rights and permissions
About this article
Cite this article
Lung, R., O’Brien, J., Grebenyuk, J. et al. The prevalence of radiographic femoroacetabular impingement in younger individuals undergoing total hip replacement for osteoarthritis. Clin Rheumatol 31, 1239–1242 (2012). https://doi.org/10.1007/s10067-012-1981-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-1981-9