Abstract
Introduction
Tibiocalcaneal (TC) arthrodesis is a limb salvage method for patients with severe deformities combined with necrosis and/or luxation of the talus. The aim of this study was to examine the clinical and radiological outcome of TC arthrodesis.
Materials and methods
This retrospective study identified 12 patients with luxation and/or necrosis of the talus, due to charcot neuroarthropathy (83.3 %) or traumatic injuries (16.7 %). All patients underwent TC arthrodesis by an external fixator or nail arthrodesis. The mean follow up was 18 (6–36) months with a mean age of 51.3 (30–66) years. The data were collected using the AOFAS score as well as clinical and radiological examination during regular follow up.
Results
Seven (58.3 %) patients were treated with an external fixator, four (33.3 %) with nail arthrodesis and one (8.3 %) patient rejected both fixation methods. Four (100 %) patients achieved radiological and clinical bone union after nail arthrodesis and four (57.1 %) patients after external fixation. Three (42.9 %) patients treated by an external fixator showed a radiological moderate bone fusion, but a stable, asymptomatic non-union. One (8.3 %) case ended up in transfemoral amputation. Eleven patients (91.7 %) regained independent mobilization. The mean AOFAS score improved from 24.3 preoperatively to 66.7 postoperatively (p < 0.05). The postoperative satisfaction rate was good to excellent in 83.3 %.
Conclusion
TC arthrodesis is a promising and effective method for the treatment of severe ankle deformities with talus luxation. It allows patient’s return to mobility with good to excellent patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe ankle deformities with luxation and/or necrosis of the talar body are very challenging for surgical treatment as they lead to destruction of the hindfoot, ankle arthrosis and poor function. Aetiologies of talar body necrosis could be previous trauma [1], severe deformity [2], inflammatory arthritis [3] or Charcot neuroarthropathy (CN) [4, 5]. Surgical management has to consider severe bone loss due to necrosis, bone fragility, diabetes, recurrent ulcers, circulating disorders or infections in cases of CN. Surgical pre-planning is multifactorial, including radiological exams as well as consideration of comorbidities (e.g., diabetes, neurological disorders), life style (e.g., smoking, alcohol abuse) and patient expectations. For severe deformities, ankle arthrodesis (internal or external fixation techniques) is often the only alternative to limb amputation [6]. Tibiocalcaneal (TC) arthrodesis is typically considered as a limb salvage procedure in patients with necrosis and dislocation of the talar body or osteomyelitis [7, 8]. Depending on the presence or absence of ulcers and/or infection, an internal or external fixation technique is chosen. The aim of TC fusion is to create a stable, plantigrade, braceable foot and thereby mobilize the patient [9]. Thereby transtibial or transfemoral amputation can be prevented. Uncontrolled infection, non-union and failure of fixation are the main causes for failed TC arthrodesis [7, 10]. Intramedullary nails as well as external fixators are frequently used, as they offer stable fixation and allow full weight bearing afterwards.
The aim of this study was to examine the clinical and radiological outcome of TC arthrodesis in severe ankle deformities with necrosis of the talar body.
Materials and methods
The present study was performed in accordance with the Declaration of Helsinki. Between February 2012 and March 2015 we retrospectively identified 12 patients with luxation and/or necrosis of the talus, 10 (83.33 %) due to Charcot deformity (Sanders stadium IV, Eichenholtz III) and 2 (16.67 %) posttraumatic ankle luxation. All patients underwent reconstruction of the ankle with talectomy followed by TC arthrodesis using either an external fixator (Hoffmann Xpress, Stryker, Kalamazoo, MI) or nail arthrodesis (T2 SGA nail, Stryker, Kalamazoo, MI). The mean follow up was 18 (±7.24; 6–36) months. Six (50.0 %) patients were male and six (50.0 %) were female. The mean age at time of surgery was 51.3 years (±10.45; 30–66). Seven left and five right ankles were operated. Seven (58.3 %) patients were treated with an external fixator, four (33.3 %) with nail arthrodesis and one (8.3 %) patient rejected both fixation methods. In this patient the TC arthrodesis was fixed by a dorsal plaster cast postoperatively. An overview of the patient’s demographics is shown in Table 1. All patients included in this study were conservatively incurable and had clear unstable deformities. Indications for an external fixator were recurrent ulcers or a history of infection in the last 6 months. Otherwise nail arthrodesis was favoured. Preoperative all patients received a dorsoplantar and lateral standing radiograph of the affected foot.
All surgeries were performed under general anaesthesia in supine position. The aim was to rescue patient’s leg by creating a stable arthrodesis in a plantigrade position. The lateral malleolus and the talus were dissected. Afterwards tibial and calcaneal joint surfaces were positioned congruently in a plantigrade position. Depending on whether there were ulcers or positive microbiological wound germs, nail arthrodesis or an external fixator were used for TC arthrodesis. Those patients with external fixation had to rest their leg for at least 12 weeks until the external fixator was removed. Afterwards an orthopaedic splint had to be worn during night and a total contact cast for full weight bearing by day for 12 months. After 1 year patients got an orthopaedic shoe with dispensing aid. All patients with nail arthrodesis had to rest their leg for 6 weeks postoperatively. Afterwards they started weight bearing half of body weight for 3 weeks and were allowed to full weight bearing from the 10th week on. Within this period the operated ankle was placed into a walker boot (VACO®ped, Oberlaindern, Germany).
The outcome data were collected using the AOFAS score pre- and postoperatively as well as clinical and radiological examination during regular follow up at 6 and 12 weeks, 6 months, 1 year and then yearly postoperatively. The main focus of the postoperative examination was an absent infection, possibility of independent mobilization and radiological as well as clinical ankle fusion. Also, all patients were asked, if they would perform surgery again.
The Graph pad prism was used for statistical analysis. The parametric t test was performed to analyse for statistically significant differences of paired data. To verify and compare the different fixation techniques and status of bone union regarding AOFAS score, the Kruskal–Wallis-Test was used. A p value less than 0.05 indicated statistical significance.
Results
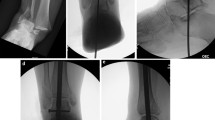
All four (100 %) patients treated by nail arthrodesis achieved clinical and radiological fusion at an average of 10.5 (±5.75; 6–18) months. After a period of 12 (±3.46; 6–18) months four (57.1 %) patients reached clinical and radiological bone fusion after external fixation. The remaining three (42.9 %) cases with an external fixator showed a moderate bone fusion in the radiographs, but achieved a stable, asymptomatic pseudarthrosis in clinical examination. Radiographs of two individual cases with TC arthrodesis are shown in Figs. 1 and 2. 91.7 % regained independent mobilization. In total, the mean AOFAS score improved from 24.3 (±17.2; 0–48) preoperatively to 66.7 (±12.14; 45–83) postoperatively (p < 0.0001). The mean pre- and postoperative AOFAS scores according to fixation technique and postoperative bone union are shown in Figs. 3 and 4. Clinical and radiological bone fusion was missing in the patient treated by a dorsal plaster cast. This case ended up in a transfemoral amputation due to an exacerbated infection. Apart from this case no other intra- or postoperative complications occurred. At final follow-up there were no infections. All patients, except for the one who ended up in amputation, gained independent mobilization and were able to put full weight on the operated ankle in a shoe with dispensing aid at last follow up. The satisfaction with the procedure was good to excellent in 83.3 % of the patients. All but one (8.3 %) patient would have done surgery again.
Preoperative radiograph of a 55-year old male patient with posttraumatic ankle destruction followed by an empyema of the ankle (a). Directly postoperative radiographs show talectomy and tibiocalcanear arthrodesis by an external fixator (b + c). Radiograph 12 weeks postoperatively, bony consolidation started and the external fixator was removed (d). X-rays e and f show postoperative status after 1 and 2 years with complete bone union. The patient was able to walk in a shoe with dispensing aid
X-rays a and b showing a 66-year old female patient with severe ankle deformity and necrosis of the talar body due to CN. Talectomy and nail arthrodesis was performed showing a plantigrade foot postoperatively (c + d). X-rays e and f show complete bone union 1 year postoperatively. The patient was able to walk in a shoe with dispensing aid
Discussion
The most important finding of our study was that TC arthrodesis is a successful limb salvage method for severe ankle deformities. It allows independent mobilization by producing a stable, plantigrade position of the foot, which is necessary for the orthopaedic technicians to perform individual devices.
As mentioned above, complex ankle deformities with necrosis and/or luxation of the talar body due to CN or other aetiologies present a challenge for surgical treatment. The main aim is to retain the limb and to restore mobility. The collapse and destruction of the talar body causes high instability of the ankle, combined with soft tissue damages, that often lead to recurrent ulcerations and secondary chronicle infections. Thus, talectomy with arthrodesis of the foot and ankle often is the only way for stabilization and cure of pre-existing infections to preserve the limb. In total, our bone fusion rate seems to be relatively small, but the main goal is a stable non-union situation. One has to distinguish between the fixation techniques, since the preoperative clinical condition is considerably worse in patients that received an external fixator, due to existing ulcers or infections. In the present study, a bone fusion rate of 100 % was achieved using intramedullary nail arthrodesis. After external fixation 57.1 % showed complete fusion in radiographs and 42.9 % had a stable and asymptomatic non-union. This implies that radiological bone fusion is not mandatory.
A stable pseudarthrosis seems to be sufficient for a good functional outcome. Fabrin et al. [11] examined five TC arthrodesis by an external fixator in patients with CN and reported one bone fusion, two stable fibrous union, one unstable pseudarthrosis and one transtibial amputation. They also concluded that a stable fibrous union leads to satisfying function. Similar results are presented by Rochmann et al. [12]. Using an ilizarov external fixator for salvage of traumatic, infected talar injuries in 11 patients, they reported a mean AOFAS score of 65.0 postoperatively and an 82 % bone fusion rate. This is also reflected in our AOFAS score, as it improved significantly (from 23.0 to 63.0) in the three patients with a stable pseudarthrosis. Overall, the postoperative improvements in our AOFAS score show that the salvaged limbs gained a satisfactory function after both fixation techniques.
After a mean follow-up of 5 years, Caravaggi et al. [10] reached a 86.7 % limb salvage rate after tibiocalcaneal nail arthrodesis in 45 patients with CN, seven with ulcers. Compared to the outcome of arthrodesis in patients with ulceration, the results are considerably better in patients with intact skin and soft tissues. Dalla Paola et al. [13] examined 18 patients with CN without chronic ulceration and reported a 100 % limb salvage and a 77.8 % bone fusion rate after nail arthrodesis. Likewise, Pinzur et al. [5] achieved a 100 % limb salvage rate after nail arthrodesis in patients with CN without ulcers. This underlines that the rate of complications following arthrodesis is higher in patients with existing infections or ulcerations, as reflected in our results. Similar results are presented by Siebachmeyer et al. [14], who examined the outcome of 20 patients with CN, 15 with chronic ulceration, after intramedullary nail arthrodesis. They achieved a limb salvage rate of 100 %, a 90 % bone fusion rate and all but one patient regained independent mobilization. They concluded that intramedullary nail arthrodesis is a successful fixation technique even in the presence of ulcers. Thus, the existence of ulcers should not necessarily be considered as an exclusion criterion for intramedullary nail arthrodesis. Randomized studies should be carried out to confirm superiority for any fixation technique in cases of patients with chronic ulcerations.
We acknowledge that there are limitations to our study. First, our study does only present retrospective results, thus causing recall bias. Second, our patient cohort is relatively small, since the number of patients with such severe ankle deformities is limited. Furthermore a power-analysis has not been performed. Third, the results of the AOFAS scores must be viewed critically [15]. CN leads to polyneuropathy causing reduction of sensation of pain. Besides, TC arthrodesis changes the gait and limits the function of the foot and ankle. Thus, sub items such as pain and function have limited significance.
Conclusion
TC arthrodesis is a promising and effective method as a limb salvage procedure for severe ankle deformities with talus luxation. It allows patient’s return to mobility with good to excellent patient satisfaction. A stable fibrous union seems to be sufficient for a good functional outcome. To regain mobility especially in high-risk foot deformities the individual orthopaedic custom made shoe manufacture is very important for the long-term outcome. Good functional results can only be achieved in well established interdisciplinary teams as orthopaedic shoe makers, technicians and orthotists who work hand in hand with the surgeons.
References
Ochman S, Evers J, Raschke MJ, Vordemvenne T (2012) Retrograde nail for tibiotalocalcaneal arthrodesis as a limb salvage procedure for open distal tibia and talus fractures with severe bone loss. J Foot Ankle Surg 51:675–679. doi:10.1053/j.jfas.2012.04.015
Hammett R, Hepple S, Forster B, Winson I (2005) Tibiotalocalcaneal (hindfoot) arthrodesis by retrograde intramedullary nailing using a curved locking nail. The results of 52 procedures. Foot Ankle Int 26:810–815
Anderson T, Linder L, Rydholm U, Montgomery F, Besjakov J, Carlsson A (2005) Tibio-talocalcaneal arthrodesis as a primary procedure using a retrograde intramedullary nail: a retrospective study of 26 patients with rheumatoid arthritis. Acta Orthop 76:580–587. doi:10.1080/17453670510041592
Caravaggi C, Cimmino M, Caruso S, Dalla Noce S (2006) Intramedullary compressive nail fixation for the treatment of severe Charcot deformity of the ankle and rear foot. J Foot Ankle Surg 45:20–24. doi:10.1053/j.jfas.2005.10.003
Pinzur MS, Noonan T (2005) Ankle arthrodesis with a retrograde femoral nail for Charcot ankle arthropathy. Foot Ankle Int 26:545–549
Pinzur MS (2007) Current concepts review: charcot arthropathy of the foot and ankle. Foot Ankle Int 28:952–959. doi:10.3113/FAI.2007.0952
Cinar M, Derincek A, Akpinar S (2010) Tibiocalcaneal arthrodesis with posterior blade plate in diabetic neuroarthropthy. Foot Ankle Int 31:511–516. doi:10.3113/FAI.2010.0511
Mirzayan R, Early SD, Matthys GA, Thordarson DB (2001) Single-stage talectomy and tibiocalcaneal arthrodesis as a salvage of severe, rigid equinovarus deformity. Foot Ankle Int 22:209–213
Zgonis T, Stapleton JJ, Jeffries LC, Girard-Powell VA, Foster LJ (2008) Surgical treatment of Charcot neuropathy. AORN journal 87:971–986 (quiz 987–990)
Caravaggi CM, Sganzaroli AB, Galenda P, Balaudo M, Gherardi P, Simonetti D, Ferraresi R, Farnetti A, Morandi A (2012) Long-term follow-up of tibiocalcaneal arthrodesis in diabetic patients with early chronic Charcot osteoarthropathy. J Foot Ankle Surg 51:408–411. doi:10.1053/j.jfas.2012.04.007
Fabrin J, Larsen K, Holstein PE (2007) Arthrodesis with external fixation in the unstable or misaligned Charcot ankle in patients with diabetes mellitus. Int J Low Extrem Wounds 6:102–107. doi:10.1177/1534734607302379
Rochman R, Jackson Hutson J, Alade O (2008) Tibiocalcaneal arthrodesis using the Ilizarov technique in the presence of bone loss and infection of the talus. Foot Ankle Int 29:1001–1008. doi:10.3113/FAI.2008.1001
Dalla Paola L, Volpe A, Varotto D, Postorino A, Brocco E, Senesi A, Merico M, De Vido D, Da Ros R, Assaloni R (2007) Use of a retrograde nail for ankle arthrodesis in Charcot neuroarthropathy: a limb salvage procedure. Foot Ankle Int 28:967–970. doi:10.3113/FAI.2007.0967
Siebachmeyer M, Boddu K, Bilal A, Hester TW, Hardwick T, Fox TP, Edmonds M, Kavarthapu V (2015) Outcome of one-stage correction of deformities of the ankle and hindfoot and fusion in Charcot neuroarthropathy using a retrograde intramedullary hindfoot arthrodesis nail. Bone Joint J 97-B:76–82. doi:10.1302/0301-620X.97B1.34542
Kostuj T, Krummenauer F, Schaper K, Stief F, Zettersten K, Baums MH, Meurer A, Lieske S (2014) Analysis of agreement between the German translation of the American Foot and Ankle Society’s Ankle and Hindfoot Scale (AOFAS-AHS) and the foot function index in its validated German translation by Naal et al. (FFI-D). AOTS 134(9):1205–1210. doi:10.1007/s00402-014-2046-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Ettinger, S., Stukenborg-Colsman, C., Plaass, C. et al. Tibiocalcaneal arthrodesis as a limb salvage procedure for complex hindfoot deformities. Arch Orthop Trauma Surg 136, 457–462 (2016). https://doi.org/10.1007/s00402-016-2420-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2420-1