Abstract
Introduction
We aimed to identify the effects of intraoperative applied leukocyte-poor platelet-rich plasma (LP-PRP) during knee arthroscopy for degenerative lesions involving pain, function and quality of life.
Methods
We performed a randomized controlled, double-blind trial (RCT) including 58 patients for arthroscopic knee surgery for cartilage or meniscal degeneration with allocation into the LP-PRP (n = 24) or control group (n = 34). During arthroscopy, LP-PRP was injected intra-articular in the intervention group. At baseline, 6 weeks, 6 months and 12 months pain, function, and life quality were assessed.
Results
91 % of enrolled patients were available for 12 months follow-up. Pain was significantly lower in the LP-PRP group (VAS 0.9. vs. 2.3) at 6 (p = 0.008) but not at 12 months (VAS 1.0 vs. 1.6, p = 0.063). LP-PRP application improved the Lysholm Score at 6 (77.5 vs. 65.6, p = 0.033) and 12 months (83.2 vs.70.0, p = 0.007). Assessment of life quality (SF-36) concerning the physical component summary was significantly higher at 6 weeks (33.9 vs. 25.6, p = 0.001) and 6 months (29.9 vs. 27.1, p = 0.027) in the LP-PRP group but equal at 1 year (31.4 vs. 30.1, p = 0.438).
Conclusions
Intraoperative application of LP-PRP may enhance pain reduction and gain of knee function within 6–12 months compared to arthroscopy alone.
Level of evidence
II, randomized controlled clinical trial with reduced power.
ClinicalTrials.gov identifier
NCT02189408.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Results of recent proteomic and molecular research create serious doubts in common mechanistic theories of osteoarthritis (OA) and rather hypothesize an inflammation [1] of a joint complex with cartilage, synovia and subchondral bone affecting and regulating one another to maintain homeostasis [2, 3].
Topical application of platelet-rich plasma (PRP) is an emerging method for musculoskeletal tissue regeneration with an exponentially increasing popularity [4] since its first use in 1987 in cardiac surgery. Today, numerous studies involve PRP use in OA and cartilage degeneration [5, 6]. Platelet α-granules with high concentrations of growth factors, including, for example., transforming growth factor-β (TGF-β), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF), were identified as OA-modifying and chondrocyte-promoting mediators [7]. By interfering with inflammation pathways, for example., nuclear factor ‘kappa-light-chain-enhancer’ of activated B cells (NF-kB), a ubiquitous regulatory transcription factor, and decreasing the concentration of tumor necrosis factor-α (TNF-α) and matrix metalloproteinase-13 (MMP-13), PRP can inhibit cartilage degradation or enhance endogenous or exogenous repair [8, 9] in vitro and in several animal models. Gene expression of matrix components, like collagen Type II and aggrecan, is upregulated and can particularly restore chondrocyte morphology and function [9, 10].
A number of preclinical studies and randomized controlled trials (RCT) provided strong evidence for clinical improvement and pain relief by intra-articular PRP application, even in total knee arthroplasty [11, 12]. We thought that evaluation of potential outcome improvement by additional peri-operative LP-PRP application may be a promising investigation because of the frequent use of arthroscopy for OA therapy. Only a few RCT examined simultaneous LP-PRP injection and arthroscopy [13] with scarce evidence for combined use for arthroscopic surgery in OA. The purpose of our study was to evaluate pain reduction, functional improvement and changes of life quality after intraoperative LP-PRP injection in arthroscopy compared to arthroscopy alone by conducting a double-blind RCT.
Methods
Patient recruitment
During January 2010 and December 2011 all patients presenting with non-traumatic knee pain, image-proven OA and intended arthroscopic surgery after failed conservative treatment of at least 12 weeks, were considered to be study participant. Inclusion criteria were OA stages II to IV according to Kellgren–Lawrence Classification for plain radiographs or modified Outerbridge grading for MR-imaging with or without concomitant meniscal lesions. Due to our study protocol, we only included patients favoring general anesthesia. As used the ACP®-system (Arthrex, Naples, Florida, USA) for LP-PRP preparation requires an additional blood withdrawal and patient-sided preparation, patient blinding could not be guaranteed in conscious participants. We excluded patients incapable of providing informed consent due to age or mental status, circumscribed chondral damage with surgical option for regenerative procedures (microfracture, autologous chondrocyte implantation), local or systemic infection, corticosteroid injection within the last 3 months, rheumatological disorders, OA with collateral ligament instability >grade II, immunosuppression, cancer or other severe disorders contradicting autologous transfusion of blood products or resulting in a probable loss to follow-up.
Study protocols were approved by the local ethics committee of our faculty of medicine. All included patients provided written informed consent after a detailed explanation of the trial, PRP in general and autologous conditioned plasma (ACP®, Arthrex, Naples, Florida, USA), which enables preparation of a leucocyte-poor but platelet-rich plasma using a sterile double-syringe system inside the OR.
Outcome measures
Outcome measures were chosen to represent three patient-related aspects of degenerative knee diseases: pain, knee function and quality of life. Pain was measured using a 100-mm visual analog scale (VAS). Function was assessed using the Lysholm Score (Lysholm Knee Scoring Scale), quality of life pre- and postoperatively using the national version of the short-form-36 (SF-36, RAND corporation). This is a universal and widespread, patient-reported health survey consisting of eight weighted sub-scales respecting physical and mental health aspects. Pain at 6-month follow-up was defined as the primary endpoint as the LP-PRP effect is known to be temporary. All used outcome measures were well established in and validated for patients with knee disorders and/or osteoarthritis [14–16].
Operative technique
Knee arthroscopy was performed according to an internal standard operating procedure (SOP) with the patient in a supine position, using an inflatable tourniquet and approaching the joint through anterolateral and anteromedial standard portals. The knee joint and its cartilage surface was completely inspected with a 30° scope and the anterior cruciate ligament (ACL) and both menisci were manually tested for integrity and fixation using a hook. After completing arthroscopic interventions (cartilage debridement, partial meniscectomy), the irrigation fluid was evacuated. In cases of random allocation to the interventional group, 15 ml of blood were obtained from a peripheral cubital vein and preparation of LP-PRP was made using the ACP®-technique. Blood was centrifuged for 5 min with 1.500 rpm and separated into three fractions, with the thrombocyte phase being isolated in a second sterile syringe for direct application via the anterolateral portal. Wound closure without any kind of drainage was performed and full-weight bearing was allowed immediately.
Sample size calculation, study design and statistical procedures
A sample size calculation based upon a two-sided t test with α = 0.05 and 1 − β = 0.8 and an estimated and required difference between the intervention and control group of 0.1 (1 unit respectively 10 mm on VAS) resulted in a necessary number of 60 patients with a desired allocation ratio of 1 (G*-Power 3.1, a priori sample size calculation). The difference of 10 mm on VAS was chosen to be the minimal effect of clinical relevance.
Study patients were randomized by a doctor’s assistant in a blind manner using sealed white shuffled envelopes, which contained either a “PRP” or “control” note.
Patient blinding was ensured by the fact that the whole preparation and application procedure took place during general anesthesia. Intra-articular injection was made through the standard anterolateral portal with no additional, distinguishing incision. Participation in our trial, but not specific group allocation was described in shared documents and medical records and allocation details were only available for few researchers within the institute.
Doctors blinding was guaranteed by following a standard follow-up procedure. All physical examinations at follow-up evaluations took place in our outpatients’ office and were performed by an orthopedic surgeon neither being involved in the operative procedure nor having access to allocation uncovering documents. LP-PRP application was not mentioned in the operation protocols.
Data analysis was performed using SPSS® for Windows®, version 22.0 (SPSS Inc., Chicago, IL, USA). Presentations of metric variables included the mean, median and standard deviation, whereas nominal data were shown as the relative and absolute frequency.
All analyses consisted of a two-sided check of significance with a p value <0.05, which indicated significant results. To identify a Gaussian distribution, the Kolmogorow–Smirnow test was performed. Metric variables with a Gaussian distribution were analyzed using the t test for unpaired, independent samples, and the equality of variances was thus consistent with Levene’s test. If the Gaussian distribution could not be presupposed, then the Mann–Whitney U test as a non-parametric method was performed. Quality of randomization between both groups with special respect to intraoperative grade of OA (IRCS classification) or distribution of meniscal degeneration was controlled post hoc in this manner.
More than 2 dependent, non-Gaussian samples were compared with the Friedman test.
Categorized data were analyzed using the Chi-square and Fisher’s exact test. Significant results were further specified using confidence intervals and VAS as the primary endpoint, in addition to post hoc power analysis.
Results
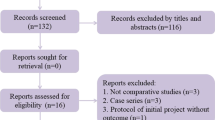
According to CONSORT-criteria, patient enrollment and allocation could be seen in Fig. 1. We finally included 58 patients with a mean age of 64 years, average cartilage degeneration grade III according IRCS classification and main meniscal damage located medially. The demographic details are shown in Table 1.
We could achieve a good 12-month follow-up of 91.4 %. All patients lost to follow-up (PRP group = 2, control group = 3) showed degeneration of IRCS grade IV and underwent total knee arthroplasty (TKA) due to severe osteoarthritis. There were no significant differences concerning sex, operated side, intraoperative grade of cartilage lesion or distribution of concomitant degenerative meniscal tears comparing intervention and control group. Patients allocated to the intervention group received a mean volume of 4 ml of LP-PRP.
We further could not identify further significant preoperative differences of baseline outcome measures between the two groups except a slight difference according to the SF 36 physical sub-scale favoring the LP-PRP group. Values of all outcome measures pre- and postoperatively as well as statistical data can be found in Table 2.
Pain at preoperative assessment was equal between the PRP and control group, then significantly decreased after arthroscopy in both groups at 6 weeks with a cumulative relative pain reduction of 68 %. Further development of pain diverges allocation-dependent: in the PRP group, pain further reduced to a minimum of 0.9 after 6 months, whereas it remains at 2.3 in the control group with a significant difference (p = 0.008). Compared to preoperative levels, the relative pain reduction after LP-PRP application reached 89 %. Both groups exhibited final low VAS scores without significance (p = 0.063).
Knee function, which was appraised with the Lysholm Score, also showed an improvement in both groups with comparable baseline scores (Table 2). After intervention, values of LP-PRP-treated patients significantly increased more than values in the control group at 6 weeks, and 6 and 12 months with a final Lysholm Score difference of 13 which corresponds to a relative improvement of 99.5 and 99.4 %, respectively.
Patients’ self-assessment using SF-36 was analyzed with regard to physical and mental health. The physical health baseline was significantly higher in the LP-PRP group. After application, LP-PRP patients demonstrated significantly higher scores with a peak at 6 weeks. An opposing trend was observed concerning the mental health summary, which significantly favored the control group at 6 weeks, 6 months, and 12 months after being equivalent at preoperative assessment. Consistent with the PRP group, the highest scores could be found after 6 weeks.
Discussion
In our study, we could demonstrate that LP-PRP applied during knee arthroscopy of degenerative knee joints is superior to arthroscopy alone going along with decreasing VAS and increasing Lysholm and SF-36 Scores. It gives a clue of LP-PRP potential for pain relief, functional improvement and physical aspects of life quality. With significance, we demonstrated that PRP is not only effective in young and healthy patients suffering from sports-related injuries, but also useful for a population with moderate to severe stages of OA. Despite the increasing number of publications [17], only a few studies provide substantial level I or II evidence. The initial skepticism concerning PRP may have resulted from inconsistent therapeutic and adverse effects. Based on profound knowledge of content and interactions of PRP today, the oppositional effects can be explained with the different formulations regarding the proportion of leucocytes and erythrocytes. Braun et al. [18] recently demonstrated that leukocyte-rich formulations (LR-PRP) and red blood cell concentrates cause significantly higher rates of cell death among chondrocytes compared to the LP-PRP used by us. The concentration of TNF-α, a key mediator in inflammation, which directly correlates to OA-related pain [19] was proven to be lower in LP-PRP in vitro. The direct reduction of circulating TNF-α by LP-PRP may explain the immediate and extensive decrease of VAS Score and thereby the reported pain relief.
The Lysholm Score was significantly improved after LP-PRP application for the entire follow-up period of 12 months. LP-PRP is reported to reduce joint swelling and periods of effusion, and thereby may naturally extend the range of motion and activity levels. Most likely by a temporary restoration of physiological balance between pro- and anti-inflammation, LP-PRP can improve pain and function for a limited period, but definitely not repair structural damaged tissue, which may be an explanation for therapy failure in severe OA stages.
Our study results cannot only be reasonably explained by latest molecular research, but are also supported by clinical studies with comparable results [4–6, 20–22].
Interestingly, our study shows significant results for the efficacy of arthroscopy for pain reduction independently of simultaneously PRP use. We like to underline the immediate and lasting relative pain reduction of a mean of 68 % at 6 weeks and 80 % after 12 months in both groups. Jackson [23] and Wang-Saegusa [6] published nearly identical data reporting percentage improvement between 68 and 88 %. Aware of high-quality, evidence level I publications, which cannot provide statistical support for arthroscopic debridement and partial meniscal resection for degenerative tears [24], we deem arthroscopic knee surgery in general and use of LP-PRP in particular a considerable option also for OA treatment with respect to low rate of complications and rare side and adverse effects using LP-PRP [20]. We can recommend its use in cases of intended arthroscopy after failed conservative treatment with profound education about the temporary nature of potential improvement and the generally nonrefundable average costs ranging from 80 to 180€ in Germany. We also have to point out that intraoperative use of LP-PRP is currently not represented in Germany’s diagnosis related groups (DRG) revenue system.
There were several limitations in our study. Our randomization procedure caused two groups with an unequal number of participants. We could not include the number of a priori—calculated patients to achieve the aspired power. Although post hoc power analysis showed a power of 0.86 for VAS at 6 months for our primary endpoint (post hoc, two-tailed, Wilcoxon-signed rank test, calculated by G*Power 3.1 for Mac OS X), our intended quality could not be achieved and our study must therefore be categorized as a RCT of evidence level II.
Follow-up examination was restricted to 12 months due to the temporary effect of PRP, which leaves potential long-term effects undetected. Repetitive application after 6 and/or 12 months was not performed, but would have been an interesting aspect to examine if LP-PRP-related effects could be reproducible and change mid-term outcome.
We did not analyze the platelet or leukocyte concentration to characterize and quantify the PRP formulations because we used direct preparation inside the OR using the ACP®-double-syringe technique with immediate application. Our outcome measure focus on patient-related aspect, but lack in objective parameters like IL6, sonographically assessed volume of effusion or range of motion.
Conclusions
Intra-articular LP-PRP application may be a considerable, effective additional treatment during knee arthroscopy for degenerative meniscal or cartilage lesions, resulting in remarkable pain reduction and functional improvement for a limited period of 6–12 months. Patients with severe osteoarthritis may not benefit from this procedure.
Further studies including more patients in equally distributed groups and examination of repetitive application with a follow-up of 24 or more months is adorable.
References
Berenbaum F (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr Cartilage 21:16–21
Mobasheri A (2013) The future of osteoarthritis therapeutics: emerging biological therapy. Curr Rheumatol Rep 15:385–394
Fernandes JC, Martel-Pelletier J, Pelletier JP (2002) The role of cytokines in osteoarthritis pathophysiology. Biorheology 39:237–246
Sampson S, Gerhardt M, Mandelbaum B (2008) Platelet rich plasma injections grafts for musculoskeletal injuries—a review. Curr Rev Musculoskelet Med 1:165–174
Spakova T, Rosocha J, Lacko M, Harvanova D, Gharaibeh A (2012) Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehabil 91:411–417
Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cusco R, Garcia-Balletbo M (2011) Infltration of plasma rich in growth factors for osteoarthritis of the knee -short-term effects on function and quality of life. Arch Orthop Trauma Surg 131:311–317
Boswell SG, Cole BJ, Sundman EA et al (2012) Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy 28:429–439
Sundmann EA, Cole BJ, Karas V et al (2013) The anti- inflammatory and matrix restorative machanisms of platelet-rich plasma in osteoarthritis. Am J Sports Med 42:35–41
Perdisa Filardo G, Di Matteo B, Marcacci M, Kon E (2014) Platelet rich plasma: a valid augmentation for cartilage scaffolds? A systematic review. Histol Histopathol 29:805–814
Park SI, Lee HR, Kim S, Ahn MW, Do SH (2012) Time- sequential modulation in expression of growth factors from platelet-rich plasma (PRP) on the chondrocyte cultures. Mol Cell Biochem 361:9–17
Zhu Y, Yuan M, Meng HY et al (2013) Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarthr Cartilage 21:1627–1637
Aggarwal AK, Shashikanth VS, Marwaha M (2014) Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop 38:387–395
Mirzatolooei F, Alamdari MT, Khalkhali HR (2013) The impact of platelet-rich plasma on the prevention of tunnel widening in anterior cruciate ligament reconstruction using quadrupled hamstring tendon. Bone Joint J 95-B:65–69
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am 86:1139–1145
Wang D, Jones MH, Khair MM, Miniaci A (2010) Patient-reported outcome measures for the knee. J Knee Surg. 23:137–151
Ko Y, Lo NN, Yeo SJ, Yang KY, Yeo W, Chong HC, Thumboo J (2013) Comparison of the responsiveness of the SF-36, the Oxford Knee Score, and the Knee Society Clinical Rating System in patients undergoing total knee replacement Qual Life Res 22:2455–2459
Filardo G, Kwon E, Roffi A, Di Matteo B, Merli ML, Marcacci M (2013) Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2743-1
Braun HJ, Kim HJ, Chu CR, Dragoo JL (2014) The effect of platelet-rich plasma formulations and blood products on human synoviocyte. Am J Sports Med pp 1204–1210
Ohtori S, Takahashi K, Moriya H et al (2004) TNF-alpha and TNF-alpha receptor type 1 upregulation in glia and neurons after peripheral nerve injury: studies in murine DRG and spinal cord. Spine (Phila Pa 1976) 29:1082–1088
Anitua E, Sanchez M, Aguirre JJ, Prado R, Padilla S, Orive G (2014) Efficacy and safety of plasma rich in growth factors intra-articular infiltrations in the treatment of knee osteoarthritis. Arthroscopy. doi:10.1016/j.arthro.2014.05.021
Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A (2013) Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med 41:356–364
Felson DT, Buckwalter J (2002) Debridement and lavage for osteoarthritis of the knee. N Engl J Med 347:132–133
Jackson RW, Dieterichs C (2003) The results of arthroscopic lavage and debridement of osteoarthritic knees based on the severity of degeneration: a 4- to 6-year symptomatic follow-up. Arthroscopy 19:13–20
Moseley JB et al (2002) A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 347:81–88
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
IRB: Ethik-Kommission der Ruhr-Universität Bochum (Approval No. 3564-09).
Rights and permissions
About this article
Cite this article
Duif, C., Vogel, T., Topcuoglu, F. et al. Does intraoperative application of leukocyte-poor platelet-rich plasma during arthroscopy for knee degeneration affect postoperative pain, function and quality of life? A 12-month randomized controlled double-blind trial. Arch Orthop Trauma Surg 135, 971–977 (2015). https://doi.org/10.1007/s00402-015-2227-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2227-5