Abstract
Introduction
Successful anterior cruciate ligament (ACL) reconstruction is dependent on correct placement of both tibial and femoral tunnels. The purpose of this study is to investigate whether we can use intraoperative femoral tunnel length measurement to estimate the correct femoral tunnel placement on coronal plane.
Methods
This prospective study comprised 164 consecutive patients who underwent ACL reconstruction surgery. Transtibial or anteromedial portal technique is used for drilling the femoral tunnels. The length of the femoral tunnel was measured during the operation. The femoral tunnel coronal plane angle was calculated on the postoperative tunnel radiographs. A statistical comparison was made of the lengths of the tunnel, the techniques used drilling and the femoral tunnel angles.
Results
The far anteromedial portal was used in 81 (49 %) cases and the transtibial technique in 83 (51 %) cases. The mean femoral tunnel length was 42 ± 6.4 mm and the mean femoral tunnel coronal angle was 41.1° ± 11.6. The tunnel angle in the transtibial technique was determined as significantly low compared to the far anteromedial portal technique (32.6°:49.8°) and the tunnel length was significantly longer (45.8:38.1 mm) (p < 0.001). In the statistical analysis, it was found that a patient with a tunnel length of 41 mm and above had a 92.1 % likelihood of femoral tunnel angle below 45°.
Conclusion
Femoral tunnel length can be used as a clue for intraoperative evaluation of the femoral tunnel position. If the femoral tunnel length is greater than 41 mm, the coronal plane orientation of the femoral tunnel will be improper and not at a desired position.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most important factor in a successful anterior cruciate ligament (ACL) reconstruction is the correct placement of both tibial and femoral tunnels [1–3]. It has been shown that improper graft placement fails to restore the natural knee biomechanics and cannot control rotational stability. Furthermore, improper tunnels may cause graft impingement, loss of knee motion and increase the rate of re-rupture in later period [1, 4, 5]. Previously sagittal plane position of the graft has been accepted as an important consideration for successful ACL reconstruction; however, importance of coronal plane position of the femoral tunnel has also been recognised to obtain an oblique graft orientation with better understanding of the anatomy of ACL [6–8]. Femoral tunnel drilling is accepted as the critical point to provide an oblique ligament orientation, thus obtaining an anatomic reconstruction that ensures both anteroposterior and rotational stability [9].
During arthroscopic ACL reconstruction, several methods and landmarks have been described to determine the proper entry point for femoral tunnel drilling including clock-face position of the intercondylar notch, ACL footprint and remnants, and other anatomic landmarks such as resident’s ridge, lateral intercondylar ridge, the posterolateral rim, and the lateral bifurcate ridge [10, 11]. Even though it is easy to use the clock-face position as a reference, there are several limitations: it refers to a two-dimensional structure and therefore neglects the depth of the notch, its position varies with knee flexion, and it is not universally employed because of the asymmetric anatomy of the notch [12, 13]. The desired coronal femoral tunnel placement has been stated as between 1 and 2 o’clock for the left knee and 10 and 11 o’clock for the right knee [14]. However, this description of femoral tunnel placement in the coronal plane is determined based mainly on the subjective impression of surgeons and experience is required to do this successfully [15]. Furthermore, the anatomic landmarks may have disappeared in chronic ACL ruptures or during the notchplasty. Therefore, another practical guide which can estimate the proper femoral tunnel placement would be helpful for the arthroscopy surgeons. We hypothesised that there is a relationship between femoral tunnel length and the angle of the tunnel on coronal plane. The purpose of this study is to investigate whether we can use intraoperative femoral tunnel length measurement to estimate the correct femoral tunnel placement on coronal plane.
Patients and methods
This prospective study was performed on 164 consecutive patients with ACL rupture who underwent arthroscopic ACL reconstruction between November 2011 and July 2013 in our hospital. The study was carried out in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All patients gave informed consent prior to their inclusion in the study and local ethics committee approved the study protocol.
Surgical technique
All patients were operated by the same surgeon, and all operations were performed with the single bundle technique. Quadrupled hamstring autografts were used in all cases. Endobutton fixation was used on the femoral side and bio-absorbable interference screws and an additional U-shaped titanium staple were used on the tibial side for graft fixation. The tibial tunnel was drilled first in all patients. This was done with the knee in 90° flexion using a 55° tibial guide. The posterior edge of anterior horn of the lateral meniscus was used as a landmark for the tibial tunnel aperture. After drilling with a reamer at the appropriate thickness according to the graft taken, the entrance for the femoral tunnel was examined. At this stage, the knee was flexed to 90° and 6 mm over the top femoral guide placed thorough tibial tunnel. If the surgeon thinks the femoral tunnel would be in a desired position the pin was placed and the femoral tunnel was drilled by the cannulated reamer. If the surgeon thinks that the femoral tunnel would not be in a desired position an accessory anteromedial portal was opened. In the far anteromedial portal technique, the knee was flexed at least 120° and more. An accessory portal was created under direct visualization using a spinal needle making sure the portal would allow good access to the ACL footprint. After opening the portal, the guide pin was placed in the appropriate position by direct arthroscopic visualisation with free hand technique. Clock-face evaluation and ACL remnants were used as landmark and the femoral tunnel was drilled with a cannulated reamer. All drilled femoral tunnel lengths were measured in millimetres during the operation by depth gauge with 1 mm of the marking separation regardless of which technique was used.
Radiographic measurements
On the postoperative second day, standard anteroposterior (AP), true lateral and tunnel view (patient prone with knee flexed at 40° flexion) radiographs were taken. The rotation of the knee was assessed according to the fibular head position. If the fibular head was either completely projected behind the tibia (internally rotated) or the fibular head showed less than 30 % of projected intersection with the lateral tibial cortex (externally rotated), the radiographs were repeated until proper radiographs were obtained for radiographic measurements.
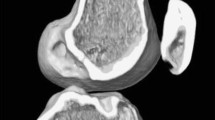
On the tunnel view knee radiographs, the clock-face description of the femoral tunnel placement was evaluated as described by Yamazaki et al. [15]. All measurements were performed by three independent observers, who were blinded to the femoral drilling technique. The average values of the three measurements were recorded and used for the statistical analysis. The clock was drawn between the two lines as follows. One line connected the distal edges of the medial and lateral femoral condyles. The other was parallel to the previous line through the top of the posterior intercondylar notch. The midpoint was determined between the two points and a circle was drawn with this central point. The point of the circle touching the posterior intercondylar notch line was accepted as 12 o’clock and that passing through the medial and lateral femoral condyles line was accepted as 6 o’clock. The centre of the femoral tunnel was marked as the cross-point of the intercondylar clock and the femoral tunnel extension of the 4 mm tunnel outside the joint to the lateral cortex. The line connecting the centre of the clock and the cross-point above was expressed as time shown on the clock. The angle between the drawn clock time and 12:00 was measured in degrees and designated as the clock-face angle of the femoral tunnel (Fig. 1). All the knees were assumed to be left knees. The determined clock-face angles were recorded as 30° = 1 o’clock, 45° = 1:30, and 60° = 2 o’clock.
Intercondylar clock-face (clock-face angle) description of the femoral tunnel. A line connected the distal edges of the medial and lateral femoral condyles. a Another line was parallel to the previous line through the top of the posterior intercondylar notch. b The midpoint was determined between the two points and a circle was drawn with this central point. The point of the circle touching the posterior intercondylar notch line was accepted as 12 o’clock and that passing through the medial and lateral femoral condyles line was accepted as 6 o’clock. c, d The centre of the femoral tunnel was marked as the cross-point of the intercondylar clock and the femoral tunnel extension of the 4 mm tunnel outside the joint to the lateral cortex. e The line connecting the centre of the clock and the cross-point above was expressed as time shown on the clock. f The angle between the drawn clock time and 12 o’clock was measured in degrees and designated as the clock-face angle
Statistical analysis
The SPSS statistical software (SPSS 19.0 for Windows, Inc., Chicago, IL, USA) was used for all statistical calculations. Continuous variables were given as mean ± standard deviation, medians (min–max); categorical variables were defined as percentages. Kolmogorov–Smirnov test was used to test for normal distribution. The Chi-square test was used for categorical variables among the groups. Two-sided t tests were used to analyse the differences in means and proportions between groups. Continuous variables among tunnel length groups were compared by ANOVA analysis. For post hoc analysis, Scheffe test was applied. The Pearson’s correlation coefficient was used for the analysis of the correlation between tunnel length and tunnel angle. Statistical significance was defined as P < 0.05.
Results
A total of 164 patients (10 female, 154 male) with a mean age of 29.6 ± 8.4 years (range, 15–52) were included in the analysis. A far medial accessory portal was used in 81 (49 %) operations and the transtibial technique was used in 83 (51 %) operations to drill the femoral tunnel. The mean femoral tunnel length was 42 ± 6.4 mm (range, 30–60) and the mean femoral tunnel clock-face angle was 41.1 ± 11.6 degrees (range, 20–72). In the correlation analysis, a strong negative correlation was determined between the tunnel length and femoral tunnel clock-face angle (rho = −0.829; p < 0.001). In other words, as the tunnel length increases, the tunnel angle decreases (Fig. 2). The mean tunnel length in far anteromedial portal technique was 38.1 ± 5 mm (range, 30–60) and as 45.8 ± 5.3 mm (range, 35–60) in the transtibial technique. The mean femoral tunnel clock-face angle was 49.8 ± 9.1 degrees (range, 20–72) (01:40 for left knee) in the far anteromedial portal technique and 32.6 ± 6.3 (range, 24–60) (01:00 for left knee) in the transtibial technique. In the transtibial technique, the tunnel angle was significantly decreased and the tunnel length was significantly increased (Table 1).
The patients were grouped according to tunnel length and statistically compared according to angles of 30°, 45° and 60° (1 o’clock, 1:30, and 2 o’clock, respectively, for the left knee; 1:30 and 2 o’clock are desirable coronal positions). The results are shown in Table 2. In 100 % (75/75) of patients with tunnel length of 40 mm and below the tunnel angle was 30° and above, in 81.3 % (61/75) of patients the tunnel angle was 45° and above and in 13.3 % (10/75) of patients, the tunnel angle was 60° and above.
In patients with tunnel length 41 mm and above, there was a 33.7 % likelihood of tunnel angle below 30°, there was a 92.1 % likelihood of tunnel angle below 45°, there was a 98.9 % likelihood of tunnel angle below 60°. When we analysed only transtibial group, in patients with tunnel length 41 mm and above, there was a 39.4 % likelihood of tunnel angle below 30°, there was a 98.6 % likelihood of tunnel angle below 45°, there was a 100 % likelihood of tunnel angle below 60°. We have also analysed only anteromedial portal group. In 100 % (63/63) of patients with tunnel length of 40 mm and below the tunnel angle was 30° and above, in 92 % (58/63) of patients the tunnel angle was 45° and above and in 14.3 % (9/63) of patients, the tunnel angle was 60° and above.
In other words for only transtibial group, in patients with tunnel length of 41 mm and below, there was a 25 % likelihood of tunnel angle above 45 degrees; for only anteromedial group in patients, tunnel length of 41 mm and below, there was a 92 % likelihood of tunnel angle above 45° and regardless of the technique used (both transtibial or anteromedial technique) in patients with tunnel length of 41 mm and above, there was a 92.1 % likelihood of tunnel angle below 45°.
Discussion
In this study, we aimed to find a critical femoral tunnel length measurement to estimate the proper femoral tunnel coronal plane angle. According to our analysis, in patients with tunnel length of 41 mm and above, there was a 92.1 % likelihood of tunnel angle below 45° regardless of the technique used (transtibial or far anteromedial technique). If you are using transtibial technique the possibility is even higher 98.6 %. Therefore, it will be beneficial to re-evaluate the femoral tunnel placement when the femoral tunnel is above 41 mm during the operation. This practical tip may help surgeons to avoid improper graft placement besides other methods and landmarks.
On the tibial side, during drilling the tibial tunnel the surgeon must pay attention to avoid an anterior position of the tunnel, which will lead to graft impingement with the roof of the notch during knee extension [16]. However, on the femoral side, minimal displacements at the femoral tunnel aperture may alter the graft orientation and tension significantly [1, 17]. It is known that vertical tunnel positioning in the femur only restores anteroposterior stability but not rotational stability. Placing the femoral tunnel at a more oblique angle may add rotational stability and more effectively resist rotational loads when compared to vertical tunnel placement [6, 7]. Therefore, surgeons should pay attention for the femoral tunnel drilling.
The clock-face representation is a widely used method to describe the anatomy of the intercondylar notch. This representation was originally intended to be a general description and it is being used without prior validation of its accuracy and reproducibility [12]. Steiner et al. [13] noted that two criteria are necessary to adequately describe the clock-face method: the knee flexion angle and transverse axis of the clock face. The majority of published studies fail to specify one or both of these criteria [7, 8, 10, 11, 18, 19]. Azzam et al. [12] compared the intra-observer and inter-observer reliability of the clock-face representation of the intercondylar notch and concluded that although there was a strong intraclass correlation coefficient, its reliability between surgeons is based on descriptions, thus resulting in a wide range of responses. Therefore, they recommended combining the clock-face representation with other descriptive methods for the intercondylar notch, such as footprints of the cruciate ligaments and other anatomic landmarks, resident’s ridge or lateral intercondylar ridge, the posterolateral rim, and the lateral bifurcate ridge. In addition, it should be keep in mind that there may be variations in the shape of the femoral notch and these anatomic variations may affect the clock-face evaluation [20]. In addition, ACL remnants on the lateral wall of the intercondylar notch which are used to determine the anatomic footprint may be lost in chronic cases. Measuring the femoral tunnel length will increase the success of these surgeons who estimate the clock-face angle.
Currently, the two femoral drilling techniques is often used. Group Mars [21] and Scopp [22] reported that the transtibial technique was not sufficient to open a more oblique femoral tunnel and the anteromedial portal gave a better result. In a cadaver study by Giron et al. [23] femoral tunnel opening with double incision and single incision transtibial technique and single incision anteromedial portal technique were compared and no difference of note was found between the three techniques. In the current study, while the mean femoral tunnel length was 45.8 mm and the mean femoral tunnel angle was 32.6° in the transtibial technique, the mean femoral tunnel length was 38.1 mm and the mean femoral tunnel angle was 49.8° in the tunnels opened with the anteromedial technique. Therefore the results of this study support the hypothesis that the anteromedial technique is necessary to be able to be closer to clock face 2 o’clock to be able to open a more oblique tunnel.
Lopez-Vidriero et al. [24] reported that 80 % of American orthopaedic surgeons perform fewer than 10 ACL reconstructions per year. It is important to stress that the anteromedial portal drilling technique is demanding and that the learning curve could be challenging, with a higher incidence of complications [25]. Surgeons with less experience could face more difficulties when beginning the anteromedial technique. According to Hohmann et al. [14] the observation of significant improvement in tunnel placement after 100 cases. Therefore, surgeons performing fewer than 20 ACL operations per year should confirm with more landmarks.
One of limitation of this study is that the measurements were made on direct radiographs. In several studies the difficulties of visualising bone tunnels on direct radiographs have been reported [26–28] and that radiographs taken in rotation will affect the measurements [29]. In the current study, the tunnels were seen better by taking the radiographs on postoperative second day and if rotation was detected, the radiographs were repeated. Secondly, the size of the femur may differ from patient to patient. Thus, a same coronal angle orientation of the graft may end with different femoral tunnel length in different femoral sizes. However, we have analysed a large population and presented the mean values. The strong aspects of this study were that the operations were all performed by a single surgeon who often performed anterior cruciate ligament surgery. This study is a prospective study and the radiographic measurements were made by three independent surgeons.
To understand whether the femoral tunnel is at the desired place during surgery may be difficult even for an experienced surgeon. Because the orientation of the femoral tunnel is significant in the success of ACL surgery, opening the tunnel according to the clock-face angle only may decrease the success of the surgery. It is absolutely necessary to use other non-related methods in addition to the intercondylar clock face. The length of the femoral tunnel may be included in these methods besides ACL footprint, ACL remnant and other anatomic landmarks. Measuring the length of the tunnel is a routine procedure and no extra effort is required. It should be kept in mind that when the tunnel is measured at 41 mm and above, there is a 92.1 % likelihood of clock-face angle orientation of less than 1:30.
References
Hefzy MS, Grood ES, Noyes FR (1989) Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med 17:208–216
Klos TV, Harman MK, Habets RJ, Devilee RJ, Banks SA (2000) Locating femoral graft placement from lateral radiographs in anterior cruciate ligament reconstruction: a comparison of 3 methods of measuring radiographic images. Arthroscopy 16:499–504
Musahl V, Plakseychuk A, Van Scyoc A, Sasaki T, Debski RE, McMahon PJ, Fu FH (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med 33:712–718
Markolf KL, Hame S, Hunter DM, Oakes DA, Zoric B, Gause P, Finerman GA (2002) Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 20:1016–1024
Rupp S, Muller B, Seil R (2001) Knee laxity after ACL reconstruction with a BPTB graft. Knee Surg Sports Traumatol Arthrosc 9:72–76
Bedi A, Raphael B, Maderazo A, Pavlov H, Williams RJ III (2010) Transtibial versus anteromedial portal drilling for anterior cruciate ligament reconstruction: a cadaveric study of femoral tunnel length and obliquity. Arthroscopy 26(3):342–350
Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H, Kim CH (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23(7):771–778
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement Richard O’Connor Award paper. Arthroscopy 19(3):297–304
Dargel J, Schmidt-Wiethoff R, Fischer S, Mader K, Koebke J, Schneider T (2009) Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc 17(3):220–227
Basdekis G, Abisafi C, Christel P (2008) Influence of knee flexion angle on femoral tunnel characteristics when drilled through the anteromedial portal during anterior cruciate ligament reconstruction. Arthroscopy 24:459–464
Golish SR, Baumfeld JA, Schoderbek RJ, Miller MD (2007) The effect of femoral tunnel starting position on tunnel length in anterior cruciate ligament reconstruction: a cadaveric study. Arthroscopy 23:1187–1192
Azzam MG, Lenarz CJ, Farrow LD, Israel H, Kieffer D, Kaar SG (2011) Inter- and intraobserver reliability of the clock face representation as used to describe the femoral intercondylar notch. Knee Surg Sports Traumatol Arthrosc 19(8):1265–1270
Steiner ME, Murray MM, Rodeo SA (2008) Strategies to improve anterior cruciate ligament healing and graft placement. Am J Sports Med 36:176–189
Hohmann E, Bryant A, Tetsworth K (2010) Tunnel positioning in anterior cruciate ligament reconstruction: how long is the learning curve? Knee Surg Sports Traumatol Arthrosc 18:1576–1582
Yamazaki J, Muneta T, Koga H, Sekiya I, Ju Y-J, Morito T et al (2011) Radiographic description of femoral tunnel placement expressed as intercondylar clock time in double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19:418–423
Howell SM, Taylor MA (1993) Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg Am 75(7):1044–1055
Zavras TD, Race A, Bull AM, Amis AA (2001) A comparative study of ‘isometric’ points for anterior cruciate ligament graft attachment. Knee Surg Sports Traumatol Arthrosc 9(1):28–33
Jepsen CF, Lundberg-Jensen AK, Faunoe P (2007) Does the position of the femoral tunnel affect the laxity or clinical outcome of the anterior cruciate ligament-reconstructed knee? A clinical, prospective, randomized, double-blind study. Arthroscopy 23:1326–1333
Rue JP, Ghodadra N, Lewis PB, Bach BR Jr (2008) Femoral and tibial tunnel position using a transtibial drilled anterior cruciate ligament reconstruction technique. J Knee Surg 21:246–249
van Eck CF, Martins CA, Vyas SM, Celentano U, van Dijk CN, Fu FH (2010) Femoral intercondylar notch shape and dimensions in ACL-injured patients. Knee Surg Sports Traumatol Arthrosc 18:1257–1262
Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38(10):1979–1986
Scopp JM, Jasper LE, Belkoff SM, Moorman CT III (2004) The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy 20(3):294–299
Giron F, Cuomo P, Aglietti P, Bill AMJ, Amis AA (2006) Femoral attachment of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14(3):250–256
Lopez-Vidriero E, Johnson D (2009) Evolving concepts in tunnel placement. Sports Med Arthrosc Rev 17:210–216
Lubowitz JH (2009) Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy 25:95–101
Khalfayan EE, Sharkey PF, Alexander AH, Bruckner JD, Bynum EB (1996) The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med 24:335–341
Lintner DM, Dewitt SE, Moseley JB (1996) Radiographic evaluation of native anterior cruciate ligament attachments and graft placement for reconstruction. A cadaveric study. Am J Sports Med 24:72–78
Sommer C, Friederich NF, Muller W (2000) Improperly placed anterior cruciate ligament grafts: correlation between radiological parameters and clinical results. Knee Surg Sports Traumatol Arthrosc 8:207–213
Giron F, Buzzi R, Aglietti P (1999) Femoral tunnel position in anterior cruciate ligament reconstruction using three techniques. A cadaver study. Arthroscopy 15:750–756
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Celiktas, M., Kose, O., Sarpel, Y. et al. Can we use intraoperative femoral tunnel length measurement as a clue for proper femoral tunnel placement on coronal plane during ACL reconstruction?. Arch Orthop Trauma Surg 135, 523–528 (2015). https://doi.org/10.1007/s00402-015-2173-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2173-2