Abstract
Purpose
Despite the widespread use of multivitamin/mineral supplements, the effects of multivitamin/mineral on cardiovascular disease (CVD) remain inconclusive. We aimed to prospectively investigate how multivitamin/mineral use is associated with CVD.
Methods
This population-based cohort study included 465,278 men and women who participated in the UK Biobank and were free from CVD at baseline. Participants were enrolled between 2006 and 2010 and followed-up until the end of 2018. Data on supplement use including multivitamin/mineral were collected using self-reported questionnaires. Cox proportional hazards models were used to estimate the hazard ratios of CVD events in relation to multivitamin/mineral use.
Results
During the follow-up, we identified 25,772 cases of CVD events, 4754 cases of CVD mortality, 18,728 cases of coronary heart disease, 6726 cases of myocardial infarction, and 4561 cases of stroke. The multivariable-adjusted hazard ratios associated with multivitamin/mineral use were 0.96 (95% CI: 0.93, 0.99) for CVD events, 0.92 (0.86, 1.00) for CVD mortality, 0.96 (0.93, 0.99) for coronary heart disease, and 0.92 (0.86, 0.97) for myocardial infarction. Subgroup analysis suggested that multivitamin/mineral use was associated with a significantly lower risk of CVD events in participants aged < 60 years and in former and current smokers (P for interaction ≤ 0.01). Sensitivity analyses showed no substantial change in the results when we excluded participants who developed CVD events during the first 2 years of follow-up.
Conclusion
Multivitamin/mineral supplementation was associated with very modest reductions in CVD events. Age and smoking might modify these associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The consumption of multivitamin/mineral supplements is common in developed countries because of the perception that they ensure an adequate nutrient intake and can prevent various chronic diseases, including cardiovascular disease (CVD) [1]. However, published results have not provided clear evidence of the potential cardiovascular benefits of multivitamin/mineral supplementation [2].
The Physicians’ Health Study (PHS) II, which was a randomized, controlled trial that tested daily multivitamin/mineral (Centrum Silver) use in CVD prevention, reported that this supplementation did not affect total CVD [3]. However, this study showed a significant reduction (by 39%) in fatal myocardial infarction (MI). Another randomized, controlled, supplementation trial called the SU.VI.MAX study evaluated the efficacy of nutritional doses of antioxidant vitamins and minerals, and indicated a significant interaction by sex for cancer incidence and all-cause mortality, that did not reach significance for CVD but still beared relevance [4]. The well-known limitations of these two trials make extrapolating these findings to the general population difficult [5].
Several large, population-based, observational studies have also reported inconsistent results regarding multivitamin/mineral use in CVD prevention [6,7,8,9,10,11,12]. A prospective cohort of Swedish women suggested a lower risk of MI in women with no history of CVD at baseline who were using multivitamins [6]. The Japan Collaborative Cohort study showed an inverse association of borderline statistical significance between multivitamin use and the risk of stroke mortality [7]. However, other observational studies showed no association of multivitamin/mineral use with the CVD incidence or mortality [8,9,10]. The above-mentioned studies were in homogeneous study populations (women [6, 8, 9] or men [10, 11] only) or investigated single CVD outcomes (MI [6], stroke [7], or CVD mortality [10, 12] only) with a limited sample size. These factors might have limited not only their generalizability, but also the ability to investigate the potential factors modifying the associations between multivitamin/mineral supplementation and total CVD outcomes.
Therefore, this prospective cohort study comprehensively examined the association between multivitamin/mineral supplement use and CVD outcomes in nearly half a million adults in the UK Biobank study. This study also further examined the potential modifying factors that might affect these associations.
Methods
Study design and participants
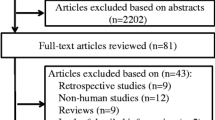
The UK Biobank is a large, population-based, prospective cohort study that aimed to investigate how different diseases are caused by the combination of lifestyle, environment, and genes [13]. The study design and population have been reported in detail previously [13]. Briefly, between 2006 and 2010, the UK Biobank study recruited more than half a million men and women aged 40–69 years at 22 assessment centers across England, Scotland, and Wales. Participants provided baseline information, physical measures, and biological samples, and were longitudinally followed-up for a wide range of health-related outcomes. In the current study, we excluded participants who withdrew from the study (n = 1298), those who had no available data on multivitamin/mineral supplements (n = 7295), and those with self-reported prior CVD (n = 28,634) at baseline. We included 465,278 participants in the final analysis (Fig. 1).
This study was performed under generic ethical approval obtained by UK Biobank investigators from the National Health Service National Research Ethics Service (Ref: 11/NW/0.0382) and all participants provided written informed consent. The current analyses were carried out under application number 52632.
Exposure assessment
At baseline, the habitual use of multivitamin/mineral supplements was recorded using a touch screen questionnaire. Participants were asked “Do you regularly take any of the following?” and could select their answers from a list of supplements, including multivitamins/minerals. We defined the habitual use of multivitamins/minerals as “1 = yes” or “0 = no.”
Ascertainment of outcomes
The primary outcome of this study was total CVD events, which comprised CVD mortality, coronary heart disease (CHD), and stroke. The secondary outcomes were individual CVD mortality, individual CHD events, MI events, and stroke events (ischemic and hemorrhagic stroke). The date and cause of death were identified by linking to death registries of the National Health Service Information Centre (England and Wales) and the National Health Service Central Register Scotland (Scotland). The date and cause of hospital admissions were identified through record linkage to Health Episode Statistics (England and Wales) and the Scottish Morbidity Records (Scotland). Detailed information on the linkage procedures can be found at http://content.digital.nhs.uk/services. At the time of the analysis, hospital admission data were available up to March 31, 2017, and we censored the disease-specific outcome analysis at this date or at the date of the first incidence of disease or death, whichever occurred first. Mortality data were available up to February 14, 2018. Therefore, we censored mortality analysis at this date or at date of death, whichever occurred first. The International Classification of Diseases, 10th Revision (ICD-10) codes were used to define CVD events in death and medical records. CHD was defined as ICD codes I20–I25. MI was defined as ICD codes I21, I22, I23, I24.1, or I25.2. Stroke was defined as ICD codes I60–I64 (ischemic stroke: code I63; hemorrhagic stroke: codes I60–I62). CVD mortality was defined as ICD codes I00–I99.
Covariates
The UK Biobank project used the baseline questionnaire to assess the following potential confounding variables: sociodemographic characteristics (age, sex, ethnicity, Townsend Deprivation Index, education, and gross annual household income), lifestyle behaviors (body mass index [BMI], smoking status, alcohol consumption, physical activity, and healthy diet [healthy diet score was evaluated by red meat intake ≤ 3 times each week, vegetable intake ≥ 4 tablespoons each day, fruit intake ≥ 3 pieces each day, fish intake ≥ 4 times each week, cereal intake ≥ 5 bowls each week, and urinary sodium concentration ≤ 70.6 mmol/L; one point was given for each favorable diet factor and the total diet score ranged from 0 to 6; a healthy diet was defined as a diet score ≥ 3] [14]), health conditions (hypertension, diabetes, high cholesterol concentrations, and longstanding illness), and drug use (antihypertensive drugs, insulin, aspirin, and lipid-lowering drugs).
The Townsend Deprivation Index is a composite measure of deprivation based on non-home ownership, non-car ownership, unemployment, and household overcrowding. This index represents the participant’s socioeconomic status and is provided directly by the UK Biobank [15, 16]. Education was coded as having received a degree (college/university degree) or no degree, and this information was derived from the questionnaire. BMI was calculated as the weight, measured to the nearest 0.1 kg using the Tanita BC-418 MA body composition analyzer (Tanita Corporation of America, IL), divided by the square of the height in meters, measured with a Seca 202 device (SECA, Hamburg, Germany). According to healthy physical activity recommendations [17], we categorized participants into < 150 or ≥ 150 min/week on the basis of the total time spent in moderate physical activity in minutes each week. Sodium concentrations were measured at the UK Biobank laboratory from stored baseline urine samples by ion selective electrode method using a Beckman Coulter AU5400. Baseline serum C-reactive protein was measured by immunoturbidimetric-high-sensitivity assay on a Beckman Coulter AU5800. Analytic range for urine sodium was 2–200 mmol/L and 0.08–80 mg/L for serum C-reactive protein. Blood pressure was measured twice with a digital sphygmomanometer (Omron 705 IT; OMRON Healthcare Europe B.V., Hoofddorp, Netherlands) or a manual sphygometer. The mean value of the two measurements were used to minimize measurement error. Information on the medical history (physician’s diagnosis of diabetes, high cholesterol, and longstanding illness) was collected by the self-completed baseline assessment questionnaire. Hypertension was defined as a self-reported history of hypertension, the use of antihypertensive drugs, a systolic blood pressure ≥ 140 mm Hg, or a diastolic blood pressure ≥ 90 mm Hg. Details of these assessments can be found on the UK Biobank website (www.ukbiobank.ac.uk).
Statistical analyses
Baseline characteristics are presented as the number (percentage) for categorical variables and the mean (standard deviation) for continuous variables. We used the chi-square test and Student’s t test to examine the participants’ characteristics according to whether they were users or non-users of multivitamin/mineral supplementation at baseline.
After verification of the proportional hazard assumption, Cox proportional hazard models were used to examine the associations between multivitamin/mineral supplementation and CVD outcomes (CVD events, CVD mortality, CHD, MI, or stroke). We fitted two sets of models. The basic model was adjusted for baseline age (years) and sex (male or female). The multivariable model was adjusted for the additional variables of ethnicity (white and others), the Townsend Deprivation Index, household income (< £18,000, £18,000–£30,999, £31,000–£51,999, £52,000–£100,000, or > £100,000), BMI (kg/m2), smoking status (never, former, or current), alcohol consumption (never, 1–2, 3–4, or ≥ 5 times/week), physical activity (< 150 or ≥ 150 min/week), healthy diet (yes or no), diabetes (yes or no), hypertension (yes or no), high cholesterol concentrations (yes or no), longstanding illness (yes or no), cholesterol-lowering medication (yes or no), antihypertensive drug use (yes or no), insulin treatment (yes or no), aspirin use (yes or no), and C-reactive protein concentrations (mg/L).
We performed subgroup analyses to estimate potential modification effects according to age (< 60 or ≥ 60 years), sex (male or female), obesity [yes (BMI ≥ 30 kg/m2) or no (BMI < 30 kg/m2)], healthy diet (yes or no), smoking status (never, former, or current), and physical activity (< 150 or ≥ 150 min/week). We assessed potential modifying effects by modeling the cross-product term of the stratifying variable with multivitamin/mineral supplementation. Furthermore, we conducted several sensitivity analyses to test the robustness of the results. First, we conducted sensitivity analyses by excluding participants who developed CVD events during the first 2 and 3 years of follow-up to minimize the effect of reverse causation. Second, because habitual use of multivitamin/mineral supplements was very likely to have strong association with habitual use of other supplements, we performed a sensitivity analysis by excluding participants who took any other supplements.
We performed multiple imputation for missing covariate data using the Markov chain Monte Carlo method. Detailed information on the number of missing covariates was shown in Supplemental Table S1. A two-tailed P value < 0.05 was considered statistically significant in all analyses. Statistical analysis was conducted using SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
Table 1 shows the baseline characteristics of the study participants stratified by multivitamin/mineral supplementation (users versus non-users). Of the 465,278 participants, 259,898 (55.9%) were women who had a mean age of 56.2 years. Overall, 103,687 (22.3%) participants reported habitual multivitamin/mineral supplementation at baseline. Multivitamin/mineral users were younger, and more likely to be women, not current smokers, drink less alcohol, and be physically active compared with non-users. Additionally, multivitamin/mineral users had a healthy diet, and had a lower prevalence of diabetes, hypertension, and high cholesterol concentrations, but had a higher prevalence of longstanding illness, compared with non-users. Multivitamin/mineral users were also less likely to take antihypertensive drugs, cholesterol-lowering medication, and insulin treatment, more likely to take aspirin, and had lower C-reactive protein than non-users.
Multivitamin/mineral use and outcomes
The median times to follow-up were 9.0 years (interquartile range: 8.3–9.7, totaling 4,190,751 person-years) for mortality outcomes and 8.1 years (interquartile range: 7.4–8.8, totaling 3,705,616 person-years) for CVD events. During the follow-up, we identified 25,772 cases of CVD events, 4754 cases of CVD mortality, 18,728 cases of CHD, 6726 cases of MI, and 4561 cases of stroke (3481 ischemic and 1249 hemorrhagic stroke). Table 2 shows the associations of habitual use of multivitamins/minerals with the outcomes. After adjusting for age and sex, we found significant inverse associations of multivitamin/mineral use with the risk of CVD events, CVD mortality, CHD, and MI (all P < 0.05). In the multivariable-adjusted models, the hazard ratios associated with multivitamin/mineral use were 0.96 (95% confidence interval: 0.93, 0.99) for CVD events, 0.92 (0.86, 1.00) for CVD mortality, 0.96 (0.93, 0.99) for CHD, and 0.92 (0.86, 0.97) for MI. However, we did not observe any significant associations between multivitamin/mineral use and stroke (hazard ratio 1.00; 95% confidence interval: 0.93, 1.07; P = 0.94), ischemic stroke (0.95; 0.88, 1.04; P = 0.25), or hemorrhagic stroke (1.13; 0.99, 1.29; P = 0.07).
Subgroup and sensitivity analyses
We conducted subgroup analyses according to potential risk factors (Fig. 2). Multivitamin/mineral use was associated with a significantly lower risk of total CVD events in participants aged < 60 years (P for interaction = 0.01) or previous and current smokers (P for interaction = 0.002). Sensitivity analyses showed no substantial change in the results when we excluded participants who developed CVD events during the first 2 years of follow-up (Table 3). After excluding participants who developed CVD events during the first 3 years of follow-up, we found a borderline inverse association between multivitamin/mineral use and lower risk of CVD events (Supplemental Tables S2). The association between multivitamin/mineral use and the risk of CVD events was abolished after excluding participants who took any other supplements (Table 4).
Association of multivitamin/mineral supplementation and the risk of cardiovascular events stratified by potential risk factors. Results were adjusted for age, sex, ethnicity (white and others), Townsend Deprivation Index, household income (< £18,000, £18,000–£30,999, £31,000–£51,999, £52,000–£100,000, or > £100,000), body mass index (kg/m2), smoking status (never, former, or current), alcohol consumption (never, 1–2, 3–4, or ≥ 5 times/week), physical activity (< 150 or ≥ 150 min/week), healthy diet (yes or no), diabetes (yes or no), hypertension (yes or no), high cholesterol (yes or no), longstanding illness (yes or no), cholesterol-lowering medication (yes or no), antihypertensive drug use (yes or no), insulin treatment (yes or no), and aspirin use (yes or no)
Discussion
In this large prospective study in the UK population, habitual multivitamin/mineral use was associated with very modest reductions in total CVD events, individual CVD mortality, CHD, and MI. Such associations were independent of traditional risk factors, which were baseline age, sex, ethnicity, the Townsend Deprivation Index, household income, BMI, smoking status, alcohol consumption, physical activity, healthy diet, major comorbidities, medicinal drug use, and C-reactive protein. The associations between the use of multivitamins/minerals and risks of CVD outcomes were modified by age and smoking. There was no substantial change in the results when we excluded participants who developed CVD events during the first 2 years of follow-up.
Several observational studies suggested inverse associations between multivitamin/mineral supplementation and CVD outcomes [6, 11, 18,19,20]. In a case–control study of Swedish residents aged 45–70 years, the odds ratios of MI were 0.79 (95% confidence interval: 0.63, 0.98) for men and 0.66 (95% confidence interval: 0.48, 0.91) for women when regular users of multivitamin supplements were compared with non-users [18]. A nationally representative, prospective sample of adults in the US using restricted data of the Third National Health and Nutrition Examination Survey showed that the use of multivitamins/minerals for > 3 years was significantly associated with a 35% lower risk of CVD mortality compared with non-users at a median 18-year follow-up [19]. However, the Nurses’ Health Study [8] and Women’s Health Study [9] showed that neither baseline nor time-varying multivitamin use was associated with the long-term risk of stroke. A systematic review and meta-analysis and its update of clinical trials and prospective cohort studies both demonstrated that multivitamin/mineral supplementation did not improve CVD outcomes in the general population [2, 21].
In this prospective study that included nearly half a million adults, we observed an extremely modest effect of multivitamin/mineral use on CVD events, only a few percent lower. Other vitamin and mineral supplement use fully attenuated the effects of multivitamin/mineral, demonstrating the importance of long-term clinical trials that can control for residual confounding when examining the health effects of this common supplement. Until then, even a very modest reduction in CVD for multivitamin/mineral supplement may still have public health impact. In subgroup analysis, there were consistent and significant interactions between multivitamin/mineral use and baseline age for CVD events, CHD, and MI. Multivitamin/mineral use was associated with a significantly lower risk of CVD outcomes in participants aged < 60 years than in those aged ≥ 60 years. Effect modification by age could be explained by the possibility that multivitamin/mineral use is more effective when initiated earlier in life to counter the initiation and progression of atherosclerosis, which often begins at an earlier age [22]. Furthermore, we found that the inverse associations between multivitamin/mineral use and CVD outcomes were significantly modified by smoking. Former and current smokers who took multivitamin/mineral supplementation had a lower risk of CVD outcomes. Former smokers include those who quit smoking due to illness. The lower risk observed for current smokers may be due to the fact that this particular subgroup consisted of those exposed to the potential confounding effect of smoking, and perhaps therefore be more prone to show the reverse association between multivitamin/mineral and CVD[23].
Multivitamin/mineral supplements typically contain a wide spectrum of low-dose essential vitamins and minerals that are obtained through a healthy diet [24]. Many of the included vitamins and minerals in supplements may play important roles in preventing development of CVD. Antioxidants, such as vitamin C, vitamin E, and carotenoids, may inhibit the oxidation of low-density lipoprotein cholesterol and thus mitigate the formation of atherosclerotic plaques[25, 26]. Supplements containing B vitamins may have protective effects on the risk of CVD via lowering of homocysteine concentrations[27, 28]. Previous evidence supports a role for vitamin D supplementation in maintaining cardiovascular health by inhibiting the development of atherosclerosis and improving endothelial function[29]. Endothelial selenoproteins are involved in protecting the cardiovascular system from different types of stress, including ischemia–reperfusion, homocysteine dysregulation, and myocardial hypertrophy [30]. Magnesium has vasodilatory, anti-inflammatory, anti-ischemic, and antiarrhythmic properties, therefore, it could be a useful therapeutic agent in cardiovascular medicine [31].
Strengths and limitations
The major strengths of our study include the large-scale, prospective study design, the long and practically complete follow-up, and the detailed information on socioeconomic characteristics, lifestyle, diet, and other covariates. Moreover, there were detailed data on various CVD outcomes, including CVD mortality, CHD, MI, and stroke. These advantages enabled us to comprehensively examine the potential role of multivitamin/mineral use on CVD outcomes. We acknowledge that our study also has potential limitations. First, the UK Biobank did not record detailed information on the use of multivitamin/mineral, such as formulation, dosage, frequency, and duration of use, limiting the ability to conduct more detailed analysis. Second, separating beneficial effects of multivitamin/mineral supplementation from effects due to healthy lifestyle habits was difficult. However, even when we controlled for known cardiovascular risk factors and performed stratified analyses to evaluate the associations in subgroups with different health behaviors, the observed weak association persisted. Third, potential reverse causality cannot be ruled out owing to the observational nature of the study. Finally, although we adjusted for several confounders in multivariable analysis, we cannot exclude the possibility of residual confounding. For example, the information on multivitamin/mineral use was only available at baseline. And measurement errors were inevitable because of the nature of the self-administrated questionnaire.
Conclusions
In this large-scale prospective study, we found that multivitamin/mineral supplementation was associated with very modest reductions in CVD events. Age and smoking might affect these associations. Long-term clinical trials are needed to address whether this common supplement affects CVD risk.
References
Neuhouser ML (2003) Dietary supplement use by American women: challenges in assessing patterns of use, motives and costs. J Nutr 133(6):1992s–1996s. https://doi.org/10.1093/jn/133.6.1992S
Kim J, Choi J, Kwon SY, McEvoy JW, Blaha MJ, Blumenthal RS, Guallar E, Zhao D, Michos ED (2018) Association of multivitamin and mineral supplementation and risk of cardiovascular disease: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 11(7):e004224. https://doi.org/10.1161/circoutcomes.117.004224
Sesso HD, Christen WG, Bubes V, Smith JP, MacFadyen J, Schvartz M, Manson JE, Glynn RJ, Buring JE, Gaziano JM (2012) Multivitamins in the prevention of cardiovascular disease in men: the Physicians’ Health Study II randomized controlled trial. JAMA 308(17):1751–1760. https://doi.org/10.1001/jama.2012.14805
Hercberg S, Galan P, Preziosi P, Bertrais S, Mennen L, Malvy D, Roussel AM, Favier A, Briançon S (2004) The SUVIMAX Study: a randomized, placebo-controlled trial of the health effects of antioxidant vitamins and minerals. Arch Intern Med 164(21):2335–2342. https://doi.org/10.1001/archinte.164.21.2335
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, LaVange L, Marinac-Dabic D, Marks PW, Robb MA, Shuren J, Temple R, Woodcock J, Yue LQ, Califf RM (2016) Real-world evidence—what is it and what can it tell us? N Engl J Med 375(23):2293–2297. https://doi.org/10.1056/NEJMsb1609216
Rautiainen S, Akesson A, Levitan EB, Morgenstern R, Mittleman MA, Wolk A (2010) Multivitamin use and the risk of myocardial infarction: a population-based cohort of Swedish women. Am J Clin Nutr 92(5):1251–1256. https://doi.org/10.3945/ajcn.2010.29371
Dong JY, Iso H, Kitamura A, Tamakoshi A (2015) Multivitamin use and risk of stroke mortality: the Japan collaborative cohort study. Stroke 46(5):1167–1172. https://doi.org/10.1161/strokeaha.114.008270
Adebamowo SN, Feskanich D, Stampfer M, Rexrode K, Willett WC (2017) Multivitamin use and risk of stroke incidence and mortality amongst women. Eur J Neurol 24(10):1266–1273. https://doi.org/10.1111/ene.13358
Rautiainen S, Lee IM, Rist PM, Gaziano JM, Manson JE, Buring JE, Sesso HD (2015) Multivitamin use and cardiovascular disease in a prospective study of women. Am J Clin Nutr 101(1):144–152. https://doi.org/10.3945/ajcn.114.088310
Messerer M, Håkansson N, Wolk A, Akesson A (2008) Dietary supplement use and mortality in a cohort of Swedish men. Br J Nutr 99(3):626–631. https://doi.org/10.1017/s0007114507812049
Rautiainen S, Rist PM, Glynn RJ, Buring JE, Gaziano JM, Sesso HD (2016) Multivitamin use and the risk of cardiovascular disease in men. J Nutr 146(6):1235–1240. https://doi.org/10.3945/jn.115.227884
Li K, Kaaks R, Linseisen J, Rohrmann S (2012) Vitamin/mineral supplementation and cancer, cardiovascular, and all-cause mortality in a German prospective cohort (EPIC-Heidelberg). Eur J Nutr 51(4):407–413. https://doi.org/10.1007/s00394-011-0224-1
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R (2015) UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12(3):e1001779. https://doi.org/10.1371/journal.pmed.1001779
Ma H, Li X, Sun D, Zhou T, Ley SH, Gustat J, Heianza Y, Qi L (2019) Association of habitual glucosamine use with risk of cardiovascular disease: prospective study in UK Biobank. BMJ (Clin Res ed) 365:l1628. https://doi.org/10.1136/bmj.l1628
Tyrrell J, Jones SE, Beaumont R, Astley CM, Lovell R, Yaghootkar H, Tuke M, Ruth KS, Freathy RM, Hirschhorn JN, Wood AR, Murray A, Weedon MN, Frayling TM (2016) Height, body mass index, and socioeconomic status: mendelian randomisation study in UK Biobank. BMJ (Clin Res ed) 352:i582. https://doi.org/10.1136/bmj.i582
Li ZH, Zhong WF, Liu S, Kraus VB, Zhang YJ, Gao X, Lv YB, Shen D, Zhang XR, Zhang PD, Huang QM, Chen Q, Wu XB, Shi XM, Wang D, Mao C (2020) Associations of habitual fish oil supplementation with cardiovascular outcomes and all cause mortality: evidence from a large population based cohort study. BMJ (Clin Res ed) 368:m456. https://doi.org/10.1136/bmj.m456
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, Dempsey PC, DiPietro L, Ekelund U, Firth J, Friedenreich CM, Garcia L, Gichu M, Jago R, Katzmarzyk PT, Lambert E, Leitzmann M, Milton K, Ortega FB, Ranasinghe C, Stamatakis E, Tiedemann A, Troiano RP, van der Ploeg HP, Wari V, Willumsen JF (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54(24):1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Holmquist C, Larsson S, Wolk A, de Faire U (2003) Multivitamin supplements are inversely associated with risk of myocardial infarction in men and women–Stockholm Heart Epidemiology Program (SHEEP). J Nutr 133(8):2650–2654. https://doi.org/10.1093/jn/133.8.2650
Bailey RL, Fakhouri TH, Park Y, Dwyer JT, Thomas PR, Gahche JJ, Miller PE, Dodd KW, Sempos CT, Murray DM (2015) Multivitamin-mineral use is associated with reduced risk of cardiovascular disease mortality among women in the United States. J Nutr 145(3):572–578. https://doi.org/10.3945/jn.114.204743
Watkins ML, Erickson JD, Thun MJ, Mulinare J, Heath CW Jr (2000) Multivitamin use and mortality in a large prospective study. Am J Epidemiol 152(2):149–162. https://doi.org/10.1093/aje/152.2.149
Jenkins DJA, Spence JD, Giovannucci EL, Kim YI, Josse RG, Vieth R, Sahye-Pudaruth S, Paquette M, Patel D, Blanco Mejia S, Viguiliouk E, Nishi SK, Kavanagh M, Tsirakis T, Kendall CWC, Pichika SC, Sievenpiper JL (2021) Supplemental vitamins and minerals for cardiovascular disease prevention and treatment: JACC focus seminar. J Am Coll Cardiol 77(4):423–436. https://doi.org/10.1016/j.jacc.2020.09.619
Salonen RM, Nyyssönen K, Kaikkonen J, Porkkala-Sarataho E, Voutilainen S, Rissanen TH, Tuomainen TP, Valkonen VP, Ristonmaa U, Lakka HM, Vanharanta M, Salonen JT, Poulsen HE (2003) Six-year effect of combined vitamin C and E supplementation on atherosclerotic progression: the Antioxidant Supplementation in Atherosclerosis Prevention (ASAP) Study. Circulation 107(7):947–953. https://doi.org/10.1161/01.cir.0000050626.25057.51
Messner B, Bernhard D (2014) Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol 34(3):509–515. https://doi.org/10.1161/atvbaha.113.300156
Rautiainen S, Wang L, Lee IM, Manson JE, Gaziano JM, Buring JE, Sesso HD (2016) Multivitamin use and the risk of hypertension in a prospective cohort study of women. J Hypertens 34(8):1513–1519. https://doi.org/10.1097/hjh.0000000000000973
Steinberg D, Witztum JL (2002) Is the oxidative modification hypothesis relevant to human atherosclerosis? Do the antioxidant trials conducted to date refute the hypothesis? Circulation 105(17):2107–2111. https://doi.org/10.1161/01.cir.0000014762.06201.06
Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 352(16):1685–1695. https://doi.org/10.1056/NEJMra043430
Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis (2002). JAMA 288(16):2015–2022. doi:https://doi.org/10.1001/jama.288.16.2015
McNulty H, Pentieva K, Hoey L, Ward M (2008) Homocysteine, B-vitamins and CVD. Proc Nutr Soc 67(2):232–237. https://doi.org/10.1017/s0029665108007076
McGreevy C, Williams D (2011) New insights about vitamin D and cardiovascular disease: a narrative review. Ann Intern Med 155(12):820–826. https://doi.org/10.7326/0003-4819-155-12-201112200-00004
Rose AH, Hoffmann PR (2015) Selenoproteins and cardiovascular stress. Thromb Haemost 113(3):494–504. https://doi.org/10.1160/th14-07-0603
Muñoz-Castañeda JR, Pendón-Ruiz de Mier MV, Rodríguez M, Rodríguez-Ortiz ME (2018) Magnesium replacement to protect cardiovascular and kidney damage? Lack of prospective clinical trials. Int J Mol Sci. https://doi.org/10.3390/ijms19030664
Acknowledgements
We thank UK Biobank participants. This research has been conducted using the UK Biobank Resource (application No 52632).
Funding
This study is supported by the National Natural Science Foundation of China (82173648), Innovative Talent Support Plan of the Medical and Health Technology Project in Zhejiang Province (2021422878), Internal Fund of Ningbo Institute of Life and Health Industry, University of Chinese Academy of Sciences (2020YJY0212), Ningbo Clinical Research Center for Digestive System Tumors (2019A21003), and Sanming Project of Medicine in Shenzhen (SZSM201803080).
Author information
Authors and Affiliations
Contributions
LH and YZ: conceptualized the manuscript; BC, CZ, and LH: contributed to the literature search and interpretation, the statistical analysis, the writing of the paper, and refining of figures and tables; RZ and MW: conducted the data collection; LH and YZ had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; and all authors: reviewed and revised the manuscript, read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was performed under generic ethical approval obtained by UK Biobank investigators from the National Health Service National Research Ethics Service (Ref: 11/NW/0.0382) and all participants provided written informed consent. The current analyses were carried out under application number 52632.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Che, B., Zhong, C., Zhang, R. et al. Multivitamin/mineral supplementation and the risk of cardiovascular disease: a large prospective study using UK Biobank data. Eur J Nutr 61, 2909–2917 (2022). https://doi.org/10.1007/s00394-022-02865-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02865-4