Abstract
Purpose
The anti-glycative and anti-oxidative effects from Houttuynia cordata leaves aqueous extract (HCAE) in heart and kidney of diabetic mice were examined.
Methods
HCAE, at 1 or 2 %, was supplied in drinking water for 8 weeks. Plasma glucose and blood urea nitrogen (BUN) levels and creatine phosphokinase (CPK) activity were measured. The production of oxidative and inflammatory factors was determined. Activity and protein expression of associated enzymes or regulators were analyzed.
Results
HCAE intake at both doses lowered plasma glucose and BUN levels, and CPK activity and also restored creatinine clearance rate in diabetic mice. HCAE intake, only at 2 %, retained plasma insulin levels (P < 0.05). HCAE reduced reactive oxygen species, protein carbonyl, interleukin-6, tumor necrosis factor-alpha, N ε-(carboxymethyl)-lysine, pentosidine and fructose levels, and reserved glutathione content in heart and kidney of diabetic mice (P < 0.05). Diabetes enhanced aldose reductase (AR) activity and protein expression in heart and kidney (P < 0.05). HCAE intake at both doses decreased renal AR activity and protein expression, but only at 2 % lowered cardiac AR activity and protein expression (P < 0.05). Diabetes increased protein expression of RAGE, p47phox and gp91phox, nuclear factor kappa-B (NF-κB) p50, NF-κB p65 and mitogen-activated protein kinase in heart and kidney (P < 0.05). HCAE intake only at 2 % limited RAGE expression, but at 1 and 2 % downregulated p47phox, NF-κB p65 and p-p38 expression in these organs (P < 0.05).
Conclusions
These findings suggest that Houttuynia cordata leaves aqueous extract could ameliorate cardiac and renal injury under diabetic condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperglycemia enhances polyol pathway for glucose metabolism, and aldose reductase (AR) is the rate-limiting enzyme in this pathway [1, 2]. AR metabolizes glucose to sorbitol, which is further converted to fructose. Excessive glucose and fructose occurred in diabetic condition promote the generation of advanced glycation endproducts (AGEs). AGEs and their modified derivatives cause cellular damage and organ malfunctions, and even elicit diabetic complications [3, 4]. N ε-(carboxymethyl)-lysine (CML) and pentosidine are predominant AGEs contributing to the occurrence of diabetic complications like diabetic cardiomyopathy and nephropathy in diabetic patients [5, 6]. Therefore, glycative stress could be diminished by inhibiting AR and decreasing AGEs production. In addition, AGEs upregulate their membrane-anchored receptor (RAGE), and the RAGE–AGE interaction evokes intracellular reactive oxygen species (ROS) generation and activates mitogen-activated protein kinase (MAPK) and nuclear factor kappa-B (NF-κB) signaling pathways [7, 8]. The activation of both pathways further accelerates diabetic deterioration via increasing the formation of glycative, oxidative, inflammatory and fibrotic factors. Thus, the suppression on RAGE, NF-κB and/or MAPK pathways may benefit diabetic prevention and/or attenuation.
Houttuynia cordata Thumb is traditionally applied as a medicinal plant in Asian countries including China, Japan and Taiwan [9]. Wang et al. [10] reported that this plant was used to treat several symptoms such as clearing heat, eliminating carbuncle, detoxification and promoting diuresis. Furthermore, those authors indicated that the decoction of this plant protected renal tissue of diabetic rats through reducing protein expression of transforming growth factor-beta1 [10]. The study of Kumar et al. [11] revealed that ethanol extract prepared from whole plant of H. cordata exhibited anti-hyperglycemic effect in diabetic mice via raising antioxidant activity and glucose transporters. Those previous studies already suggest that H. cordata could provide antidiabetic activity. On the other hand, the fresh leaf part of this plant is consumed as a vegetable in China [12]. Our previous study found that the aqueous extract of H. cordata leaves contained many phenolic acids and flavonoids such as kaempferol, quercetin, myricetin, ellagic acid, ferulic acid and gallic acid, and the intake of this extract protected mice against high saturated fat diet-induced obesity, hepatic inflammatory and oxidative injury [13]. So far, the antidiabetic and antiglycative effects as well as the action modes of the aqueous extract prepared from H. cordata leaves remain unknown. Furthermore, heart and kidney are two organs more vulnerable to diabetes. Thus, the antidiabetic protection for these organs seems relatively more important.
The major purpose of this study was to examine the antiglycative effects of aqueous extract of H. cordata leaves in heart and kidney of diabetic mice. The effects of this extract upon the production of AGEs and ROS as well as the activity and/or protein expression of AR, RAGE, NF-κB and MAPK were also evaluated. These results could provide evidence regarding the application of H. cordata leaves aqueous extract as a medicinal supplement against diabetes.
Materials and methods
Materials
Fresh H. cordata leaves were obtained from Nantou County, Taiwan, in 2012. H. cordata leaves aqueous extract (HCAE) was made by mixing 50 g chopped fresh leaves and 150 ml distilled water, homogenizing for 1 min in a Waring blender and cooking for 15 min at 100 °C. After filtrating through a filter paper, the filtrate was then freeze-dried to a powder. Our previous study indicated that the content of total phenolic acid and total flavonoid in HCAE was 2175 ± 210 and 1766 ± 182 mg/100 g dry weight, respectively. In order to standardize HCAE, the content of both total phenolic acid and total flavonoid in HCAE used in the present study was analyzed by the methods of Singleton et al. [14] and Zhishen et al. [15]. HCAE powder at 1 or 2 g was further mixed with 99 or 98 ml double-distilled water to prepare 1 or 2 % HCAE drinking water for experiments.
Animals and diets
Male 3-week-old Balb/cA mice were purchased from National Laboratory Animal Center (National Science Council, Taipei City, Taiwan). Mice with 22.7 ± 0.6 g body weight were treated with a single i.v. injection of streptozotocin (50 mg/kg) into the tail vein of mice after 12 h fast to induce diabetes. Blood glucose levels were measured on day 10 from the tail vein by a one-touch blood glucose meter (Lifescan Inc., Milpitas, CA, USA) after 12 h fast. Mice with fasting blood glucose levels ≥200 mg/dl were used. Animal experiments were performed in accordance with protocols approved by the Animal Care Research Committee of China Medical University (102-36-N).
Experimental design
After diabetes has been induced, mice were divided into three groups (10 mice/group): diabetic mice with 0, 1 or 2 % HCAE treatment. In addition, two groups of nondiabetic mice were also used, in which 0 (control) or 2 % HCAE was supplied. All mice were free to access food and water at all times. Consumed feed and water volume were recorded. Body weight and plasma glucose levels were measured weekly. Urine was collected for 24 h from mice in metabolic cages. After 8 weeks of supplementation, mice were fasted for 12 h and treated with carbon dioxide. Blood, heart and kidney from each mouse were collected. Protein concentration of cardiac or renal homogenate was determined by an assay kit purchased from Pierce Biotechnology Inc. (Rockford, IL, USA).
Blood and urinary analyses
Plasma glucose levels were measured by glucose HK kit bought from Sigma Chemical Co. (St. Louis, MO, USA). Plasma insulin levels were measured by insulin radioimmunoassay kit (Linco Research Inc., St. Charles, MO, USA). Plasma creatine phosphokinase (CPK) activity was assayed by an ELISA kit (Randox, UK). Plasma blood urea nitrogen (BUN), plasma and urinary creatinine concentrations were measured by a Beckman Autoanalyzer (Beckman Coulter, Fullerton, CA, USA). Creatinine clearance rate (CCr) was calculated according to a Cockcroft-Gault formula: [urinary volume (ml) × urinary creatinine (mg/dl)]/[plasma creatinine (mg/dl) × urine collection length (min)]. Results were expressed as ml/min/100 g body weight. Glycated albumin level was analyzed by chromatography on phenylboronate agarose for the separation of nonglycated from glycated albumin by eluting the glycated fraction with 0.35 mol/l sorbitol.
Measurement of CML, pentosidine and fructose levels
Cardiac or renal tissue was homogenized and digested with proteinase K (1 mg/ml) for 3 h at 37 °C and followed by adding 2 mmol/l phenylmethylsulfonyl fluoride to stop reaction. CML was determined by a competitive ELISA kit purchased from Roche Diagnostics (Penzberg, Germany) with 4G9, a CML-specific monoclonal antibody. Absorbance at 405 nm was read in a microtiter Bio-Rad plate reader (Hercules, CA, USA). Pentosidine levels were analyzed by a HPLC method described by Miyata et al. [16]. Sample was lyophilized and hydrolyzed in 500 µl of 6 N HCl at 110 °C for 16 h. NaOH was used for neutralization, and sample was used for HPLC measurement. HPLC (Waters, Tokyo, Japan) equipped with a fluorescence detector and a C18 reverse-phase column was used, and excitation and emission wavelength was set at 335 and 385 nm, respectively. In addition, 50 mg of heart or kidney was homogenized with phosphate buffer containing U-[13C]-sorbitol as an internal standard. After protein precipitation and centrifugation, the supernatant was lyophilized. Fructose content in lyophilized sample was assayed by liquid chromatography according to the method of Guerrant and Moss [17].
Assay of AR activity
The method of Nishinaka and Yabe-Nishimura [18] was used to determine AR activity. d/l-glyceraldehyde was sued as a substrate. The decrease in absorbance at 340 nm was monitored to reflect NADPH oxidation.
Measurement of ROS, glutathione (GSH), protein carbonyl, interleukin (IL)-6 and tumor necrosis factor (TNF)-alpha levels
Cardiac or renal tissue was homogenized with cold phosphate buffer containing 1 mM EDTA and 0.05 % Tween. An oxidation-sensitive dye, 2′,7′-dichlorofluorescein diacetate (DCFH-DA), was used to determine ROS level. Briefly, 500 μl of homogenate was mixed with 500 μl of 2 mg/ml DCFH-DA for 30 min. Fluorescence at 488 nm excitation and 525 nm emission was recorded by a fluorescence plate reader. Results are expressed as relative fluorescence unit (RFU) per mg protein. GSH concentration was quantified by a colorimetric glutathione kit purchased from OxisResearch Co. (Portland, OR, USA). Protein carbonyls were analyzed by the Zentech PC kit bought from BioCell Chem. Co. (Auckland, New Zealand). Briefly, 50 µl of tissue homogenate was blended with a 200 μl dinitrophenylhydrazine (DNP) solution. Then, adsorbed DNP-protein reacted with an anti-DNP-biotin antibody, and the absorbance at 450 nm was measured. IL-6 and TNF-alpha levels in heart or kidney homogenate were measured using ELISA kits purchased from R&D Systems (Minneapolis, MN, USA).
Western blot analyses
Cardiac or renal tissue, 40 mg, was homogenized in buffer containing protease inhibitor cocktail purchased from Sigma-Aldrich Chemical Co. (St. Louis, MO, USA) and 0.5 % Triton X-100. Homogenate was then mixed with buffer (60 mmol/L Tris–HCl, 2 % β-mercaptoethanol and 2 % SDS, pH 7.2) and followed by boiling for 5 min. Protein sample at 40 μg was electrophoresed on 10 % SDS-polyacrylamide gel and further transferred onto nitrocellulose membranes (Millipore, Bedford, MA, USA) for 1 h. After blocking with a protein solution containing 5 % skim milk for 1 h, membranes were treated with monoclonal antibody (Boehringer-Mannheim, Indianapolis, IN, USA) against RAGE (1:500), AR, p47phox, gp91phox, NF-κB p50, NF-κB p65 (1:1000) and MAPK (1:2000) at 4 °C overnight, and followed by incubating with horseradish peroxidase-conjugated antibody at room temperature for 3.5 h. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a loading control, and the bands were quantified by an ATTO image analyzer (Tokyo, Japan).
Statistical analysis
Each group had ten mice (n = 10). All data were expressed as mean ± standard deviation (SD). Statistical analysis was processed by one-way ANOVA. Post hoc comparisons were carried out by Dunnet’s t test. Statistical significance was considered at p value <0.05.
Results
Effect of HCAE on diabetic characteristics
HCAE intake at 2 % did not change body weight, water intake, feed intake, urine output, heart weight and kidney weight in normal mice (Table 1, P > 0.05). Diabetes significantly decreased body weight and increased water intake, feed intake and urine output (P ≤ 0.01); however, diabetic mice with HCAE intake at both doses had significantly higher body weight (P = 0.009 and 0.037), lower water intake (P = 0.025 and 0.031), lower feed intake (P = 0.045 and 0.043) and less urine volume (P = 0.013 and 0.02). As shown in Table 2, diabetes raised plasma glucose and BUN levels, and CPK activity, but decreased plasma insulin and CCr levels (P ≤ 0.009). HCAE intake at both doses reduced plasma levels of glucose (P = 0.01 and 0.03) and BUN (P = 0.011 and 0.037), and CPK activity (P = 0.008 and 0.015) and also restored CCr levels (P = 0.01 and 0.042) in diabetic mice. HCAE intake, only at 2 %, retained the insulin level (P = 0.029).
Effects of HCAE on oxidative, inflammatory and glycative factors
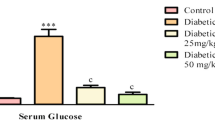
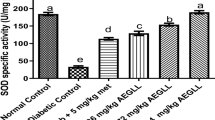
Diabetes increased ROS, protein carbonyl, IL-6 and TNF-alpha levels, but lowered GSH content in heart and kidney (Table 3, P ≤ 0.002). HCAE intake decreased cardiac levels of ROS (P = 0.009 and 0.039), protein carbonyl (P = 0.007 and 0.021), IL-6 (P = 0.01 and 0.035) and TNF-alpha (P = 0.008 and 0.016), and retained GSH content (P = 0.01 and 0.041). HCAE intake at both doses also reduced renal levels of ROS (P = 0.01 and 0.043), protein carbonyl (P = 0.008 and 0.019), IL-6 (P = 0.01 and 0.023) and TNF-alpha (P = 0.007 and 0.017), and retained GSH content (P = 0.006 and 0.025). Diabetes increased CML, pentosidine and fructose levels in heart and kidney and also raised urinary glycative albumin level (Table 4, P ≤ 0.001). HCAE intake lowered the generation of CML (P = 0.008 and 0.029), pentosidine (P = 0.01 and 0.036) and fructose (P = 0.009 and 0.018) in heart. HCAE intake at 1 or 2 % also decreased renal level of CML (P = 0.01 and 0.021), pentosidine (P = 0.011 and 0.04), fructose (P = 0.009 and 0.023) and urinary glycative albumin level (P = 0.01 and 0.042). As shown in Fig. 1, diabetes enhanced AR activity and protein expression in heart and kidney (P < 0.05). HCAE intake at both doses decreased renal AR activity and protein expression and only at 2 % lowered cardiac AR activity and expression (P < 0.05).
Effects of HCAE on expression of RAGE, NADPH oxidase, NF-κB and MAPK
Diabetes promoted protein expression of RAGE, p47phox and gp91phox in heart and kidney (Fig. 2, P < 0.05). HCAE intake only at 2 % limited RAGE expression in both organs, but at 1 and 2 % lowered p47phox expression in these organs (P < 0.05). HCAE intake did not affect gp91phox expression (P > 0.05). Diabetes also upregulated cardiac and renal expression of NF-κB p50, NF-κB p65 and MAPK (Fig. 3, P < 0.05). HCAE intake at both doses downregulated NF-κB p65 and p-p38 expression in two organs (P < 0.05).
Discussion
The effects of H. cordata upon glycemic control and renal protection in diabetic animals have been reported [11, 12]. However, decoction of crude H. cordata was used by Wang et al. [11], while Kumar et al. [12] used ethanol extract prepared from whole plant of H. cordata. In our present study, the aqueous extract of H. cordata leaves was used, and our data revealed that the intake of this extract decreased plasma glucose, BUN and CPK levels or activity, retained plasma insulin level and raised CCr in diabetic mice. These novel findings suggest that the aqueous extract of H. cordata leaves could exhibit antidiabetic activity. Furthermore, we found that this extract repressed polyol, NF-κB and MAPK pathways in heart and kidney of diabetic mice, which consequently diminished the formation of glycative, inflammatory and oxidative factors including AGEs, ROS and inflammatory cytokines in these two organs. These data support that H. cordata leaves aqueous extract could provide multiple protective actions against diabetic deterioration.
Hyperglycemia enhances oxidative and inflammatory stress, which contribute to the development of diabetic cardiomyopathy and/or nephropathy [19, 20]. In our present study, diabetes caused overproduction of ROS, protein carbonyl, IL-6 and TNF-alpha in heart and kidney. These findings agreed those previous studies and indicated that these two organs were vulnerable to diabetes. NADPH oxidase complex plays an important role in diabetes-induced ROS generation [21, 22]. We examined the influence of aqueous extract of H. cordata leaves upon the expression of p47phox and gp91phox, NADPH oxidase cytosolic and membrane components, and our data revealed that this extract effectively downregulated cardiac and renal protein expression of p47phox, which in turn led to lower ROS production and spared GSH content in both organs. These findings suggest that aqueous extract of H. cordata leaves could mitigate diabetes elicited cardiac and renal oxidative injury via regulating NADPH oxidase. ROS is a stimulator for the formation of inflammatory cytokines like IL-6 and TNF-alpha [23]. Thus, the less ROS level in heart and kidney of mice treated with aqueous extract of H. cordata leaves subsequently ameliorated inflammatory stress. Consequently, the lower IL-6 and TNF-alpha levels in heart and kidney were observed. In addition, hyperglycemia and ROS are crucial activators for signal transduction cascades of NF-κB and MAPK [20, 24], and the activation of both pathways facilitates the production of inflammatory cytokines and oxidants. Our results revealed that the intake of aqueous extract from H. cordata leaves markedly limited protein expression of NF-κB p65 and p-p38 in heart and kidney of diabetic mice, which in turn decreased inflammatory cytokines in these organs. These results suggest that aqueous extract of H. cordata leaves was able to mediate NF-κB and MAPK signaling pathways under diabetic condition.
CML, pentosidine and urinary glycated albumin are indicators of diabetes associated with glycative stress, especially in patients with elevated risk of diabetic cardiomyopathy and/or nephropathy because the accumulation of these AGEs in organs impairs their functions [25, 26]. The activated polyol pathway, mainly due to enhanced activity and expression of aldose reductase, promotes AGEs formation [27, 28]. In this study, H. cordata leaves aqueous extract substantially reduced both activity and protein expression of this enzyme in heart and kidney, which subsequently decreased fructose flux and finally reduced CML, pentosidine and urinary glycated albumin production. These findings indicated that this extract attenuated cardiac and renal glycative stress by repressing polyol pathway. In addition, we found this extract at 2 % downregulated RAGE expression in two organs. The suppression on RAGE expression definitely contributed to mitigate glycative stress in these tissues by inhibiting the de novo synthesis of AGEs. On the other hand, the engagement of AGEs and RAGE benefits NF-κB and MAPK pathways activation and consequently accelerates the formation of glycative, oxidant, inflammatory and coagulant factors [29, 30]. Because the available RAGE has been reduced by H. cordata leaves aqueous extract, the interaction between AGEs and RAGE could be substantially suppressed. Thus, the less AGEs and ROS levels, as well as the limited NF-κB p65 and p-p38 expression in heart and kidney of diabetic mice, could be partially ascribed to this extract and downregulate RAGE in these organs. Since oxidative, inflammatory and glycative injuries in these organs of diabetic mice have been alleviated, the observed improvement in cardiac and renal functions, evidenced by the changes in CPK activity, BUN and CCr levels in those diabetic mice, could be explained.
Our previous study reported that aqueous extract of H. cordata leaves was rich in phytochemicals, and the content of kaempferol, myricetin, quercetin, ferulic acid, ellagic acid or gallic acid was in the range of 104–245 mg/100 g dry weight [13]. So far, the antidiabetic and even antiglycative effects of kaempferol, ferulic acid and/or gallic acid have been reported [31–34]. Therefore, it seems highly possible that these compounds presented in this extract of H. cordata leaves executed the observed antidiabetic protection. Furthermore, our previous study found that this extract contained other compounds such as naringenin, rutin and rosmarinic acid, although at relatively lower amount, in the range of 62–94 mg/100 g dry weight. Certainly, the contribution from these compounds for antidiabetic actions of this extract should not be ignored. H. cordata is commonly used as a vegetable or for medicinal purpose in Asia. Our previous and present studies supported that the aqueous extract from the leaf part of this plant benefited liver, heart and kidney protection. Thus, H. cordata leaves aqueous extract could be developed as a supplement for health promotion. However, further human study is necessary to verify the safety and effects of this extract.
In conclusion, the intake of H. cordata leaves aqueous extract attenuated glycative, oxidative and inflammatory stress in heart and kidney of diabetic mice through mediating NADPH oxidase, aldose reductase, RAGE, NF-κB and MAPK. These findings suggest that H. cordata leaves aqueous extract may benefit diabetic prevention and/or alleviation.
Abbreviations
- AGEs:
-
Advanced glycation endproducts
- AR:
-
Aldose reductase
- BUN:
-
Blood urea nitrogen
- CCr:
-
Creatinine clearance rate
- CML:
-
N ε-(carboxymethyl)-lysine
- CPK:
-
Creatine phosphokinase
- Cr:
-
Creatinine
- DCFH-DA:
-
2′,7′-Dichlorofluorescein diacetate
- DNP:
-
Dinitrophenylhydrazine
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GSH:
-
Glutathione
- HCAE:
-
Houttuynia cordata leaves aqueous extract
- IL:
-
Interleukin
- MAPK:
-
Mitogen-activated protein kinase
- NF-κB:
-
Nuclear factor kappa-B
- RFU:
-
Relative fluorescence unit
- ROS:
-
Reactive oxygen species
- TNF-alpha:
-
Tumor necrosis factor-alpha
References
Dunlop M (2000) Aldose reductase and the role of the polyol pathway in diabetic nephropathy. Kidney Int Suppl 77:S3–S12
Chung SS, Ho EC, Lam KS, Chung SK (2003) Contribution of polyol pathway to diabetes-induced oxidative stress. J Am Soc Nephrol 14:S233–S236
Peyroux J, Sternberg M (2006) Advanced glycation endproducts (AGEs): pharmacological inhibition in diabetes. Pathol Biol 54:405–419
Vlassara H, Striker GE (2013) Advanced glycation endproducts in diabetes and diabetic complications. Endocrinol Metab Clin North Am 42:697–719
Hirata K, Kubo K (2004) Relationship between blood levels of N-carboxymethyl-lysine and pentosidine and the severity of microangiopathy in type 2 diabetes. Endocr J 51:537–544
Ghanem AA, Elewa A, Arafa LF (2011) Pentosidine and N-carboxymethyl-lysine: biomarkers for type 2 diabetic retinopathy. Eur J Ophthalmol 21:48–54
Barlovic DP, Thomas MC, Jandeleit-Dahm K (2010) Cardiovascular disease: what’s all the AGE/RAGE about? Cardiovasc Hematol Disord Drug Targets 10:7–15
Xie J, Méndez JD, Méndez-Valenzuela V, Aguilar-Hernández MM (2013) Cellular signalling of the receptor for advanced glycation end products (RAGE). Cell Signal 25:2185–2197
Meng J, Leung KS, Jiang Z, Dong X, Zhao Z, Xu LJ (2005) Establishment of HPLC-DAD-MS fingerprint of fresh Houttuynia cordata. Chem Pharm Bull 53:1604–1609
Wang F, Lu F, Xu L (2007) Effects of Houttuynia cordata thumb on expression of BMP-7 and TGF-beta1 in the renal tissues of diabetic rats. J Tradit Chin Med 27:220–225
Kumar M, Prasad SK, Krishnamurthy S, Hemalatha S (2014) Antihyperglycemic activity of Houttuynia cordata Thunb. in streptozotocin-induced diabetic rats. Adv Pharm Sci 2014:809438
Guan JZ, Wang JJ, Cheng ZH, Liu Y, Li ZY (2012) Cytomixis and meiotic abnormalities during microsporogenesis are responsible for male sterility and chromosome variations in Houttuynia cordata. Genet Mol Res 11:121–130
Lin MC, Hsu PC, Yin MC (2013) Protective effects of Houttuynia cordata aqueous extract in mice consuming a high saturated fat diet. Food Funct 4:322–327
Singleton VL, Orthofer R, Lamuela-Raventos RM (1999) Analysis of total phenols and other oxidation substrates and antioxidants by means of Folin Ciocalteu reagent. Methods Enzymol 299:152–178
Zhishen J, Mengcheng T, Jianming W (1999) The determination of flavonoid content in mulberry and their scavenging effects on superoxide radicals. Food Chem 64:555–559
Miyata T, Taneda S, Kawai R, Ueda Y, Horiuchi S, Hara M, Maeda K, Monnier VM (1996) Identification of pentosidine as a native structure for advanced glycation end products in β-2-microglobulin-containing amyloid fibrils in patients with dialysis-related amyloidosis. Proc Natl Acad Sci USA 93:2353–2358
Guerrant G, Moss CW (1984) Determination of monosaccharides as aldononitrile, O-methyloxime, alditol, and cyclitol acetate derivatives by gas chromatography. Anal Chem 56:633–638
Nishinaka T, Yabe-Nishimura C (2001) EGF receptor-ERK pathway is the major signaling pathway that mediates upregulation of aldose reductase expression under oxidative stress. Free Radic Biol Med 31:205–216
Fiorentino TV, Prioletta A, Zuo P, Folli F (2013) Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr Pharm Des 19:5695–5703
Palomer X, Salvadó L, Barroso E, Vázquez-Carrera M (2013) An overview of the crosstalk between inflammatory processes and metabolic dysregulation during diabetic cardiomyopathy. Int J Cardiol 168:3160–3172
Gorin Y, Block K (2013) Nox as a target for diabetic complications. Clin Sci 125:361–382
Teshima Y, Takahashi N, Nishio S, Saito S, Kondo H, Fukui A, Aoki K, Yufu K, Nakagawa M, Saikawa T (2014) Production of reactive oxygen species in the diabetic heart. Roles of mitochondria and NADPH oxidase. Circ J 78:300–306
Mukherjee TK, Mukhopadhyay S, Hoidal JR (2005) The role of reactive oxygen species in TNFalpha-dependent expression of the receptor for advanced glycation end products in human umbilical vein endothelial cells. Biochim Biophys Acta 1744:213–223
Harijith A, Ebenezer DL, Natarajan V (2014) Reactive oxygen species at the crossroads of inflammasome and inflammation. Front Physiol 5:352
Lieuw-A-Fa ML, van Hinsbergh VW, Teerlink T, Barto R, Twisk J, Stehouwer CD, Schalkwijk CG (2004) Increased levels of N(epsilon)-(carboxymethyl)lysine and N(epsilon)-(carboxyethyl)lysine in type 1 diabetic patients with impaired renal function: correlation with markers of endothelial dysfunction. Nephrol Dial Transplant 19:631–636
Chao PC, Huang CN, Hsu CC, Yin MC, Guo YR (2010) Association of dietary AGEs with circulating AGEs, glycated LDL, IL-1α and MCP-1 levels in type 2 diabetic patients. Eur J Nutr 49:429–434
Kaneko M, Bucciarelli L, Hwang YC, Lee L, Yan SF, Schmidt AM, Ramasamy R (2005) Aldose reductase and AGE-RAGE pathways: key players in myocardial ischemic injury. Annu N Y Acad Sci 1043:702–709
Obrosova IG, Kador PF (2011) Aldose reductase/polyol inhibitors for diabetic retinopathy. Curr Pharm Biotechnol 12:373–385
Shi L, Yu X, Yang H, Wu X (2013) Advanced glycation end products induce human corneal epithelial cells apoptosis through generation of reactive oxygen species and activation of JNK and p38 MAPK pathways. PLoS ONE 8:e66781
Fukami K, Yamagishi S, Okuda S (2014) Role of AGEs-RAGE system in cardiovascular disease. Curr Pharm Des 20:2395–2402
Kim JM, Lee EK, Kim DH, Yu BP, Chung HY (2010) Kaempferol modulates pro-inflammatory NF-kappaB activation by suppressing advanced glycation endproducts-induced NADPH oxidase. Age 32:197–208
Zang Y, Sato H, Igarashi K (2011) Anti-diabetic effects of a kaempferol glycoside-rich fraction from unripe soybean (Edamame, Glycine max L. Merrill. ‘Jindai’) leaves on KK-A(y) mice. Biosci Biotechnol Biochem 75:1677–1684
Ramar M, Manikandan B, Raman T, Priyadarsini A, Palanisamy S, Velayudam M, Munusamy A, Marimuthu PN, Vaseeharan B (2012) Protective effect of ferulic acid and resveratrol against alloxan-induced diabetes in mice. Eur J Pharmacol 690:226–235
Umadevi S, Gopi V, Elangovan V (2014) Regulatory mechanism of gallic acid against advanced glycation end products induced cardiac remodeling in experimental rats. Chem Biol Interact 208:28–36
Acknowledgments
This study was partially supported by a Grant from Ministry of Science and Technology, Taipei City, Taiwan (NSC 102-2313-B-039-002-MY3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There was no conflict of interest regarding this manuscript.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00394-017-1463-6.
Rights and permissions
About this article
Cite this article
Hsu, Cc., Yang, Ht., Ho, Jj. et al. Houttuynia cordata aqueous extract attenuated glycative and oxidative stress in heart and kidney of diabetic mice. Eur J Nutr 55, 845–854 (2016). https://doi.org/10.1007/s00394-015-0994-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0994-y