Abstract
Aims
In each cardiopulmonary exercise test (CPET), resting spirometry is performed in advance. In patients with a congenital heart defect (CHD), lung volumes are often impaired. This study investigates correlations between lung volumes and CPET parameters and determines, whether body plethysmography provides substantial additional information for these patients.
Methods
Data from 102 patients (23.8 ± 10.4 years of age, 39 female) with various forms of CHD were examined from April 2018 to October 2022. All patients underwent spirometry (measuring forced vital capacity, FVC and forced expiratory volume in 1 s, FEV1), body plethysmography (measuring total lung capacity, TLC) and an exhausting CPET. Data is presented as the median and interquartile range (z-scores) and correlated with Spearman’s rho.
Results
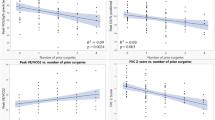
Fifty-five% of all patients had normal results in lung function and 45% had normal peak oxygen uptake (≥ 80% predicted in peak VO2). Patients with impaired lung function were significantly more likely to have low exercise capacity (Fisher’s exact test: p = 0.028). FVC z-values and %predicted peak VO2 (r = 0.365, p < 0.001) correlated significantly as well as FEV1_z and %predicted peak VO2 (r = 0.320, p = 0.001), and TLC z-values and %predicted peak VO2 (r = 0.249, p = 0.012). No correlation was found between FEV1/FVC z-values and %predicted peak VO2 (r = -0.043, p = 0.670).
Conclusion
Spirometry and exercise capacity positively correlate, also in CHD patients. However, body plethysmography does not provide additional or improved prediction and is therefore only recommended in noteworthy results in spirometry to exclude further lung co-morbidities.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays, patients with a congenital heart defect (CHD) reach not only adolescence but also adulthood [1] and, therefore, research is facing “new” questions. Survival is no longer the main goal; patients’ quality of life, exercise capacity and participation in daily life are now of high interest [2,3,4,5,6,7,8,9,10,11,12,13,14]. Additionally, co-morbidities or further notable results in patients with CHD occur more often [8].
In this prospective study, lung function and volumes were studied. Previous studies have already shown not only in COPD [15], but also in CHD, that, depending on the type of CHD, one-third to half of all patients have noteworthy results in spirometry [16, 17].
However, next to spirometry, body plethysmography (investigating total lung capacity, TLC and residual volume, RV) may explain restrictive results in spirometry and may be advisable.
This study therefore aims to (I) describe lung volumes in CHD patients, measured by spirometry and body plethysmography with the latest reference; (II) correlate these results with parameter of cardiopulmonary exercise test. Since body plethysmography is performed fewer in this cohort, the (III) whether body plethysmography even provide (better) information on CHD patients’ exercise capacity?
Materials and methods
The study was registered at the “Deutsches Register für Klinische Studien” (DRKS00021120) and approved by the ethical committee of the Technical University of Munich (project number: 110/19 S).
Study subjects
From April 2018 to October 2022 a total of 102 children and adults (23.8 ± 10.4 years of age, 39 female) with various types of CHD underwent spirometry, body plethysmography and a symptom-limited cardiopulmonary exercise test (CPET) at the German Heart Center of Munich. CPET was performed due to regular follow-up. For lung function test (body plethysmography), since it is not part of the routine, all participants signed informed consent. Table 1 shows the anthropometric data and underlying CHD classification.
Lung function and volumes
All tests were performed with the HDpft 2000 and were assessed using the software KoKo Px v7, following the latest ATS/ERS guidelines [18] in both, spirometry and body plethysmography.
Patients first underwent spirometry, and after at least two similar and valid tests were obtained, body plethysmography was performed as described in the manual. This involved having the patient breathe at the functional residual volume for at least six breaths, followed by closing a shutter to assess the volume of thoracic gas (VTG). After three breaths, the shutter automatically opens and the patient performs one normal breath before taking maximal inspiration and expiration (to assess inspiratory and expiratory capacity). Total lung capacity was calculated using the expiratory vital capacity method: average functional residual capacity (FRC) + average inspiratory capacity (IC), which is equal to residual volume (RV) + maximum ventilatory capacity (VC). At least two similar and valid tests were required.
Classification of abnormal results was done following Stanojevic et al. [18]:
-
FVC and FEV1 z-scores < -1.645 with normal FEV1/FVC defined as a preserved ratio impaired spirometry (PRISm)
-
If TLC in body plethysmography z-score < -1.645 the pattern is restrictive.
-
If TLC is normal, it is a non-specific pattern.
-
-
Normal FVC and ≥ FEV1 z-scores but FEV1/FVC z-score < -1.645 is an obstructive pattern.
-
FEV1/FVC z-score < -1.645 and a TLC z-score < -1.645 is a combination of restrictive and obstructive patterns.
-
FVC z-score OR FEV1 z-score < -1.645 but other parameters are normal as un-classified spirometry.
This last group was analyzed separately and, where needed, included in the group with markedly results (Table 2).
Exercise capacity
As part of their routine follow-up, all patients underwent a standardized [19] symptom-limited cardiopulmonary exercise test, as previously described [20, 21]: All patients performed an upright sitting bicycle CPET with a ramp-wise increase of load (5 to 30 Watts per minute). After a rest of three minutes for baseline and unloaded paddling for further three minutes, exhaustion should be reached after 8–12 min (proved by a respiratory exchange ratio ≥ 1.05 in children and ≥ 1.10 in adults). Five minutes after maximum exhaustion, patients were continuously observed. All patients were motivated to cycle to their maximum.
The highest running 30 s average of oxygen uptake was used as peak oxygen uptake (peak VO2). The percentage of predicted (%peak VO2) was calculated for children and adults below the age of 25 years by Cooper et al. [22] and adults 25 years and older, Gläser et al. [23] was used. Peak VO2 results ≥ 80% predicted are defined as normal, 80–60% as slightly impaired and < 60% as severely impaired.
All patients were under permanent 12-lead electro-cardiogram and pulse oximetry surveillance, blood pressure was measured every two minutes.
Data analyses
Due to the low number of participants, anthropometric measures were expressed as median and interquartile ranges [IQR25; IQR75]. Correlations between lung volumes and CPET were calculated using Spearman’s rho correlation or Fisher’s exact test, if adequate.
All data were analyzed using SPSS 28.0 software (IBM Inc., Armonk, NY, USA) with a two-tailed level of significance at p-value ≤ 0.05.
Results
Detailed results are seen in Table 3 and Table 4.Fifty-six patients (55%) had normal results in FVC and FEV1. While 28 patients (28%) showed a preserved ratio impaired spirometry (PRISm). Four patients had an obstructive pattern, and another four had both patterns. Of the 28 patients with PRISm, 16 (57%) were proven to have a small lung (additional TLC_z < -1.645), while the other 10 were defined as “non-specific-pattern” (normal TLC_z) and required further investigations. Table 4 shows six patients with only FEV1_z below the threshold, who can be classified as having additional obstructive results. Another four patients only had reduced FVC_z, which could be originated from insufficient effort during the test.
Overall, 45% of the patients (n = 46) had normal peak oxygen uptake (%predicted ≥ 80), 41% (n = 42) showed mild impairments with %predicted below 80 but above or equal to 60 and the others (14% or n = 14) showed severe reduction in peak oxygen uptake below 60% of peers.
Patients with impaired lung function more often showed low exercise capacity (Fisher’s exact test: p = 0.028). However, subgroups showed no significant cluster – a CHD itself does not accumulate impaired results.
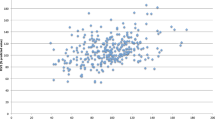
There were significant correlations between FVC_z, FEV1_z, and TLC_z with %predicted peak VO2 (r = 0.365, p < 0.001; r = 0.320, p = 0.001; r = 0.249, p = 0.012 respectively), with FVC being the strongest predictor followed by FEV1 and TLC. However, a correlation was only seen in z-score values, not in raw data (measurements in litre). Therefore, it is important to calculate the adjusted data in lung function and exercise capacity to exclude potential bias.
Discussion
In this cohort, about half of the patients with various CHD exhibit impaired results in spirometry that are associated with a limited exercise capacity.
Published data from several studies support this study’s findings: right heart obstruction patients (mostly tetralogy of Fallot) often suffer from low FVC and FEV1 [24, 25], as well as in TCPC patients, PRISm often occur [26]. However, only limited data are available for left heart obstruction or isolated shunts, showing more or less normal results in lung function tests [16, 26,27,28]. Nevertheless, patients with CHD have lower z-scores than the reference (Table 3). Furthermore, lung function correlates with exercise capacity – which was already studied in previous publications [28,29,30]. The present study adds that there is also a correlation between exercise capacity with TLC.
However, results show that a significant proportion of patients with a PRISm have significantly smaller lungs in body plethysmography (16 from 28 with a restrictive pattern). Even of more interest are those with a non-specific pattern (restrictive in spirometry with normal TLC). Formerly, these patients were classified as airflow occlusion or air trapping etc. [31, 32] which was revised with the latest task force report in 2021 [18]. In our cohort, twelve patients are grouped as “non-specific pattern”. Adding patients with only FEV1_z or FVC_z below the threshold, a total of 22 patients, representing 22% of all patients, have abnormal results that need to undergo further investigations (e.g. bronchodilator test, muscle test) [18, 30]. Co-working with lung specialists is recommended and advisable in patients with CHD.
Limitations
All included patients are under regular tertiary care. Furthermore, patients who consider their lung function test results may more likely refuse to participate. Patients with cognitive restrictions, language barriers or not being able to perform a CPET could not be included. Furthermore, if the patient did the CPET, not until full exhaustion (n = 26) were excluded. Insufficient quality in spirometry and/or body plethysmography also excluded patients (n = 76). All of these bias the results (n = 204 eligible, n = 102 for analyses).
Conclusions
Lung function and exercise capacity correlate significantly. Following the guidelines, performing a CPET in patients with CHD includes a lung function test. Not only since there is a significant correlation, but also since a valid lung function (examine FVC and FEV1) gives further information during the test (see pulmonary limitation etc.). This is why it must always be included.
However, total lung capacity and therefore body plethysmography may not add any extra or better value, except in cases where simple spirometry reveals noteworthy results. Especially if a restrictive pattern is seen, body plethysmography should be performed to ensure a restriction and warrant further examinations by a pulmonary specialist.
References
Khairy P, Ionescu-Ittu R, Mackie AS et al (2010) Changing mortality in congenital heart disease. J Am Coll Cardiol 56:1149–1157
Häcker AL, Reiner B, Oberhoffer R et al (2019) Functional outcomes in children with anatomically repaired transposition of the great arteries with regard to congenital ventricular septal defect and coronary pattern. Arch Dis Child 104:851–856
Hock J, Reiner B, Neidenbach RC et al (2018) Functional outcome in contemporary children with total cavopulmonary connection - Health-related physical fitness, exercise capacity and health-related quality of life. Int J Cardiol 255:50–54
Hock J, Schwall L, Pujol C et al (2020) Tetralogy of Fallot or Pulmonary Atresia with Ventricular Septal Defect after the Age of 40 Years: A Single Center Study. J Clin Med 9
Müller J, Christov F, Schreiber C et al (2009) Exercise capacity, quality of life, and daily activity in the long-term follow-up of patients with univentricular heart and total cavopulmonary connection. Eur Heart J 30:2915–2920
Müller J, Hess J, Hager A (2014) Sense of coherence, rather than exercise capacity, is the stronger predictor to obtain health-related quality of life in adults with congenital heart disease. Eur J Prev Cardiol 21:949–955
Muller MJ, Norozi K, Caroline J et al (2022) Morbidity and mortality in adults with congenital heart defects in the third and fourth life decade. Clin Res Cardiol 111:900–911
Neidenbach RC, Lummert E, Vigl M et al (2018) Non-cardiac comorbidities in adults with inherited and congenital heart disease: report from a single center experience of more than 800 consecutive patients. Cardiovasc Diagn Ther 8:423–431
Pelosi C, Kauling RM, Cuypers J et al (2023) Executive functioning of patients with congenital heart disease: 45 years after surgery. Clin Res Cardiol
Pujol C, Schiele S, Maurer SJ et al. (2020) Patients with Single-Ventricle Physiology over the Age of 40 Years. J Clin Med 9
Reiner B, Oberhoffer R, Ewert P et al (2019) Quality of life in young people with congenital heart disease is better than expected. Arch Dis Child 104:124–128
Tutarel O, Kempny A, Alonso-Gonzalez R et al (2014) Congenital heart disease beyond the age of 60: emergence of a new population with high resource utilization, high morbidity, and high mortality. Eur Heart J 35:725–732
Uzark K, Zak V, Shrader P et al (2016) Assessment of Quality of Life in Young Patients with Single Ventricle after the Fontan Operation. J Pediatr 170(166–172):e161
Van Den Bosch AE, Roos-Hesselink JW, Van Domburg R et al (2004) Long-term outcome and quality of life in adult patients after the Fontan operation. Am J Cardiol 93:1141–1145
Trudzinski FC, Kellerer C, Jörres RA et al (2023) Gender-specific differences in COPD symptoms and their impact for the diagnosis of cardiac comorbidities. Clin Res Cardiol 112:177–186
Alonso-Gonzalez R, Borgia F, Diller GP et al (2013) Abnormal lung function in adults with congenital heart disease: prevalence, relation to cardiac anatomy, and association with survival. Circulation 127:882–890
Hock J, Willinger L, Dalla Pozza R et al (2023) Abnormalities in pulmonary function and volumes in patients with CHD: a systematic review. Cardiol Young. 2023 Feb;33(2):169–181.
Stanojevic S, Kaminsky DA, Miller MR et al (2022) ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J 60
Mantegazza V, Apostolo A, Hager A (2017) Cardiopulmonary Exercise Testing in Adult Congenital Heart Disease. Ann Am Thorac Soc 14:S93–S101
Fritz C, Muller J, Oberhoffer R et al (2020) Inspiratory muscle training did not improve exercise capacity and lung function in adult patients with Fontan circulation: A randomized controlled trial. Int J Cardiol 305:50–55
Hock J, Remmele J, Oberhoffer R et al (2022) Breathing training improves exercise capacity in patients with tetralogy of Fallot: a randomised trial. Heart 108:111–116
Cooper DM, Weiler-Ravell D (1984) Gas exchange response to exercise in children. Am Rev Respir Dis 129:S47-48
Gläser S, Ittermann T, Schaper C et al (2013) The Study of Health in Pomerania (SHIP) reference values for cardiopulmonary exercise testing. Pneumologie 67:58–63
Akam-Venkata J, Sriram C, French M et al (2019) Does Restrictive Lung Function Affect the Exercise Capacity in Patients with Repaired Tetralogy of Fallot? Pediatr Cardiol 40:1688–1695
Powell AW, Mays WA, Knecht SK et al (2019) Pulmonary effects on exercise testing in tetralogy of Fallot patients repaired with a transannular patch. Cardiol Young 29:133–139
Fabi M, Balducci A, Cazzato S et al (2020) Resting respiratory lung volumes are “healthier” than exercise respiratory volumes in different types of palliated or corrected congenital heart disease. Pediatr Pulmonol 55:697–705
Ginde S, Bartz PJ, Hill GD et al (2013) Restrictive lung disease is an independent predictor of exercise intolerance in the adult with congenital heart disease. Congenit Heart Dis 8:246–254
Morales Mestre N, Reychler G, Goubau C et al (2019) Correlation Between Cardiopulmonary Exercise Test, Spirometry, and Congenital Heart Disease Severity in Pediatric Population. Pediatr Cardiol 40:871–877
Callegari A, Neidenbach R, Milanesi O et al (2019) A restrictive ventilatory pattern is common in patients with univentricular heart after Fontan palliation and associated with a reduced exercise capacity and quality of life. Congenit Heart Dis 14:147–155
Turquetto ALR, Caneo LF, Agostinho DR et al (2017) Impaired Pulmonary Function is an Additional Potential Mechanism for the Reduction of Functional Capacity in Clinically Stable Fontan Patients. Pediatr Cardiol 38:981–990
Hyatt RE, Cowl CT, Bjoraker JA et al (2009) Conditions associated with an abnormal nonspecific pattern of pulmonary function tests. Chest 135:419–424
Iyer VN, Schroeder DR, Parker KO et al (2011) The nonspecific pulmonary function test: longitudinal follow-up and outcomes. Chest 139:878–886
Funding
JH received an unrestricted grant from Stiftung KinderHerz Deutschland gGmbH. No other funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest.
Additional information
Parts of the data were previously presented at different congresses and were part of the PhD of Julia Hock and the MD of Mohammed Bessar.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hock, J., Bessar, M., Ewert, P. et al. Body plethysmography – additional information on exercise capacity in patients with congenital heart disease?. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02385-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02385-7