Abstract
Congenital heart disease (CHD) is a common chronic disease. This study aimed to verify the relationship between spirometry and exercise capacity in children, considering the CHD severity. All cardiopulmonary exercise testing (CPET) and Spirometry from CHD children (5–18 years) were retrospectively reviewed during three years. CPET and Spirometry were analyzed and correlated based on the CHD severity[modified Ross classification (mR)]. Patients (n = 321) were analyzed and subdivided for CHD severity (n = 49, n = 149, n = 80, n = 43, from mR1 to mR4, respectively). The maximal workload (Wmax) in mR1 and mR2 was higher than in patients from mR3 and mR4. Peak oxygen uptake (peak VO2) was reduced in mR3 and mR4 compared to mR1 and mR2. Carbon dioxide output was only significantly lower in mR4. Although spirometric parameters were globally in the normal range, forced expiratory volume and forced vital capacity were different between subgroups (p < 0.001 and p = 0.002, respectively). Wmax and peakVO2 were weakly or moderately but significantly correlated with spirometry. Respiratory exchange ratio and final blood oxygen saturation were only significantly and weakly correlated to obstruction in small airways. The most severe CHD patients had lower exercise capacity and lung function parameters. A weak to moderate correlation between CPET and spirometry was found. However, the lung function reported in our study was normal, but with a negative correlation with the age. It reinforces the benefits of precocious and regularly spirometry and CPET assessment in CHD children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD) is a frequent chronic disease among children and adolescents, with an incidence of 4 to 8 per 1000 live births [1].
In CHD pediatric and adult populations, Cardiopulmonary Exercise Test (CPET) is a routine testing in the clinical follow-up to evaluate their morbidity and mortality [2]. It is also used to detect changes in cardiovascular and respiratory adaptation during exercise and to investigate the disease severity and long-term evolution [3, 4].
In adults, cardiac (Chronic Heart Failure, CHF) and pulmonary (Chronic Obstructive Pulmonary Disease, COPD) diseases are frequently coexisting [5]. The CPET is useful to discriminate the respective impact of lung and heart defects [6] and spirometry is performed as part of the standard care [7] to assess (obstructive, restrictive, or mixed) pulmonary diseases [8].
The CHD pediatric population suffers from physical limitations associated to reduced exercise capacity [1, 9,10,11]. As previously demonstrated, CHD children who underwent sternotomy or thoracotomy are also more likely to have a pattern of restrictive lung function [12,13,14]. Consecutive chest mechanical alterations were well described and impact on lung function [15]. On the contrary, physical fitness and exercise capacity were recently correlated with enhanced lung function in adolescents and young adults [16]. Despite these evidences, potential correlations between lung function, exercise capacity, and CHD severity have never been studied.
Our study aimed to verify this potential relationship between lung function and exercise capacity in a cohort of children and adolescent with CHD, taking into account the severity of their cardiac disease.
Methods
Subjects and Study Design
All Children with CHD aged from 5 to 18 years were retrospectively selected from our database at the Cliniques universitaires Saint-Luc (UCL, Belgium) between January 2013 and December 2015. All patients performed simultaneous CPET and spirometry as part of their annual follow-up. Patients evaluated for other reasons than CHD (cardiac exploration for syncope/faint, thoracic pain, palpitations, dyspnea, etc.), and children with concomitant severe chronic disease (neurodevelopmental disorder, chronic renal or respiratory failures) were excluded from this study. Only the most recent CPET was selected for each child when they had performed more than one CPET during the period of recruitment.
The study was approved by the regional Ethics Committee at the Cliniques universitaires Saint-Luc and Université Catholique de Louvain (2016/026).
Outcomes
CPET
All children performed a maximal CPET, with a pediatric face mask (Hans Rudolph), a calibrated gas analyser (Oxycon Pro, Jaeger), a breath-to-breath measurements software (Windows 98, Jaeger), a 12-lead ECG monitoring (Cardiosoft, GE Healthcare), a pulse oxymeter (Nellcor), and an automated sphygmomanometer with adapted pediatric cuffs.
All CPET were performed on the same treadmill following a standardized modified Bruce protocol [17]: 1-min rest, 3-min warm-up (1 km/h, slope 0%), and then 2-min increments in speed (from 2.5 to 10.5 km/h) and slope (from 3 to 18%), and finally a 3-min active recovery (2.5 km/h, 0% slope) and then 2-min rest. Exercise was pursued until the limit of the child’s tolerance was reached, with active verbal encouragements. The following CPET variables were measured: oxygen uptake (VO2; ml/kg/min), carbon dioxide production (VCO2; ml/kg/min), respiratory exchange ratio (RER = VCO2/VO2), minute ventilation (VE; breaths/min), ventilatory equivalent for oxygen (VE/VO2), ventilatory equivalent for carbon dioxide (VE/VCO2), dead space-to-tidal volume ratio (VD/VT), heart rate (HR; beats per minute - bpm), maximum workload (Watts and METS), and oxygen pulse (VO2/HR; ml). For all CPET performed, the same senior qualified investigator manually established the peak oxygen uptake (peak VO2), the ventilatory anaerobic threshold (AT) using Beaver’s method [18], the ventilation efficiency (VE/VCO2 slope with VE = slope × VCO2 + b), and the oxygen uptake efficiency slope (OUES with VO2 = OUES × log10 VE + b) [19,20,21]. PeakVO2 and AT were normalized in percentage of predicted peak VO2 using normal values published by Wasserman and Cooper [22,23,24].
Spirometry
Lung function tests were performed systematically and simultaneously with a spirometric gas analyser (Oxycon Pro, Jaeger) before and after each exercise test, assessing forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), FEV1/FVC ratio [25]. Values were expressed in percentage of predicted values, as determined by European Respiratory Society (GLI 2012) [26].
Modified Ross Classification
In CHD adult population, the NYHA functional classification is the most common classification used to determine the disease severity, including heart failure. Nevertheless, this classification does not apply in pediatric patients. For this reason, we classified our pediatric CHD population into 4 severity groups using the modified Ross classification (Table 1), which was developed to assess the heart failure severity in all pediatric ages [27, 28].
Analysis
Clinical data were analyzed by SPSS Statistics 24.0 (IBM Corp., Armonk, NY, USA). Descriptive results were expressed as mean ± standard deviation (SD) and confidence interval of 95%. To verify intergroup differences based on severity (modified Ross classification), an analysis of variance (ANOVA) was used, followed by post hoc analyses (Tukey). Correlations between CPET and spirometry were evaluated using Pearson’s correlation coefficient (r). The criteria for statistical significance were set at p < 0.05 (significant), p < 0.01 (very significant), and p < 0.001 (highly significant).
Results
This retrospective study was carried out on 321 patients diagnosed with CHD. In total, we analyzed 597 CPET protocols and excluded 276 patients (they did not have a CHD). Their anthropometric and pathophysiological characteristics are shown in Table 2, divided in subgroups based on the modified Ross classification (n = 49, 149, 80, and 43, respectively). Age and body mass index (BMI) varied significantly between subgroups (p = 0.002 and p = 0.011, respectively), and as expected, all cardiovascular performance parameters were or tended to be reduced with CHD severity. Two hundred and twenty-three children previously underwent a cardiac surgery, while the 98 others were free of any surgical intervention.
It is worth observing that Wmax was higher than the predicted value in all subgroups. However, mR1 and mR2 (139.9 ± 25.3 and 128.9 ± 30.0) subgroups showed higher values than mR3 and mR4 subgroups (113.3 ± 32.6 and 95.9 ± 29.9). Moreover, these two last subgroups differed significantly from each other.
Mean peak VO2 (expressed in % of predicted value) was in the normal range for all groups except for mR4 (76.8 ± 21.5). In the mR3 and mR4 subgroups, peak VO2 (85.0 ± 20.8 and 76.8 ± 21.5) were reduced compared to the mR1 and mR2 subgroups (111.0 ± 20.3 and 104 ± 22.4). However, given the large coefficients of variation that we observed in each of the subgroups, not only the most severe patients had lower values in terms of exercise capacity parameters (% of patients with peak VO2 < 80% of predicted value in mR1 = 8%, mR2 = 11%, mR3 = 40%, and mR4 = 49%; with p = < 0.001).
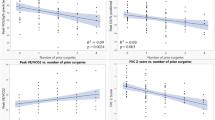
Regardless the CHD severity, even if the spirometric values were in the normal range (expressed in % of predicted value) for all subgroups, FEV1 and FVC differ significantly (p < 0.001 and p = 0.002, respectively), and 13% and 9% of children (exclusively in the surgical group) had abnormal FVC and FEV1/FVC, respectively. Negative correlations were found between age and peak VO2 (r = − 0.492; p < 0.001), FEV1 (r = − 0.397; p < 0.001) and FVC (r = − 0.289; p < 0.001). Some patients showed a reduced peak VO2 with normal FEV1 (Fig. 1).
Wmax and VO2 were correlated to all spirometric parameters, even though the intensity of all correlations was moderate to weak (Table 3). RER and final SpO2 were significantly and weakly correlated to obstruction in small airways (FEF25-75%).
Discussion
The aim of this study was to investigate the relationship between lung function and exercise capacity considering the CHD severity in pediatric population. We highlighted weak to moderate correlations between CPET and spirometry. The most severe CHD were related to lower exercise capacity performances even though all spirometric values were in the normal range. Pulmonary and cardiac disease are commonly coexisting in CHD adults [29]. However, it is not well described why and when these lung function impairments might appear in pediatric population with CHD.
There are several classifications for CHD. In clinical practice, the classification proposed by Uzark [30] or Houyel [31] is considered to be the most useful. However, the NYHA functional classification is the most commonly used in literature, especially in adults. In CHD pediatric population, the modified Ross classification [28] is preferred because it incorporates feeding difficulties, growth problems, and symptoms of exercise intolerance into a numeric score equivalent to the NYHA classification [32] used in CHD adults, and its sensitivity allows to assess and capture the progression of a heart failure [27].
In our study in pediatric CHD patients, CPET and spirometric parameters were in the normal range (Table 2) with Wmax, peak VO2, FEF 25–75%, FEV1, FVC, and FEV1/FVC within the predicted values (122.3% of predicted value, 97.1%, 102.5%, 108.5%, 105.1%, and 97.2% of predicted value, respectively). This is consistent with the study previously described by Müller [33], where the CPET parameters measured on cycloergometer were also in the normal range. Indeed, the patients from Müller had a value of mean peak VO2 of 87.1% of predicted value like in our entire cohort of CHD patients (97.1% of predicted value). However, in our cohort, the peak VO2 was significantly lower in the groups with more severe heart disease (mR1 = 111%, mR2 = 104%, mR3 = 85%, and mR4 = 76%; p = < 0.001). Müller also showed an association between the severity of the heart defect and the peak VO2 (r = − 0.410; p < 0.001) in CHD children. Note that the mean Wmax studied on treadmill in our study was also higher than the predicted value (122% of predicted value), as well as in Müller study which was performed on cycloergometer (133% of predicted value) [33].
It is well known that CHD children are less active than their healthy peers [34] and overprotection is common in children with CHD [35]. This could explain their lower CPET performance. However, physical activity and active life style are highly recommended for all CHD patients without demonstrated cardiovascular risk in CPET (ventricular dysfunction, arrhythmias...), as stated in the guidelines from the Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology [4, 36]. Furthermore, sedentary behaviors are increasingly recognized as a risk factors for cardiovascular diseases, and they increase the risk of comorbidities [34]. On this basis, we promote regular physical activity during childhood in our CHD patients, as part of a healthy general behavior [37].
Rhodes [38] showed a significant improvement in peak VO2 (p = 0.005), Wmax (p < 0.001), and FEV1 (p = 0.001) (expressed as a % of predicted value) after cardiac rehabilitation (12 week, 2 times/week during 1 h) in CHD children (6 to 17 years old) with initial peak VO2 and Wmax lower than 80% of predicted values and mR4 severity as inclusion criteria. This confirms that normal CPET and spirometry parameters reported in our cohort can be, at least in part, explained by the children’s active behavior and lifestyle.
Although we and others [38, 39] showed that the spirometry values were higher than 80% of predicted value for FVC (82.2 ± 16.0 before, 81.1 ± 14.6 after) and FEV1 (81.7 ± 16.3 before, 82.2 ± 15.8 after), they usually become abnormal with the age [29], compromising the exercise tolerance and contributing to respiratory comorbidities [15, 40]. In fact, in our cohort study, we observed a negative moderate correlation between the age of the children and the peakVO2 (r = -0.492), FEV1 (r = − 0.397), and FVC (r = − 0.289) suggesting a negative evolution related to age.
Hawkins [12] found a restrictive lung function in CHD children (n = 220) after cardiothoracic surgery by sternotomy, thoracotomy or both (25.6%, 23.5%, and 54.2% respectively; p < 0.0001). In our cohort, although 70% of children (n = 223) had a previous operation at the time of their CPET evaluation, only 13% (FVC) and 9% (FEV1/FVC) presented abnormal lung function.
Adults surviving with CHD can develop more complications compared to children. The pulmonary disease is one of the most common comorbidity in these patients [29]. In our study, we observed that CPET and spirometry presented a weak to moderate correlation, and the parameters decrease (< 80% of predicted value) with the CHD severity. However, looking at CPET and spirometry parameters and their high level of variability, it is straightforward to understand that there is a significant proportion of children with less severe CHD showing poor CPET and spirometric.
As suggested by others [7, 8], our results highlight the need for performing early lung function test in the regular follow-up of these patients, starting in childhood as a part of the prevention of future comorbidities. Indeed, we observed negative correlations between age and the different cardio-respiratory parameters.
We acknowledge some limitations in our study. A lower proportion of mR4 patients were included compared to mR1, mR2, and mR3. However, this subgroup still included 43 children (13%). The heterogeneity of lung function test reference values available in the literature (Zapletal, Cooper, Miller, GLI...) can somehow compromise inter-study and intra-study comparisons, particularly between genders.
In conclusion, while CPET parameters were normal, as expected, they were lower in the most severe CHD children. Even if the lung function reported in our large CHD pediatric population was also normal, it does not imply that these patients will not have lung impairments in adulthood as illustrated by the negative correlation with age. Moreover, we demonstrated significant correlations between Wmax and FEV1, peak VO2 and FEV1, and peak VO2 and FVC. These results suggest the potential benefits of precocious and regularly spirometry and CPET assessment in CHD children. These patients will likely benefit from an earlier and more careful evaluation to guide their postoperative rehabilitation and prevent further lung impairments in adulthood.
References
Tikkanen AU, Oyaga AR, Riaño OA, Álvaro EM, Rhodes J (2012) Paediatric cardiac rehabilitation in congenital heart disease: a systematic review. Cardiol Young 22(03):241–250
Rhodes J, Ubeda T, Jenkins KJ (2010) Exercise testing and training in children with congenital heart disease. Circulation 122(19):1957–1967
Amedro P, Picot MC, Moniotte S et al (2015) Correlation between cardio-pulmonary exercise test variables and health-related quality of life among children with congenital heart diseases. Int J Cardiol 203:1052–1060
Baumgartner H, Bonhoeffer P, De Groot NMS et al (2010) ESC Guidelines for the management of grown-up congenital heart disease. Eur Heart J 31(23):2915–2957
Barron A, Francis DP, Mayet J et al (2016) Oxygen uptake efficiency slope and breathing reserve, not anaerobic threshold, discriminate between patients with cardiovascular disease over chronic obstructive pulmonary disease. JACC Heart Fail 4(4):252–261
Myers J, Arena R, Dewey F et al (2008) A cardiopulmonary exercise testing score for predicting outcomes in patients with heart failure. Am Heart J 156(6):1177–1183
Taylor C, Nichols S, Ingle L (2015) A clinician’s guide to cardiopulmonary exercise testing 1: an introduction. Br J Hsopital Med 76(4):192–196
Longmuir PE, Brothers JA, De Ferranti SD et al (2013) Promotion of physical activity for children and adults with congenital heart disease: a scientific statement from the American Heart Association. Circulation 127(21):2147–2159
Gomes-Neto M, Saquetto MB (2015) Impact of exercise training in aerobic capacity and pulmonary function in children and adolescents after congenital heart disease surgery: a systematic review with meta-analysis. Pediatr Cardiol 37:217–224
Dulfer K, Helbing WA, Duppen N, Utens EM (2014) Associations between exercise capacity, physical activity, and psychosocial functioning in children with congenital heart disease: a systematic review. Eur J Prev Cardiol 21(10):1200–1215
Duppen N, Takken T, Hopman MTE et al (2013) Systematic review of the effects of physical exercise training programmes in children and young adults with congenital heart disease. Int J Cardiol 168(3):1779–1787
Hawkins SMM, Taylor AL, Sillau SH, Mitchell MB, Rausch CM (2014) Restrictive lung function in pediatric patients with structural congenital heart disease. J Thorac Cardiovasc Surg 148(1):207–211
Zaqout M, De Baets F, Schelstraete P et al (2010) Pulmonary function in children after surgical and percutaneous closure of atrial septal defect. Pediatr Cardiol 31(8):1171–1175
Giannico S, Hammad F, Amodeo A et al (2006) Clinical outcome of 193 extracardiac fontan patients. The first 15 years. J Am Coll Cardiol 47(10):2065–2073
Healy F, Hanna BD, Zinman R (2012) Pulmonary complications of congenital heart disease. Paediatr Respir Rev 13(1):10–15
Hancox RJ, Rasmussen F (2018) Does physical fitness enhance lung function in children and young adults? Eur Respir J 51(2):1701374
Takken T, Blank a CC, Hulzebos EHH, van Brussel M, Groen WGG, Helders PJJ (2009) Cardiopulmonary exercise testing in congenital heart disease: (contra)indications and interpretation. Neth Heart J 17(10):385–392
Beaver WL, Wasserman K, Whipp B (1986) A new method for detecting anaerobic threshold by gas exchange. Am Physiol Soc 60:2020–2027
Baba R, Nagashima M, Goto M et al (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28(6):1567–1572
Bongers BC, Hulzebos HJ,. van Brussel C, Takken M, Blank AT (2011) The oxygen uptake efficiency slope in children with congenital heart disease: construct and group validity. Eur J Cardiovasc Prev Rehabil 18(April):384–392
Giardini A, Specchia S, Gargiulo G, Sangiorgi D, Picchio FM (2009) Accuracy of oxygen uptake efficiency slope in adults with congenital heart disease. Int J Cardiol 133(1):74–79
Cooper D, Berry C, Lamarra N, Wasserman K (1985) Kinetics of oxygen uptake and heart rate at onset of exercise in children. J Appl Physiol 59(1):211–217
Cooper DM, Weiler-Ravell D, Whipp BJ, Wasserman K (1984) Growth-related changes in oxygen uptake and heart rate during progressive exercise in children. Pediatr Res 18:845
Cooper D, Weiler-Ravell D, Whipp B, Wasserman K (1984) Aerobic parameters of exercise as a function of body size during growth in children. J Appl Physiol Respir Env Exerc Physiol 56(3):628–634
Zapletal A, Motoyama EK, Van DeWoestijne KP, Hunt VR, Bouhuys A (1969) Maximum expiratory flow-volume curves and airway conductance in children and adolescents. J Appl Physiol 26:308–316
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343
Hinton RB, Ware SM (2017) Heart failure in pediatric patients with congenital heart disease. Circ Res 120(6):978–994
Ross RD, Bollinger RO, Pinsky WW (1992) Grading the severity of congestive heart failure in infants. Pediatr Cardiol 13(2):72–75
Singh AK, Patel N, Leung K, Patel P, Talwar A (2013) Manifestation of pulmonary disease in adults with CHD. Indian J Chest Dis Allied Sci 55(516):85–95
Uzark K, Jones K, Slusher J, Limbers C, Burwinkle TM, Varni JW (2008) Quality of life in children with heart disease as perceived by children and parents. Pediatrics 121(5):e1060–e1067
Houyel L, Khoshnood B, Anderson RH et al (2011) Population-based evaluation of a suggested anatomic and clinical classification of congenital heart defects based on the International Paediatric and Congenital Cardiac Code. Orphanet J Rare Dis 6(1):64
Jayaprasad N (2016) Heart failure in children. Hear Views 17(3):92–99
Muller J, Bohm B, Semsch S, Oberhoffer R, Hess J, Hager A (2013) Currently, children with congenital heart disease are not limited in their submaximal exercise performance. Eur J Cardio-Thoracic Surg 43(6):1096–1100
Voss C, Duncombe SL, Dean PH, de Souza AM, Harris KC (2017) Physical activity and sedentary behavior in children with congenital heart disease. J Am Heart Assoc 6(3):1–11
Hirth A, Reybrouck T, Bjarnason-Wehrens B, Lawrenz W, Hoffmann A (2006) Recommendations for participation in competitive and leisure sports in patients with congenital heart disease: a consensus document. Eur J Cardiovasc Prev Rehabil 13(3):293–299
Takken T, Giardini A, Reybrouck T et al (2012) Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol 19(5):1034–1065
Westhoff-bleck M, Treptau J, Löffler F (2015) Exercise training in adults with complex congenital heart disease. Ann Sport Med Res 2(6):1037
Rhodes J, Curran TJ, Camil L et al (2005) Impact of cardiac rehabilitation on the exercise function of children with serious congenital heart disease. Pediatrics 116(6):1339–1345
Turquetto ALR, Canêo LF, Agostinho DR et al (2017) Impaired pulmonary function is an additional potential mechanism for the reduction of functional capacity in clinically stable fontan patients. Pediatr Cardiol 38(5):981–990
Alonso-Gonzalez R, Borgia F, Diller GP et al (2013) Abnormal lung function in adults with congenital heart disease: prevalence, relation to cardiac anatomy, and association with survival. Circulation 127(8):882–890
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that we have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morales Mestre, N., Reychler, G., Goubau, C. et al. Correlation Between Cardiopulmonary Exercise Test, Spirometry, and Congenital Heart Disease Severity in Pediatric Population. Pediatr Cardiol 40, 871–877 (2019). https://doi.org/10.1007/s00246-019-02084-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02084-5