Abstract
Background
Little is known about the prognostic impact of heart failure (HF) duration in patients with advanced HF.
Methods
A total of 109 consecutive patients with advanced HF referred to the institutional heart transplant program between July 2014 and December 2017 were prospectively enrolled. The patients were divided into two groups according to the HF duration using a pre-specified cutoff (> 18 months, n = 38; ≤ 18 months, n = 71). The Cox proportional hazards model was generated to investigate the association between the HF duration and a 1-year composite endpoint (all-cause mortality, left ventricular assist device implantation, and hospitalization due to HF).
Results
Patients with a longer HF duration were older and had significantly lower blood pressure, and greater left ventricular volume compared with those with a shorter HF duration. The 1-year event-free survival rate was significantly lower in patients with a longer HF duration (49.1% vs. 80.0%, log-rank p < 0.001). After adjustment, a longer HF duration was independently associated with an increased risk for the composite endpoint (hazard ratio, 2.44; 95% confidence interval, 1.03–5.76; p = 0.04). Additionally, longer HF duration was independently associated with an increased wall motion score index and a decreased heart-to-mediastinum ratio of 123I-meta-iodobenzylguanidine (MIBG) myocardial scintigraphy (all associations, p < 0.05).
Conclusions
A longer HF duration is associated with an increased risk of adverse outcomes as well as more severe myocardial damage among patients with advanced HF.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a clinical syndrome with high mortality and affects 23 million people worldwide. Advanced HF is defined as a persistent or progressive severe symptomatic status with decreased cardiac function despite guideline-based optimized medical and device therapy. Recognizing the transition to this advanced stage is necessary to facilitate the triage of advanced surgical options, such as heart transplant or left ventricular assist device (LVAD) implantation, or allow physicians to initiate the management of end-of-life care.
Emerging evidence indicates that a longer duration from the initial HF diagnosis is linked to adverse outcomes [1,2,3]. A meta-analysis of 39,372 patients with HF generated a prognostic risk score, including HF duration, with the cutoff by 18 months. A post hoc study of the ASCEND-HF trial of 7141 chronic HF patients reported that a longer HF duration (i.e., > 1, > 12, or > 60 months) was associated with poor prognosis [4]. However, little is known about the prognostic impact of HF duration in patients with advanced HF considering the advanced surgical options. Additionally, a cohort study of 373 patients with LVAD support reported that a shorter HF duration prior to LVAD implantation was associated with cardiac recovery [5], suggesting an association between the HF duration and myocardial recovery capacity. To provide optimized treatment strategy for patients with advanced HF, further evidence regarding the association between HF duration and myocardial recovery capacity in this population should be accumulated.
In this study, we investigated the association between HF duration and adverse outcomes including all-cause mortality, LVAD implantation, and hospitalization due to HF and assessed the association between HF duration and myocardial recovery capacity in patients with advanced HF.
Methods
Study population
In this observational study, 109 consecutive patients with advanced HF referred to our institutional heart transplant program between July 2014 and December 2017 were prospectively enrolled. Advanced HF was defined as the advanced symptomatic status with a New York Heart Association (NYHA) functional scale ≥ 3 despite the guideline-based HF therapy or depending on the intravenous infusion of catecholamine [6, 7]. The date of the first HF admission was collected by reviewing the clinical data record. The HF duration was calculated in reference to the first HF admission. For analyses, the patients were divided into 2 groups according to the HF duration (> 18 or ≤ 18 months). The cutoff of the HF duration was chosen based on the literature [4, 8]. This study was approved by the ethics committee of Chiba University Hospital and performed in concordance with the Declaration of Helsinki. All patients provided written informed consent.
Outcome measures
The pre-specified primary outcome measure was the composite endpoint of all-cause mortality, LVAD implantation, and hospitalization due to HF. A multidisciplinary heart team including physicians and cardiac surgeons made the decision of whether or not to proceed with LVAD implantation. Echocardiography was performed after admission. In addition to the traditional measurement, we assessed the segmental myocardial contractility (grade 1 indicating normal; 2, hypokinesis; 3, akinesis; 4, dyskinesis) and calculated the wall motion score index [9, 10]. Two cardiologists blinded to the study design conducted each analysis.
Meta-iodobenzylguanidine myocardial scintigraphy
The myocardial sympathetic nerve activity was assessed in patients who underwent cardiac scintigraphy. Early and delayed anterior planar images were acquired at 15 and 210 min, respectively, after intravenously administering 111 MBq of 123I-meta-iodobenzylguanidine (MIBG) (MyoMIBG; FUJIFILM Toyama Chemical Co., Ltd., Tokyo, Japan). The heart-to-mediastinum (H/M) ratio was calculated as the ratio of the average counts per pixel in the heart to those in the mediastinum using a semiautomatic software (Smart MIBG v3.0.0.0; FUJIFILM Toyama Chemical Co., Ltd., Tokyo, Japan) [11, 12].
Statistical analysis
Baseline characteristics were compared between groups. Continuous variables were reported as the mean ± standard deviation and were analyzed using the unpaired t test, while non-normally distributed variables were analyzed using the Mann–Whitney U test. Furthermore, categorical variables were reported as frequencies and percentages and were compared using the Chi-square test or the Fisher exact test as appropriate.
To compare the 1-year event-free survival between groups, we performed the survival analysis using the Kaplan–Meier method to estimate the event probabilities at 365 days and compare the distributions of event-free survival times among the groups using the log-rank test. Then, we estimated the hazard ratio (HR) and 95% confidence interval (CI) of a HF duration > 18 months for each outcome using the Cox proportional hazards analysis. The following were used in the final multivariate model: age, male sex, body mass index (BMI), hypertension, diabetes, atrial fibrillation (AF), coronary artery disease, NYHA functional scale, systolic blood pressure, left ventricular (LV) ejection fraction, and a HF duration > 18 months [1, 8].
We also performed sensitivity analyses to examine the consistency of inference. First, we repeated the Cox hazard multivariate analysis with another cutoff of HF duration (i.e., 12 months). Second, the propensity score (PS) was calculated using a logistic regression model. After PS matching, we estimated the HR and 95% CI of a HF duration > 18 months for the adverse outcomes using the Cox proportional hazards analysis.
The associations between the HF duration and wall motion score index and H/M ratio of I123-MIBG were estimated from the logistic regression models adjusted for baseline characteristics (age, male sex, hypertension, diabetes, AF, coronary artery disease, NYHA functional scale, LV end-diastolic volume, and medication of β-blocker) [4, 10, 13].
All statistical analyses were performed using EZR version 1.37 (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). Two-tailed p values < 0.05 were considered statistically significant [14].
Results
Study population and baseline characteristics
A total of 109 consecutive patients with advanced HF were analyzed. Patients with a longer HF duration were older and more likely to show lower BMI, systolic blood pressure, and heart rate. In addition, these patients had a higher prevalence of anemia, renal dysfunction, and a greater LV volume compared with the patients with a shorter HF duration (Table 1).
Outcomes
The Kaplan–Meier analysis for the composite endpoint at 1 year is shown in Fig. 1. The event-free survival rate was significantly lower in patients with a longer HF duration (49.1% vs. 80.0%, p < 0.001) compared with those with a HF duration ≤ 18 months. The difference in the composite endpoint was mainly impacted by two factors, LVAD implantation (66.1% vs. 89.0%, p = 0.005) and hospitalization due to HF (73.0% vs. 89.8%, p = 0.06). No significant difference in all-cause mortality between groups (90.5% vs. 96.6%, p = 0.20) was noted. In the Cox proportional hazards regression analysis, a HF duration > 18 months was significantly associated with the increased risk of composite events (HR, 2.44; 95% CI 1.03–5.76; p = 0.04; Table 2). Likewise, in the sensitivity analyses using other cutoff values (HF duration > 12 months: HR, 2.55; 95% CI 1.08–6.03; p = 0.03; Supplemental Table 1) and in the PS-matched cohort (Supplemental Table 2) (HR, 2.33; 95% CI 1.05–5.15; p = 0.04), a longer HF duration was associated with an increased risk of composite events.
Event-free survival in patients with longer and shorter heart failure duration. At 1-year follow-up, patients with a heart failure duration > 18 months showed significantly lower overall event-free survival rates (49.1% vs. 80.0%, log-rank p < 0.001) compared with those with a heart failure duration ≤ 18 months
Assessment of the echocardiographic wall motion score index
Figure 2 represents the wall motion score index in each segment according to the HF duration. The mean wall motion score index was significantly larger in patients with a HF duration > 18 months compared with those with a HF duration ≤ 18 months (2.5 ± 0.3 vs. 2.2 ± 0.3, p = 0.001). In the multivariate logistic regression analysis, a HF duration > 18 months was independently associated with an increased wall motion score index (OR, 9.10; 95% CI 1.40–59.4; p = 0.02; Supplemental Table 3).
Wall motion score index in patients with longer and shorter heart failure duration. The wall motion score index was analyzed in each of the 17 wall segments in patients with longer and shorter duration of heart failure. Scores on the wall motion index are as follows: 1—normal; 2—hypokinetic; 3—akinetic; and 4—dyskinetic. Patients with a heart failure duration > 18 months showed significantly higher wall motion score index (2.5 ± 0.3 vs. 2.2 ± 0.3, p = 0.001) compared with those with a heart failure duration ≤ 18 months. *p < 0.05; **p < 0.01
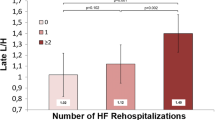
Myocardial sympathetic nerve activity
Of the 109 patients, 64 underwent 123I-MIBG myocardial scintigraphy. Patients with a HF duration > 18 months showed decreased 123I-MIBG uptake with respect to the H/M ratio (early phase, 2.0 ± 0.5 vs. 2.3 ± 0.5, p = 0.03; delayed phase, 1.6 ± 0.4 vs. 2.0 ± 0.5, p = 0.005; Fig. 3) compared with those with a HF duration ≤ 18 months. After adjustment, a HF duration > 18 months was independently and negatively associated with a delayed H/M ratio (OR, 0.08; 95% CI 0.01–0.79; p = 0.03; Supplemental Table 4).
Heart to mediastinum ratio of 123I-MIBG uptake in patients with longer and shorter heart failure duration. Sixty-nine patients underwent 123I-MIBG myocardial scintigraphy during a hospital stay. Patients with longer heart failure duration showed significantly lower H/M ratio both in the early and delayed phase compared to those with shorter heart failure duration. H/M heart-to-mediastinum, 123I-MIBG123I-meta-iodobenzylguanidine
Discussion
In this prospective cohort-based study of patients with advanced HF in a single LVAD center, we found that a HF duration > 18 months was associated with a higher risk of the composite outcomes and this association remained significant after adjustment for potential confounders. The main finding was consistent across different statistical assumptions. Additionally, we found that a HF duration > 18 months was independently associated with an increased wall motion score index as well as a decreased H/M ratio.
Importance of HF duration
The relation of HF duration with adverse outcomes is novel but consistent with earlier studies showing that patients with a shorter HF duration have favorable survival outcomes compared with those with a longer HF duration [1, 4, 15]. For example, a post hoc analysis of a randomized controlled study of 7141 hospitalized patients with acute HF reported that a HF duration < 1 month was independently associated with better survival [1]. More recently, a post hoc analysis of the SHIFT trial of 6505 patients with stable HF and reduced LV ejection fraction (< 35%) reported the parallel association between HF duration and adverse outcomes [4]. However, the prediction of adverse outcomes is more critical in patients with advanced HF and still desirable to make a strategical approach (i.e., LVAD implantation, heart transplant, end-of-life care). Our main observation is consistent with these earlier findings, and we extend them by demonstrating the association between a longer HF duration and increased risk of adverse outcomes in patients with advanced HF.
Myocardial capacity to recover
The reasons for the association between a longer HF duration and worse clinical prognosis remain to be elucidated. Several plausible underlying mechanisms linking HF duration to adverse outcomes are noted. Patients with a longer HF duration were older and more likely to have multiple comorbidities (e.g., AF, renal dysfunction) [1, 8] or HF-related physiological changes (e.g., higher age, sarcopenia) [16,17,18], which may contribute to the worsened clinical prognosis. Although these comorbidities play a role, the association between HF duration and adverse outcomes persisted significantly after adjusting these comorbidities in the earlier studies [1, 4] and in the present report.
Another possible explanation for the association may be linked to myocardial remodeling. Since HF is accompanied by myocardial remodeling as well as comorbidities, it is likely that patients with a longer HF duration have a progressive cardiac remodeling through long-standing neuroendocrine activation followed by calcium handling defects or beta-adrenergic signal transduction [19, 20]. In the present study, we found that a longer HF duration was independently associated with an increased wall motion score index, suggesting more advanced myocardial damage. These findings are in line with previous studies investigating patients with advanced HF [3, 21, 22]. For example, a cohort study of 373 patients treated with LVAD reported that a longer HF duration was associated with the smaller improvement of LV function during LVAD treatment [5]. Additionally, in the sub-cohort of 123I-MIBG myocardial scintigraphy in the present study, we found that patients with a longer HF duration were independently associated with a decreased delay H/M ratio, suggesting the poor myocardial capacity to recover in response to medical or advanced device therapy [13, 23]. In conclusion, consistent with earlier studies, our findings (a longer HF duration is associated with an increased wall motion score index and decreased H/M ratio) suggest that a longer HF duration is linked to irreversible myocardial damage, resulting in poor prognosis.
Limitations
The present study has several limitations. First, the present study was based on a prospective cohort study in a single LVAD center with a relatively small number of patients. Therefore, the number of covariates in the multivariate models is limited. However, our main findings are consistent across different statistical assumptions, including PS matching, adjusting for baseline characteristics and echocardiography findings. Second, while our finding (the association between longer HF duration and increased wall motion score index) suggests more advanced myocardial damage in patients with a longer HF duration, we did not assess follow-up echocardiography findings. Nevertheless, the adjunctive findings of 123I-MIBG suggest the poor myocardial capacity to recover by demonstrating the association between a longer HF duration and H/M ratio. Third, since our data was based on patients with advanced HF referred to institutional heart transplant program, caution should be used in generalizing the current results. Nevertheless, our findings will serve as an important foundation for further investigation to establish strategic approaches in patients with HF and determine the mechanisms of association between HF duration and clinical prognosis.
Conclusions
In patients with advanced HF, a longer HF duration is associated with an increased risk of adverse events compared with a shorter HF duration. Additionally, a longer HF duration is independently associated with impaired myocardial motion and decreased sympathetic nerve activity, suggesting lower myocardial recovery capacity.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRT:
-
Cardiac resynchronization therapy
- HF:
-
Heart failure
- H/M:
-
Heart-to-mediastinum
- HR:
-
Hazard ratio
- ICD:
-
Implantable cardioverter defibrillation
- 123I-MIBG:
-
123I-meta-iodobenzylguanidine
- LVAD:
-
Left ventricular assist device
- LV:
-
Left ventricular
- NYHA:
-
New York Heart Association
- OR:
-
Odds ratio
References
Greene SJ, Hernandez AF, Dunning A, Ambrosy AP, Armstrong PW, Butler J et al (2017) Hospitalization for recently diagnosed versus worsening chronic heart failure: from the ASCEND-HF Trial. J Am Coll Cardiol 69(25):3029–3039. https://doi.org/10.1016/j.jacc.2017.04.043(Epub 2017/06/24, PubMed PMID: 28641792)
Lassus JP, Siirila-Waris K, Nieminen MS, Tolonen J, Tarvasmaki T, Peuhkurinen K et al (2013) Long-term survival after hospitalization for acute heart failure–differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol 168(1):458–462. https://doi.org/10.1016/j.ijcard.2012.09.128(Epub 2012/10/18, PubMed PMID: 23073273)
Loyaga-Rendon RY, Acharya D, Pamboukian SV, Tallaj JA, Cantor R, Starling RC et al (2015) Duration of heart failure is an important predictor of outcomes after mechanical circulatory support. Circ Heart Fail 8(5):953–959. https://doi.org/10.1161/circheartfailure.115.002321(Epub 2015/08/08, PubMed PMID: 26251182)
Bohm M, Komajda M, Borer JS, Ford I, Maack C, Tavazzi L et al (2018) Duration of chronic heart failure affects outcomes with preserved effects of heart rate reduction with ivabradine: findings from SHIFT. Eur J Heart Fail 20(2):373–381. https://doi.org/10.1002/ejhf.1021(Epub 2017/10/14, PubMed PMID: 29027329)
Boehmer JP, Starling RC, Cooper LT, Torre-Amione G, Wittstein I, Dec GW et al (2012) Left ventricular assist device support and myocardial recovery in recent onset cardiomyopathy. J Card Fail 18(10):755–761. https://doi.org/10.1016/j.cardfail.2012.08.001(Epub 2012/10/09, PubMed PMID: 23040110)
Chaudhry SP, Stewart GC (2016) Advanced heart failure: prevalence, natural history, and prognosis. Heart Fail Clin 12(3):323–333. https://doi.org/10.1016/j.hfc.2016.03.001(Epub 2016/07/03, PubMed PMID: 27371510)
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128(Epub 2016/05/22, PubMed PMID: 27206819)
Pocock SJ, Ariti CA, McMurray JJ, Maggioni A, Kober L, Squire IB et al (2013) Predicting survival in heart failure: a risk score based on 39,372 patients from 30 studies. Eur Heart J 34(19):1404–1413. https://doi.org/10.1093/eurheartj/ehs337(Epub 2012/10/26, PubMed PMID: 23095984)
Doughty RN, Whalley GA, Walsh HA, Gamble GD, Lopez-Sendon J, Sharpe N (2004) Effects of carvedilol on left ventricular remodeling after acute myocardial infarction: the CAPRICORN Echo Substudy. Circulation 109(2):201–206. https://doi.org/10.1161/01.cir.0000108928.25690.94(Epub 2004/01/07, PubMed PMID: 14707020)
Nath S, DeLacey WA, Haines DE, Berry VA, Barber MJ, Kron IL et al (1993) Use of a regional wall motion score to enhance risk stratification of patients receiving an implantable cardioverter-defibrillator. J Am Coll Cardiol 22(4):1093–1099 Epub 1993/10/01 PubMed PMID: 8409046
Okuda K, Nakajima K, Hosoya T, Ishikawa T, Konishi T, Matsubara K et al (2011) Semi-automated algorithm for calculating heart-to-mediastinum ratio in cardiac Iodine-123 MIBG imaging. J Nucl Cardiol 18(1):82–89. https://doi.org/10.1007/s12350-010-9313-4(Epub 2010/11/26, PubMed PMID: 21104360)
Grayburn PA, Sannino A, Packer M (2019) Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT Trials. JACC Cardiovasc Imaging 12(2):353–362. https://doi.org/10.1016/j.jcmg.2018.11.006(Epub 2018/12/17, PubMed PMID: 30553663)
Imamura T, Kinugawa K, Nitta D, Kinoshita O, Nawata K, Ono M (2016) Preoperative iodine-123 meta-iodobenzylguanidine imaging is a novel predictor of left ventricular reverse remodeling during treatment with a left ventricular assist device. J Artif Org 19(1):29–36. https://doi.org/10.1007/s10047-015-0857-6(Epub 2015/07/30, PubMed PMID: 26219410)
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl 48(3):452–458. https://doi.org/10.1038/bmt.2012.244(Epub 2012/12/05, PubMed PMID: 23208313; PubMed Central PMCID: PMCPMC3590441)
Lassus JP, Siirila-Waris K, Nieminen MS, Tolonen J, Tarvasmaki T, Peuhkurinen K et al (2013) Long-term survival after hospitalization for acute heart failure–differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol 168(1):458–462. https://doi.org/10.1016/j.ijcard.2012.09.128(Epub 2012/10/18, PubMed PMID: 23073273)
Akita K, Kohno T, Kohsaka S, Shiraishi Y, Nagatomo Y, Izumi Y et al (2017) Current use of guideline-based medical therapy in elderly patients admitted with acute heart failure with reduced ejection fraction and its impact on event-free survival. Int J Cardiol 235:162–168. https://doi.org/10.1016/j.ijcard.2017.02.070(Epub 2017/03/06, PubMed PMID: 28259550)
Bekfani T, Pellicori P, Morris DA, Ebner N, Valentova M, Steinbeck L et al (2016) Sarcopenia in patients with heart failure with preserved ejection fraction: impact on muscle strength, exercise capacity and quality of life. Int J Cardiol 222:41–46. https://doi.org/10.1016/j.ijcard.2016.07.135(Epub 2016/07/28, PubMed PMID: 27454614)
Tsuchida K, Fujihara Y, Hiroki J, Hakamata T, Sakai R, Nishida K et al (2018) Significance of Sarcopenia evaluation in acute decompensated heart failure. Int Heart J 59(1):143–148. https://doi.org/10.1536/ihj.17-057(Epub 2018/01/16, PubMed PMID: 29332917)
Bohm M, Gierschik P, Jakobs KH, Pieske B, Schnabel P, Ungerer M et al (1990) Increase of Gi alpha in human hearts with dilated but not ischemic cardiomyopathy. Circulation 82(4):1249–1265 Epub 1990/10/01, PubMed PMID: 2169357
Hasenfuss G, Reinecke H, Studer R, Meyer M, Pieske B, Holtz J et al (1994) Relation between myocardial function and expression of sarcoplasmic reticulum Ca(2+)-ATPase in failing and nonfailing human myocardium. Circ Res 75(3):434–442 Epub 1994/09/01, PubMed PMID: 8062417
Hu B, Zhou Q, Chen J, Tan T, Yao X, Song H et al (2017) Prediction for improvement and remodeling in first-onset myocardial infarction by speckle tracking echocardiography: is global or regional selection better? Ultrasound Med Biol 43(10):2452–2460. https://doi.org/10.1016/j.ultrasmedbio.2017.06.001(Epub 2017/07/05, PubMed PMID: 28673476)
Imamura T, Kinugawa K, Nitta D, Komuro I (2016) Shorter heart failure duration is a predictor of left ventricular reverse remodeling during adaptive servo-ventilator treatment in patients with advanced heart failure. Int heart j 57(2):198–203. https://doi.org/10.1536/ihj.15-332(Epub 2016/03/15, PubMed PMID: 26973264)
Yamazaki J, Muto H, Kabano T, Yamashina S, Nanjo S, Inoue A (2001) Evaluation of beta-blocker therapy in patients with dilated cardiomyopathy—clinical meaning of iodine 123-metaiodobenzylguanidine myocardial single-photon emission computed tomography. Am Heart J 141(4):645–652. https://doi.org/10.1067/mhj.2001.112783(Epub 2001/03/29, PubMed PMID: 11275933)
Acknowledgements
Goto Tadahiro MD MPH (Graduate School of Medical Sciences, University of Fukui, Fukui, Japan) and Tabata Noriaki MD PhD (Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Bonn, Germany) were consulted for statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sugiura A, Kitahara H, Iwahana T, Eguchi N, Okada S, Miyauchi H and Kobayashi Y report no relationships that could be construed as a conflict of interest. Werner N reports having received speaker honoraria and research grants from Medtronic, Boston scientific, Abbott, and Edwards Lifesciences.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sugiura, A., Kitahara, H., Iwahana, T. et al. Association of heart failure duration with clinical prognosis in advanced heart failure. Clin Res Cardiol 109, 350–357 (2020). https://doi.org/10.1007/s00392-019-01515-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01515-w