Abstract
Background
Estimating the quantitative effect of transcatheter mitral valve repair on functional parameters and quality of life is important for individual treatment decision-making.
Methods
We combined data from a prospective monocentric cohort study (N = 215) with data from a systematic literature review (PubMed search term “mitraclip”, till 30.04.2016) on patients undergoing MitraClip with at least mortality after discharge reported as an outcome. Effects on functional parameters were reported as range of mean change.
Results
36 observational studies and 1 randomized controlled trial were identified. Due to substantial heterogeneity of effect estimates (I 2-heterogeneity >75%) and inadequate quality of studies with a lack of comparison group in 97.4% and lack of an independent assessment of outcomes in 86.8%, no pooled estimates were calculated. All studies reported improvements of mean New York Heart Association (NYHA) class (0.5–1.9 classes), Short-Form (SF)-12/36 scores (4.4–9.2 for physical component score, 2.6–8.9 for mental component score), 6-min walk distance [(6MWD) 2–336 m] and Minnesota Living with Heart failure questionnaire (MLWHFQ) score (−7 to −18 points), with improvements regarded as clinically relevant in 20 of 29 studies for NYHA class, in all of 7 studies for SF12/36, in 9 of 15 studies for 6MWD and in all of 8 studies for MLWHFQ.
Conclusion
MitraClip therapy provides improvements in physical capacity, physical and mental functioning and disease-specific quality of life in the majority of patients. However, more comparative and high-quality studies are required for understanding the heterogeneity of results, which is crucial for optimal patient selection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mitral regurgitation (MR) affects almost 10% of people over 75 years of age [1]. With aging populations, the potential impact of symptomatic severe MR on functional status, quality of life and health care expenditure is considerable [2, 3].
Due to high surgical risk about half of patients with symptomatic severe MR do not undergo valve surgery which is the therapy of first choice [4]. Percutaneous mitral valve repair (PMVR) has emerged as an alternative option for many inoperable or high-risk patients with symptomatic MR [5, 6]. The MitraClip system is currently the most widely applied method with more than 40,000 implants worldwide. So far a benefit of PMVR compared to conservative or surgical treatment regarding mortality has not been shown and hence PMVR is recommended as a symptomatic therapy [7]. In the EVEREST II study, which is the only randomized study on PMVR so far, an improvement in quality of life was demonstrated in patients undergoing MitraClip procedure, which was similar in magnitude when compared to surgical repair [8]. However, these data cannot be transferred to real-world patients undergoing PMVR who substantially differ with respect to underlying mitral valve pathology, age, left-ventricular function and comorbidity [9,10,11,12,13]. Taken together, the actual impact of PMVR regarding quality of life, symptom burden and functionality is weakly quantified, but of major interest for physicians and patients to guide informed-decisions [14, 15] and estimate the benefit of PMVR within the health care system.
The aim of this study was to systematically evaluate and quantify the impact of PMVR using MitraClip on various measures of functionality. We used data of a prospective cohort of patients undergoing MitraClip procedure at our center with assessment of 6-min walking distance, heart failure associated symptoms and health-related quality of life, and combined results with data obtained from a systematic review on this topic.
Methods
Prospective cohort study
All patients undergoing MitraClip procedure at our high-volume referral center were eligible for inclusion if written informed consent was given by the patient, starting in May 2014 to June 2016. All patients were on optimal medical therapy, had indication for treatment of MR according to current guidelines and underwent discussion in the interdisciplinary Heart Team with the concordant decision on an interventional treatment with the MitraClip system. There were no general clinical or morphologic criteria precluding PMVR, but the decision on feasibility basically aligned with criteria defined in a recent consensus paper of the German Society of Cardiology [16]. The study was approved by the local ethics committee of the University of Cologne (14-116).
Six-minute walking distance (6MWD) [17], New York Heart Association (NYHA)-class, Minnesota Living with Heart Failure Questionnaire (MLWHFQ) [18] and the generic, validated Medical Outcomes Study Short-Form 36 [19, 20] (SF-36, Optuminsight, Life Sciences, Inc.), were assessed during the hospitalization 1–5 days before the procedure, depending on time between admission and procedure, and at follow-up about 6 weeks after the procedure by a trained medical student who was blinded to procedural and echocardiographic results.
Systematic review protocol: data sources and study selection
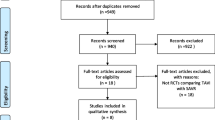
According to PRISMA criteria for systematic reviews [21], we conducted a systematic search of PubMed using the word “mitraclip” until 30.04.2016, without language restriction, to identify full-length papers on prospective and retrospective studies that reported functional status or quality of life outcome after MitraClip. We also manually searched included references of seven published reviews [22,23,24,25,26,27,28] (Fig. 1).
Studies were eligible if they reported one of the following functional measures at baseline and beyond discharge following MitraClip: (1) all-cause mortality; (2) NYHA functional class; (3) the SF-12/-36 physical component summary (PCS) and mental component summary (MCS); and (4) other measures of functional capacity and quality of life, including 6MWD, EuroQol-5D [29], and the MLWHFQ. Studies were excluded if: (1) they were experimental studies on animals, reviews, commentaries, case reports, or abstracts; (2) the intervention was not MitraClip; and (3) the study lacked defined outcomes for inclusion. When more than one study originated from the same patient population, studies were prioritized according to the following hierarchy of characteristics: (1) all quantitative measures of functionality and quality of life superior to NYHA class; (2) sample size; and (3) duration of follow-up. One multicenter registry [30] was included for the analysis, albeit parts of the registry population were also reported in several other studies [31,32,33,34,35,36] included in the systematic review. However, only the outcome EuroQol-5D was analyzed from the registry population, which was not reported and analyzed in the individual studies.
Two investigators (C.I. and R.P.) independently assessed abstracts and full-text papers for eligibility, and disagreement was resolved in all cases after a second independent re-assessment by the two investigators.
Data extraction and quality assessment
Two investigators (C.I. and S.L.) independently examined the quality of the assessed studies and disagreement was resolved by a third reviewer (R.P.). We modified the Newcastle-Ottawa Scale [37] to evaluate studies for the following quality domains (see Appendix Method 1): (1) representativeness of source population; (2) selection of the comparison patients; (3) assessment of functional outcomes; and (4) adequacy of follow-up. Evidence for publication bias was assessed visually using Funnel plots and was tested statistically using the Egger’s regression test of asymmetry.
A standardized form was used to extract patient-related and treatment-related characteristics. The following primary outcomes were extracted (for details of these measures see Appendix Tab. 1): change in NYHA class (≥1 class) [38], SF-12/36 PCS and MCS scores (≥2.5 points) [39], 6MWD (≥50 m) [17], EuroQol-5D (≥0.074 points) [40], and MLWHFQ (≥5 points) [41]. Cut-off values which are usually regarded as clinically meaningful for patients are shown in brackets. These cut-off values are arbitrary and not explicitly validated in PMVR patients, but are recommended in recent consensus statements on clinical trial design of transcatheter mitral valve repair and heart failure [42,43,44]. We also extracted all-cause mortality as secondary outcome. Where matched data were available, we used only the matched data for the clinical parameters [31, 45]. Where the median and interquartile range was given, we assumed the distribution was normal or approximately normal. Thus, we converted mean = median and standard deviation = IQR/1.35 [46].
Data synthesis and analysis
As a result of poor quality of included studies and considerable unexplained heterogeneity, we summarized the change in primary outcomes descriptively. Missing data on mean change and corresponding standard deviation were obtained as described in Chapter Seven of the Cochrane Handbook for Systematic Reviews of Interventions [46] (see Appendix Method 2 for computation of the change in primary outcomes), without pooling individual study estimates. If there were very few high-quality studies, a DerSimonian–Laird random-effects estimate [47] can be misleading and its 95% confidence interval underestimates the uncertainty of treatment effects. Thus, we presented the range (minimum–maximum) of observed mean changes and displayed the variation in forest plots. Since baseline values of 6MWD differed substantially across studies, we calculated percent changes from baseline to follow-up for secondary analyses (see Appendix Method 3 [48]). Because of the high heterogeneity of effect estimates we performed meta-regression including important study baseline characteristics and study quality criteria (representativeness of patients, availability of comparison group, completeness of follow-up and outcome assessment) using the STATA command “metareg” for outcomes with 10 or more study groups available. Analyses were performed in STATA version 12.1 (StataCorp LP, USA).
Results
Prospective cohort study
Of 230 patients admitted for MitraClip procedure, 217 agreed for participation, 2 of whom died before the procedure (Appendix Fig. 1). 215 patients were included [mean age 78 (±8) years; 57% male] in the study with a high estimated surgical risk [mean Logistic EuroScore 22% (±16%)]. Frequency of categories of left-ventricular ejection fraction (<30, 30–50 and >50%) was 27, 27 and 46%, respectively. Underlying pathology of MR was primary/degenerative in 35%, secondary/functional in 57%, or combined degenerative and functional in 8%. 87% of patients were in NYHA class III/IV.
In 7 of 215 patients (3%) a Clip could not be implanted because of technical, procedural or morphologic reasons. Overall, 192 (89%) patients underwent successful MitraClip implantation which was defined by implantation of at least 1 clip and reduction of MR grade to ≤2. No patient was lost to follow-up at 6 weeks regarding vital status. Of 208 patients with at least 1 Clip implanted, 6 (2.9%) patients died postprocedural or during 6-week follow-up. Paired values for baseline and follow-up in patients with at least 1 clip implanted and surviving till follow-up were available in 196 (97%) patients for NYHA class, in 142 (70%) patients for 6MWD and in 171 (85%) patients for MLWHFQ, PCS and MCS. Missing values were mainly due to incomplete assessment of distinct tests during follow-up visit.
Mean NYHA class decreased from 2.9 (SD 0.5) to 2.4 (SD 0.6, p < 0.0001), with 55% of patients showing an improvement of 1 class or more. Mean 6MWD increased from 256 m (SD 129 m) to 299 m (SD 121 m, p < 0.0001), with 39% of patients showing an improvement of 50 m or more. Mean MLWHFQ score decreased from 34 points (SD 18) to 21 points (SD 15, p < 0.0001), with 70% of patients showing an improvement of 5 points or more. Finally, mean PCS and MCS increased from 36 points (SD 8) and 49 points (SD 11) to 42 points (SD 8, p < 0.0001) and 52 points (SD 9, p = 0.0006), with 70 and 53% of patients showing an increase of 2.5 points or more.
Patient characteristics in included studies
Our systematic review identified 36 observational studies (34 studies of pre- and post-PMVR comparison [30,31,32,33,34,35, 45, 49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], one study of PMVR versus conservative treatment [76] and one study of PMVR versus healthy controls [36]) and 1 randomized controlled trial of PMVR compared to surgical treatment (EVEREST II trial, [8]). Clinical characteristics of patients treated with PMVR varied widely across studies (Table 1; see Appendix Tab. 2 for characteristics of individual studies). In two observational studies with comparison groups, PMVR patients were well matched regarding age, gender, logistic EuroScore, ejection fraction and cause of mitral regurgitation compared to conservatively treated patients. Many observational studies included patients who were older, had lower ejection fraction, had functional mitral regurgitation and had higher procedural success than patients in the EVEREST II trial.
Quality of included studies
The majority were small pre- and post- PMVR comparison observational studies that are prone to a high-risk of biases (see Appendix Tab. 3 for quality assessment of individual studies and Appendix Fig. 2 for summary of quality assessment). The small number of head-to-head comparison studies (2 of 38 studies) poses major challenges in drawing definitive conclusions about the functional benefits of PMVR from the available evidence. In addition, the lack of independent assessors of functional outcomes [33 studies (87%)], especially when a subjective interpretation of patient responses is possible, may lead to a conclusion favoring PMVR. Representativeness of included patients was limited or unclear in 23 (61%) studies. The pre- and post-PMVR comparison among survivors and the presence of non-negligible loss to follow-up [defined by more than 10% loss to follow-up without report of reasons; 23 studies (61%)] may also overestimate the benefits of PMVR.
There was evidence for significant publication bias for the outcomes NYHA class (p < 0.0001), PCS of SF-12/-36 (p = 0.02) and MLWHFQ (p = 0.006, Appendix Fig. 3).
Change in NYHA class
Changes in NYHA class were reported in 34 studies. Five studies [8, 31, 54, 59, 68] only qualitatively reported changes in NYHA class after PMVR with an improvement reported in all five studies. In 29 studies with quantitative data, a substantial variation in the mean change in NYHA class was observed (I 2 = 88.6%, p < 0.001 Fig. 2). In most studies, there was an average improvement of ≥1 NYHA classes after PMVR. However, several studies ([34, 35, 51, 52, 55, 56, 62, 69, 72, 74], our cohort) showed a mean change <1 NYHA class.
SF-12/-36 physical and mental component summary scores
Changes in SF-12/-36 summary scores were reported in seven studies. The mean PCS and MCS score improved in all studies with a difference regarded as clinically meaningful, with significant heterogeneity across studies (PCS range 4.4–9.2 points, I 2 = 75.1%, p < 0.001; MCS range 2.6–8.9 points, I 2 = 82.4%, p < 0.001, Fig. 3a, b). The change in SF-12/36 scores for surgical mitral valve repair (SMVR) and conservative treatment was only assessed in one study each. Patients who underwent SMVR had improvement in PCS score of 4.4 points and in MCS of 3.8 points. Healthy controls had no change in their PCS and MCS scores.
Six-minute walk distance
Changes in 6MWD were reported in 15 studies with marked heterogeneity (I 2 = 95.3%, p < 0.001) and a range of mean change from 2 to 336 m (Fig. 4). All studies showed an improvement and the majority showed an improvement of more than 50 m increase. Analyzing 6MWD as “percent change from baseline” did virtually not change results (I 2 = 81.8%, p < 0.0001, Appendix Fig. 4).
MLWHF, other measures and mortality
Changes in MLWHFQ score were reported in eight studies with substantial heterogeneity (I 2 = 89.4%, p < 0.001) regarding the magnitude of improvement ranging from −7 to −18 points (Fig. 5). All studies showed an improvement with the lower limit of the 95% interval less than −5 points.
Change in the Minnesota Living With Heart Failure Questionnaire Score. Some studies reported estimates by subgroups only and in this case 2 lines are presented for one study without repeating the author (year). MLWHFQ Minnesota Living With Heart Failure Questionnaire, CI confidence interval, SD standard deviation
One registry study reported changes in EQ-5D quality of life with an increase in mean EQ-5D score from 0.8 to 0.9 which is regarded as clinically meaningful [40].
Mortality was reported in 37 studies, with a range from 0 to 20% (mean 7%) within up to 6 months, a range from 6 to 31% (mean 18%) for >6 to 12 months and a range from 5 to 46% (mean 24%) for more than 12 months.
Meta-regression analysis
Meta-regression analyses were performed for the outcomes NYHA class and 6MWD. Only baseline NYHA class, age and sample size were significantly associated with variation of NYHA class changes after PMVR across studies. Heterogeneity I 2 decreased from 88.6 to 83.8% when adjusting for the effects of baseline NYHA class, age and sample size, suggesting a statistically significant association, but no relevant association that can explain heterogeneity. For 6MWD only baseline 6MWD was significantly associated with the variation of 6MWD changes after PMVR, with a decrease of heterogeneity I 2 from 95.3 to 93.8% when adjusting for baseline 6MWD.
Discussion
This systematic review shows distinct variations across 38 studies in the clinical characteristics of patients undergoing MitraClip as well as in the amount of improvement in functional outcomes. There was a consistent trend that MitraClip ameliorated functional capacity, physical and mental functioning as well as disease-specific quality of life. However, this evidence is based on studies of low to moderate quality with small patient numbers. These findings might nevertheless be of relevance for patients with severe symptomatic mitral regurgitation with prohibitive or high surgical risk amenable to MitraClip therapy, since this procedure so far lacks data on a morbidity and mortality benefit.
A body of evidence demonstrates that MitraClip is an effective and safe treatment option for severe MR in high-risk or inoperable patients [11, 16, 30, 34, 45, 64, 77]. Technical efficacy and safety are essential to judge the feasibility of MitraClip and eligibility of certain patient subgroups as well as to gain a safety approval. However, they do not reflect the subjective benefits from the patients’ perspective such as functionality and quality of life, which are crucial to weight up disease- and treatment-related burden [78]. Although earlier studies reported health-related quality of life after surgical and interventional mitral valve treatment [79], no current study systematically reviewed quantitative effect estimates on functional parameters after PMVR.
In our prospective cohort study we assessed a broad spectrum of validated, functional measures including exercise performance, general and disease-specific quality of life in addition to NYHA class, as recommended by the Mitral Valve Academic Research Consortium [80, 81], and overall was the second largest, non-registry study providing any quantitative functional measure. This is of particular relevance given that altogether only 7–15 of the 38 studies identified in this review reported quantitative measures of functionality. Hence, our sample of 142–171 patients with respective measures available provides a substantial part of the total number of patients of all studies combined, ranging from about 700–1000. A limitation of our study is the lack of a comparison group, which, however, applies to all studies in this field. To the best of our knowledge no study exists so far which provides an appropriate comparison group to objectively quantify the benefit of MitraClip therapy in comparison to the natural course of the disease or a gold-standard alternative therapy. The EVEREST II randomized trial included patients substantially differing from patients currently treated with MitraClip in real life. Other studies compared to healthy controls or did not provide quantitative functional measures. A further limitation of our cohort study is the short follow-up of 6 weeks. Notably, we did not observe an association of follow-up duration with the effects of MitraClip in meta-regression analysis, suggesting that recovery from the procedure is fast and patients show early and sustained benefits.
Our systematic review revealed that data on quantitative measures of functionality in patients undergoing MitraClip are sparse. The most frequently reported measure in 34 of 38 studies was NYHA class. However, the relation with objective measures of exercise capacity in elderly and morbid patients is poor [82] and challenge the suitability of NYHA class to capture impact on functional capacity and quality of life in patients undergoing MitraClip treatment [83]. The majority of the 7–15 studies reporting more sophisticated functional measures showed an overall improvement regarded as clinically meaningful. For example, the mean absolute benefit regarding 6MWD was larger than observed in heart failure patients undergoing cardiac resynchronization therapy (CRT) in all but one study, whereas the improvement in MLWHFQ was slightly lower in MitraClip studies compared to CRT, but can be still regarded as clinically relevant [84].
However, these findings have to be interpreted cautiously. As already discussed, the small sample sizes and lack of appropriate comparison groups limits an accurate effect estimation of MitraClip, and the observed publication bias might cause overestimation of effects. A further major drawback is the substantial heterogeneity across studies regarding patient characteristics, procedural success and primary outcomes. Meta-regression analyses did not identify variables which could explain heterogeneity of effects. Notably, functional or degenerative MR pathology was not associated with variation in changes of NYHA class or MLWHF. Important to note, the small number of studies with quantitative measures limits the statistical power of meta-regression analysis and hence, variable baseline characteristics as well as study quality criteria might have individual and cumulative impact on the heterogeneity of treatment effects. The large unexplained heterogeneity precludes accurate estimation of generally applicable effect sizes of benefit, which would be important for sample size calculations in future treatment trials. Additionally, the heterogeneity of beneficial effect sizes highlights the need for better tools to identify patients with best clinical response to this therapy and hence best risk–benefit for the patient as well as cost-effectiveness ratio for the health system.
An important step to improve evaluation of quality of life and functional parameters in patients undergoing MitraClip procedure will be the standardization of trial design, as recommended by MVARC [43, 44, 80, 81]. Crucial aspects are concomitant assessment of validated quality of life scales and exercise tests, as was done in our cohort, to confirm consistency, and longitudinally repeated assessments at predefined follow-up intervals with detailed report of frequency of lost patients and causes. However, it has to be emphasized that the MVARC recommendations are expert consensus and for example, cut-off values of functional parameters defined as clinically meaningful have not been validated in MitraClip patients. Particularly in the context of subjective endpoints such as quality of life, selection of an appropriate comparator group and blinded outcome assessors are mandatory. Several ongoing multicenter, randomized trials (COAPT, RESHAPE-HF2, MITRA-FR, MATTERHORN) evaluating MitraClip therapy in functional MR will analyze functional and quality of life outcomes and hopefully shed light on the quantification and individualization of MitraClip benefits.
There are additional limitations worth mentioning. Although we tried to exclude duplicate inclusion of patients mentioned in different studies, due to several multicenter studies and limited methodological reporting some patients might be included more than once. Finally, we included outcome reportings of only one follow-up time point per study for clarity reason favoring the longest follow-up presented. Due to this compromise data on more patients might be available in few studies, but with a shorter follow-up time.
Conclusion
To synopsize, treatment of severe MR with MitraClip results in improvements of physical capacity, physical and mental functioning as well as disease-specific quality of life usually regarded as clinically meaningful in the majority of patients. However, considering the huge between-study heterogeneity and the quality of individual studies, currently the quantitative benefit for the individual patient cannot be estimated and future controlled, randomized studies with assessment of symptom burden, functional status and quality of life are still required not only to quantify the benefit of MitraClip therapy with reference to conservative therapy, but also to identify patient groups who will mostly benefit.
References
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M (2006) Burden of valvular heart diseases: a population-based study. Lancet 368(9540):1005–1011. doi:10.1016/S0140-6736(06)69208-8
Armeni P, Boscolo PR, Tarricone R, Capodanno D, Maggioni AP, Grasso C, Tamburino C, Maisano F (2016) Real-world cost effectiveness of MitraClip combined with Medical Therapy Versus Medical therapy alone in patients with moderate or severe mitral regurgitation. Int J Cardiol 209:153–160. doi:10.1016/j.ijcard.2016.01.212
Trochu JN, Le Tourneau T, Obadia JF, Caranhac G, Beresniak A (2015) Economic burden of functional and organic mitral valve regurgitation. Arch Cardiovasc Dis 108(2):88–96. doi:10.1016/j.acvd.2014.09.008
Mirabel M, Iung B, Baron G, Messika-Zeitoun D, Detaint D, Vanoverschelde JL, Butchart EG, Ravaud P, Vahanian A (2007) What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J 28(11):1358–1365. doi:10.1093/eurheartj/ehm001
Schwencke C, Bijuklic K, Ouarrak T, Lubos E, Schillinger W, Plicht B, Eggebrecht H, Baldus S, Schymik G, Boekstegers P, Hoffmann R, Senges J, Schofer J (2017) Impact of cardiac comorbidities on early and 1-year outcome after percutaneous mitral valve interventions: data from the German transcatheter mitral valve interventions (TRAMI) registry. Clin Res Cardiol 106(4):249–258. doi:10.1007/s00392-016-1044-3
Wallenborn J, Stork S, Herrmann S, Kukuy O, Fette G, Puppe F, Gorski A, Hu K, Voelker W, Ertl G, Weidemann F (2016) Prevalence of severe mitral regurgitation eligible for edge-to-edge mitral valve repair (MitraClip). Clin Res Cardiol 105(8):699–709. doi:10.1007/s00392-016-0975-z
De Bonis M, Al-Attar N, Antunes M, Borger M, Casselman F, Falk V, Folliguet T, Iung B, Lancellotti P, Lentini S, Maisano F, Messika-Zeitoun D, Muneretto C, Pibarot P, Pierard L, Punjabi P, Rosenhek R, Suwalski P, Vahanian A, Wendler O, Prendergast B (2016) Surgical and interventional management of mitral valve regurgitation: a position statement from the European Society of Cardiology Working Groups on Cardiovascular Surgery and Valvular Heart Disease. Eur Heart J 37(2):133–139. doi:10.1093/eurheartj/ehv322
Feldman T, Foster E, Glower DD, Kar S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L (2011) Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 364(15):1395–1406. doi:10.1056/NEJMoa1009355
Maisano F, Franzen O, Baldus S, Schafer U, Hausleiter J, Butter C, Ussia GP, Sievert H, Richardt G, Widder JD, Moccetti T, Schillinger W (2013) Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol 62(12):1052–1061. doi:10.1016/j.jacc.2013.02.094
Mauri L, Garg P, Massaro JM, Foster E, Glower D, Mehoudar P, Powell F, Komtebedde J, McDermott E, Feldman T (2010) The EVEREST II Trial: design and rationale for a randomized study of the evalve mitraclip system compared with mitral valve surgery for mitral regurgitation. Am Heart J 160(1):23–29. doi:10.1016/j.ahj.2010.04.009
Nickenig G, Estevez-Loureiro R, Franzen O, Tamburino C, Vanderheyden M, Luscher TF, Moat N, Price S, Dall’Ara G, Winter R, Corti R, Grasso C, Snow TM, Jeger R, Blankenberg S, Settergren M, Tiroch K, Balzer J, Petronio AS, Buttner HJ, Ettori F, Sievert H, Fiorino MG, Claeys M, Ussia GP, Baumgartner H, Scandura S, Alamgir F, Keshavarzi F, Colombo A, Maisano F, Ebelt H, Aruta P, Lubos E, Plicht B, Schueler R, Pighi M, Di Mario C (2014) Percutaneous mitral valve edge-to-edge repair: in-hospital results and 1-year follow-up of 628 patients of the 2011–2012 Pilot European Sentinel Registry. J Am Coll Cardiol 64(9):875–884. doi:10.1016/j.jacc.2014.06.1166
Puls M, Lubos E, Boekstegers P, von Bardeleben RS, Ouarrak T, Butter C, Zuern CS, Bekeredjian R, Sievert H, Nickenig G, Eggebrecht H, Senges J, Schillinger W (2016) One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German transcatheter mitral valve interventions registry. Eur Heart J 37(8):703–712. doi:10.1093/eurheartj/ehv627
Zuern CS, Bauer A, Lubos E, Boekstegers P, Puls M, Bardeleben RS, Ouarrak T, Butter C, Eggebrecht H, Nickenig G, Zahn R, Senges J, May AE (2015) Influence of non-cardiac comorbidities on outcome after percutaneous mitral valve repair: results from the German transcatheter mitral valve interventions (TRAMI) registry. Clin Res Cardiol 104(12):1044–1053. doi:10.1007/s00392-015-0872-x
Abdelghani M, Cavalcante R, Miyazaki Y, de Winter RJ, Sarmento-Leite R, Mangione JA, Abizaid A, Lemos PA, Serruys PW, de Brito FS Jr. (2017) Prevalence, predictors, and prognostic implications of residual impairment of functional capacity after transcatheter aortic valve implantation. Clin Res Cardiol. doi:10.1007/s00392-017-1119-9
Bunz M, Lenski D, Wedegartner S, Ukena C, Karbach J, Bohm M, Kindermann I (2016) Heart-focused anxiety in patients with chronic heart failure before implantation of an implantable cardioverter defibrillator: baseline findings of the Anxiety-CHF Study. Clin Res Cardiol 105(3):216–224. doi:10.1007/s00392-015-0909-1
Boekstegers P, Hausleiter J, Baldus S, von Bardeleben RS, Beucher H, Butter C, Franzen O, Hoffmann R, Ince H, Kuck KH, Rudolph V, Schafer U, Schillinger W, Wunderlich N (2014) Percutaneous interventional mitral regurgitation treatment using the Mitra-Clip system. Clin Res Cardiol 103(2):85–96. doi:10.1007/s00392-013-0614-x
Rasekaba T, Lee AL, Naughton MT, Williams TJ, Holland AE (2009) The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J 39(8):495–501. doi:10.1111/j.1445-5994.2008.01880.x
Rector TS, Kubo SH, Cohn JN (1987) Patients’ self-assessment of their congestive heart failure: content, reliability, and validity of a new measure, the Minnesota Living with Heart Failure questionnaire. Heart Fail 3:198–209
Muller-Nordhorn J, Roll S, Willich SN (2004) Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart 90(5):523–527
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. doi:10.1371/journal.pmed.1000100
Gonzalez FM, Finch AP, Armeni P, Boscolo PR, Tarricone R (2015) Comparative effectiveness of Mitraclip plus medical therapy versus medical therapy alone in high-risk surgical patients: a comprehensive review. Expert Rev Med Devices 12(4):471–485. doi:10.1586/17434440.2015.1054807
D’Ascenzo F, Moretti C, Marra WG, Montefusco A, Omede P, Taha S, Castagno D, Gaemperli O, Taramasso M, Frea S, Pidello S, Rudolph V, Franzen O, Braun D, Giannini C, Ince H, Perl L, Zoccai G, Marra S, D’Amico M, Maisano F, Rinaldi M, Gaita F (2015) Meta-analysis of the usefulness of Mitraclip in patients with functional mitral regurgitation. Am J Cardiol 116(2):325–331. doi:10.1016/j.amjcard.2015.04.025
Bail DH (2015) (Meta)-analysis of safety and efficacy following edge-to-edge mitral valve repair using the MitraClip system. J Interv Cardiol 28(1):69–75. doi:10.1111/joic.12168
Philip F, Athappan G, Tuzcu EM, Svensson LG, Kapadia SR (2014) MitraClip for severe symptomatic mitral regurgitation in patients at high surgical risk: a comprehensive systematic review. Catheter Cardiovasc Interv 84(4):581–590. doi:10.1002/ccd.25564
Wan B, Rahnavardi M, Tian DH, Phan K, Munkholm-Larsen S, Bannon PG, Yan TD (2013) A meta-analysis of MitraClip system versus surgery for treatment of severe mitral regurgitation. Ann Cardiothorac Surg 2(6):683–692. doi:10.3978/j.issn.2225-319X.2013.11.02
Orban M, Braun D, Sonne C, Thaler R, Grebmer C, Lesevic H, Schomig A, Mehilli J, Massberg S, Hausleiter J (2014) Dangerous liaison: successful percutaneous edge-to-edge mitral valve repair in patients with end-stage systolic heart failure can cause left ventricular thrombus formation. EuroIntervention 10(2):253–259. doi:10.4244/EIJV10I2A41
Munkholm-Larsen S, Wan B, Tian DH, Kearney K, Rahnavardi M, Dixen U, Kober L, Alfieri O, Yan TD (2014) A systematic review on the safety and efficacy of percutaneous edge-to-edge mitral valve repair with the MitraClip system for high surgical risk candidates. Heart 100(6):473–478. doi:10.1136/heartjnl-2013-304049
Kind P (1996) Quality of life and pharmacoeconomics in clinical trials. The EuroQoL instrument: an index of health-related quality of life. Lippincott-Raven, Philadelphia, pp 191–201
Wiebe J, Franke J, Lubos E, Boekstegers P, Schillinger W, Ouarrak T, May AE, Eggebrecht H, Kuck KH, Baldus S, Senges J, Sievert H (2014) Percutaneous mitral valve repair with the MitraClip system according to the predicted risk by the logistic EuroSCORE: preliminary results from the German Transcatheter Mitral Valve Interventions (TRAMI) Registry. Catheter Cardiovasc Interv 84(4):591–598. doi:10.1002/ccd.25493
Puls M, Tichelbacker T, Bleckmann A, Hunlich M, von der Ehe K, Beuthner BE, Ruter K, Beissbarth T, Seipelt R, Schondube F, Hasenfuss G, Schillinger W (2014) Failure of acute procedural success predicts adverse outcome after percutaneous edge-to-edge mitral valve repair with MitraClip. EuroIntervention 9(12):1407–1417. doi:10.4244/EIJV9I12A238
Schueler R, Momcilovic D, Weber M, Welz A, Werner N, Mueller C, Ghanem A, Nickenig G, Hammerstingl C (2014) Acute changes of mitral valve geometry during interventional edge-to-edge repair with the MitraClip system are associated with midterm outcomes in patients with functional valve disease: preliminary results from a prospective single-center study. Circ Cardiovasc Interv 7(3):390–399. doi:10.1161/CIRCINTERVENTIONS.113.001098
Pleger ST, Schulz-Schonhagen M, Geis N, Mereles D, Chorianopoulos E, Antaredja M, Lewening M, Katus HA, Bekeredjian R (2013) One year clinical efficacy and reverse cardiac remodelling in patients with severe mitral regurgitation and reduced ejection fraction after MitraClip implantation. Eur J Heart Fail 15(8):919–927. doi:10.1093/eurjhf/hft046
Neuss M, Schau T, Schoepp M, Seifert M, Holschermann F, Meyhofer J, Butter C (2013) Patient selection criteria and midterm clinical outcome for MitraClip therapy in patients with severe mitral regurgitation and severe congestive heart failure. Eur J Heart Fail 15(7):786–795. doi:10.1093/eurjhf/hfs214
Tigges E, Kalbacher D, Thomas C, Appelbaum S, Deuschl F, Schofer N, Schluter M, Conradi L, Schirmer J, Treede H, Reichenspurner H, Blankenberg S, Schafer U, Lubos E (2016) Transcatheter mitral valve repair in surgical high-risk patients: gender-specific acute and long-term outcomes. Biomed Res Int 2016:3934842. doi:10.1155/2016/3934842
Nikendei C, Schafer H, Weisbrod M, Huber J, Geis N, Katus HA, Bekeredjian R, Herzog W, Pleger ST, Schultz JH (2016) The effects of mitral valve repair on memory performance, executive function, and psychological measures in patients with heart failure. Psychosom Med 78(4):432–442. doi:10.1097/PSY.0000000000000284
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al (2016) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 14 July 2016
Ahmed A, Aronow WS, Fleg JL (2006) Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J 151(2):444–450. doi:10.1016/j.ahj.2005.03.066
Wyrwich KW, Spertus JA, Kroenke K, Tierney WM, Babu AN, Wolinsky FD (2004) Clinically important differences in health status for patients with heart disease: an expert consensus panel report. Am Heart J 147(4):615–622. doi:10.1016/j.ahj.2003.10.039
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 14(6):1523–1532
Rector TS, Tschumperlin LK, Kubo SH, Bank AJ, Francis GS, McDonald KM, Keeler CA, Silver MA (1995) Use of the Living With Heart Failure questionnaire to ascertain patients’ perspectives on improvement in quality of life versus risk of drug-induced death. J Card Fail 1(3):201–206
Ferreira JP, Duarte K, Graves TL, Zile MR, Abraham WT, Weaver FA, Lindenfeld J, Zannad F (2016) Natriuretic peptides, 6-min walk test, and quality-of-life questionnaires as clinically meaningful endpoints in HF trials. J Am Coll Cardiol 68(24):2690–2707. doi:10.1016/j.jacc.2016.09.936
Stone GW, Vahanian AS, Adams DH, Abraham WT, Borer JS, Bax JJ, Schofer J, Cutlip DE, Krucoff MW, Blackstone EH, Genereux P, Mack MJ, Siegel RJ, Grayburn PA, Enriquez-Sarano M, Lancellotti P, Filippatos G, Kappetein AP (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 1: clinical trial design principles: a consensus document from the mitral valve academic research consortium. Eur Heart J 36(29):1851–1877. doi:10.1093/eurheartj/ehv281
Stone GW, Adams DH, Abraham WT, Kappetein AP, Genereux P, Vranckx P, Mehran R, Kuck KH, Leon MB, Piazza N, Head SJ, Filippatos G, Vahanian AS (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 2: endpoint definitions: a consensus document from the Mitral Valve Academic Research Consortium. Eur Heart J 36(29):1878–1891. doi:10.1093/eurheartj/ehv333
Glower DD, Kar S, Trento A, Lim DS, Bajwa T, Quesada R, Whitlow PL, Rinaldi MJ, Grayburn P, Mack MJ, Mauri L, McCarthy PM, Feldman T (2014) Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. J Am Coll Cardiol 64(2):172–181. doi:10.1016/j.jacc.2013.12.062
Higgins JPT (2011) Selecting studies and collecting data, Chap. 7. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration. http://www.handbook.cochrane.org
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Haney EM, Huffman LH, Bougatsos C, Freeman M, Fu R, Steiner RD, Helfand M, Nelson HD (2007). In: Screening for lipid disorders in children and adolescents. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Rockville
Cacela D, Fiarresga A, Branco L, Galrinho A, Rio P, Selas M, Ferreira R (2015) Percutaneous treatment of mitral valve regurgitation: initial experience with the MitraClip device. Port J Cardiol 34(9):515–524. doi:10.1016/j.repc.2015.04.004
Lesevic H, Sonne C, Braun D, Orban M, Pache J, Kastrati A, Schomig A, Mehilli J, Barthel P, Ott I, Sack G, Massberg S, Hausleiter J (2015) Acute and midterm outcome after MitraClip therapy in patients with severe mitral regurgitation and left ventricular dysfunction. Am J Cardiol 116(5):749–756. doi:10.1016/j.amjcard.2015.05.048
Vitarelli A, Mangieri E, Capotosto L, Tanzilli G, D’Angeli I, Viceconte N, Placanica A, Placanica G, Cocco N, Ashurov R, Al-Kindy S (2015) Assessment of biventricular function by three-dimensional speckle-tracking echocardiography in secondary mitral regurgitation after repair with the MitraClip system. J Am Soc Echocardiogr 28(9):1070–1082. doi:10.1016/j.echo.2015.04.005
Hellhammer K, Balzer J, Zeus T, Rammos C, Niebel S, Kubatz L, Wagstaff R, Kelm M, Rassaf T (2015) Percutaneous mitral valve repair using the MitraClip system in patients with anemia. Int J Cardiol 184:399–404. doi:10.1016/j.ijcard.2015.02.081
Carrasco-Chinchilla F, Arzamendi D, Romero M, Gimeno de Carlos F, Alonso-Briales JH, Li CH, Mesa MD, Arnold R, Serrador Frutos AM, Pan M, Roig E, Rodriguez-Bailon I, de la Fuente Galan L, Hernandez JM, Serra A, Suarez de Lezo J (2014) Initial experience of percutaneous treatment of mitral regurgitation with MitraClip(R) therapy in Spain. Rev Esp Cardiol (Engl Ed) 67(12):1007–1012. doi:10.1016/j.rec.2014.02.019
Matsumoto T, Nakamura M, Yeow WL, Hussaini A, Ram V, Makar M, Gurudevan SV, Trento A, Siegel RJ, Kar S (2014) Impact of pulmonary hypertension on outcomes in patients with functional mitral regurgitation undergoing percutaneous edge-to-edge repair. Am J Cardiol 114(11):1735–1739. doi:10.1016/j.amjcard.2014.08.044
van Riel AC, Boerlage-van Dijk K, de Bruin-Bon RH, Araki M, Koch KT, Vis MM, Meregalli PG, van den Brink RB, Piek JJ, Mulder BJ, Baan J Jr, Bouma BJ (2014) Percutaneous mitral valve repair preserves right ventricular function. J Am Soc Echocardiogr 27(10):1098–1106. doi:10.1016/j.echo.2014.06.001
Vandendriessche T, Kotrc M, Tijskens M, Bartunek J, Delesie M, Paelinck BP, De Bock D, Penicka M, Stockman B, De Maeyer C, Vrints C, Vanderheyden M, Claeys MJ (2014) Percutaneous mitral valve repair in high-risk patients: initial experience with the Mitraclip system in Belgium. Acta Cardiol 69(3):265–270. doi:10.2143/AC.69.3.3027829
Taramasso M, Maisano F, Denti P, Latib A, La Canna G, Colombo A, Alfieri O (2014) Percutaneous edge-to-edge repair in high-risk and elderly patients with degenerative mitral regurgitation: midterm outcomes in a single-center experience. J Thorac Cardiovasc Surg 148(6):2743–2750. doi:10.1016/j.jtcvs.2014.03.036
Koifman E, Fefer P, Hay I, Feinberg M, Maor E, Guetta V (2014) MitraClip implantation for high risk patients with severe mitral regurgitation: the Sheba experience. Isr Med Assoc J 16(2):91–95
Taramasso M, Maisano F, Latib A, Denti P, Buzzatti N, Cioni M, La Canna G, Colombo A, Alfieri O (2014) Clinical outcomes of MitraClip for the treatment of functional mitral regurgitation. EuroIntervention 10(6):746–752. doi:10.4244/EIJV10I6A128
Bozdag-Turan I, Paranskaya L, Birkemeyer R, Turan RG, Kische S, Akin I, Ortak J, Stoeckicht Y, Schubert J, Westphal B, Nienaber CA, Ince H (2014) Percutaneous mitral repair with the MitraClip system in patients with mild-to-moderate and severe heart failure: a single-centre experience. Cardiovasc Ther 32(2):66–73. doi:10.1111/1755-5922.12058
Perl L, Vaturi M, Assali A, Shapira Y, Bruckheimer E, Ben-Gal T, Vaknin-Assa H, Sagie A, Kornowski R (2013) Preliminary experience using the transcatheter mitral valve leaflet repair procedure. Isr Med Assoc J 15(10):608–612
Estevez-Loureiro R, Franzen O, Winter R, Sondergaard L, Jacobsen P, Cheung G, Moat N, Ihlemann N, Ghione M, Price S, Duncan A, Streit Rosenberg T, Barker S, Di Mario C, Settergren M (2013) Echocardiographic and clinical outcomes of central versus noncentral percutaneous edge-to-edge repair of degenerative mitral regurgitation. J Am Coll Cardiol 62(25):2370–2377. doi:10.1016/j.jacc.2013.05.093
Armoiry X, Brochet E, Lefevre T, Guerin P, Dumonteil N, Himbert D, Cormier B, Piriou N, Gautier M, Messika-Zeitoun D, Romano M, Rioufol G, Warin Fresse K, Boudou N, Leclercq F, Bedossa M, Obadia JF (2013) Initial French experience of percutaneous mitral valve repair with the MitraClip: a multicentre national registry. Arch Cardiovasc Dis 106(5):287–294. doi:10.1016/j.acvd.2013.03.059
Surder D, Pedrazzini G, Gaemperli O, Biaggi P, Felix C, Rufibach K, der Maur CA, Jeger R, Buser P, Kaufmann BA, Moccetti M, Hurlimann D, Buhler I, Bettex D, Scherman J, Pasotti E, Faletra FF, Zuber M, Moccetti T, Luscher TF, Erne P, Grunenfelder J, Corti R (2013) Predictors for efficacy of percutaneous mitral valve repair using the MitraClip system: the results of the MitraSwiss registry. Heart 99(14):1034–1040. doi:10.1136/heartjnl-2012-303105
Spargias K, Chrissoheris M, Halapas A, Nikolaou J, Tsolakis A, Bouboulis N, Pattakos S (2012) Percutaneous mitral valve repair using the edge-to-edge technique: first Greek experience. Hell J Cardiol 53(5):343–351
Ussia GP, Cammalleri V, Sarkar K, Scandura S, Imme S, Pistritto AM, Caggegi A, Chiaranda M, Mangiafico S, Barbanti M, Scarabelli M, Mule M, Aruta P, Tamburino C (2012) Quality of life following percutaneous mitral valve repair with the MitraClip system. Int J Cardiol 155(2):194–200. doi:10.1016/j.ijcard.2011.08.853
Ihlemann N, Franzen O, Jorgensen E, Hansen PB, Hassager C, Moller JE, Sondergaard L (2011) Promising results after percutaneous mitral valve repair. Dan Med Bull 58(7):A4299
Feldman T, Kar S, Rinaldi M, Fail P, Hermiller J, Smalling R, Whitlow PL, Gray W, Low R, Herrmann HC, Lim S, Foster E, Glower D (2009) Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol 54(8):686–694. doi:10.1016/j.jacc.2009.03.077
Kasner M, Gast M, Galuszka O, Stroux A, Rutschow S, Wang X, Dohmen P, Skurk C, Landmesser U, Poller W, Gross M (2016) Circulating exosomal microRNAs predict functional recovery after MitraClip repair of severe mitral regurgitation. Int J Cardiol 215:402–405. doi:10.1016/j.ijcard.2016.04.018
Adamo M, Chiari E, Curello S, Maiandi C, Chizzola G, Fiorina C, Frontini M, Cuminetti G, Pezzotti E, Rovetta R, Lombardi CM, Manzato A, Metra M, Ettori F (2016) Mitraclip therapy in patients with functional mitral regurgitation and missing leaflet coaptation: is it still an exclusion criterion? Eur J Heart Fail 18(10):1278–1286. doi:10.1002/ejhf.520
Sorajja P, Mack M, Vemulapalli S, Holmes DR Jr, Stebbins A, Kar S, Lim DS, Thourani V, McCarthy P, Kapadia S, Grayburn P, Pedersen WA, Ailawadi G (2016) Initial experience with commercial transcatheter mitral valve repair in the United States. J Am Coll Cardiol 67(10):1129–1140. doi:10.1016/j.jacc.2015.12.054
Azzalini L, Millan X, Khan R, Couture P, Ducharme A, Basmadjian A, Bonan R, Asgar AW (2016) Impact of left ventricular function on clinical outcomes of functional mitral regurgitation patients undergoing transcatheter mitral valve repair. Catheter Cardiovasc Interv. doi:10.1002/ccd.26460
Ussia GP, Cammalleri V, Mazzotta E, Pascuzzo G, Muscoli S, Marchei M, Macrini M, Anceschi A, Romeo F (2016) Cardiovascular medicine heart failure (CVM-HF) index as prognostic model for candidates to MitraClip therapy. Heart Vessels 31(10):1633–1642. doi:10.1007/s00380-015-0772-z
Tay E, Muda N, Yap J, Muller DW, Santoso T, Walters DL, Liu X, Yamen E, Jansz P, Yip J, Zambahari R, Passage J, Ding ZP, Wang J, Scalia G, Soesanto AM, Yeo KK (2016) The MitraClip Asia-Pacific registry: differences in outcomes between functional and degenerative mitral regurgitation. Catheter Cardiovasc Interv 87(7):E275–E281. doi:10.1002/ccd.26289
Van den Branden BJ, Swaans MJ, Post MC, Rensing BJ, Eefting FD, Jaarsma W, Van der Heyden JA (2012) Percutaneous edge-to-edge mitral valve repair in high-surgical-risk patients: do we hit the target? JACC Cardiovasc Interv 5(1):105–111. doi:10.1016/j.jcin.2011.09.013
Giannini C, Fiorelli F, De Carlo M, Guarracino F, Faggioni M, Giordano P, Spontoni P, Pieroni A, Petronio AS (2016) Comparison of percutaneous mitral valve repair versus conservative treatment in severe functional mitral regurgitation. Am J Cardiol 117(2):271–277. doi:10.1016/j.amjcard.2015.10.044
Schueler R, Nickenig G, May AE, Schillinger W, Bekeredjian R, Ouarrak T, Schofer J, Hehrlein C, Sievert H, Boekstegers P, Lubos E, Hoffmann R, Baldus S, Senges J, Hammerstingl C (2016) Predictors for short-term outcomes of patients undergoing transcatheter mitral valve interventions: analysis of 778 prospective patients from the German TRAMI registry focusing on baseline renal function. EuroIntervention 12(4):508–514. doi:10.4244/EIJY15M09_07
Kobe J, Hucklenbroich K, Geisendorfer N, Bettin M, Frommeyer G, Reinke F, Dechering D, Burgmer M, Eckardt L (2017) Posttraumatic stress and quality of life with the totally subcutaneous compared to conventional cardioverter-defibrillator systems. Clin Res Cardiol 106(5):317–321. doi:10.1007/s00392-016-1055-0
Tan MK, Jarral OA, Thong EH, Kidher E, Uppal R, Punjabi PP, Athanasiou T (2017) Quality of life after mitral valve intervention. Interact Cardiovasc Thorac Surg 24(2):265–272. doi:10.1093/icvts/ivw312
Stone GW, Vahanian AS, Adams DH, Abraham WT, Borer JS, Bax JJ, Schofer J, Cutlip DE, Krucoff MW, Blackstone EH, Genereux P, Mack MJ, Siegel RJ, Grayburn PA, Enriquez-Sarano M, Lancellotti P, Filippatos G, Kappetein AP (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 1: clinical trial design principles: a consensus document from the mitral valve academic research consortium. J Am Coll Cardiol 66(3):278–307. doi:10.1016/j.jacc.2015.05.046
Stone GW, Adams DH, Abraham WT, Kappetein AP, Genereux P, Vranckx P, Mehran R, Kuck KH, Leon MB, Piazza N, Head SJ, Filippatos G, Vahanian AS (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 2: endpoint definitions: a consensus document from the mitral valve academic research consortium. J Am Coll Cardiol 66(3):308–321. doi:10.1016/j.jacc.2015.05.049
Bagur R, Rodes-Cabau J, Dumont E, De Larochelliere R, Doyle D, Pibarot P, Cote M, Clavel MA, Villeneuve J, Gutierrez M, Poirier P, Bertrand OF (2011) Performance-based functional assessment of patients undergoing transcatheter aortic valve implantation. Am Heart J 161(4):726–734. doi:10.1016/j.ahj.2010.12.024
Raphael C, Briscoe C, Davies J, Ian Whinnett Z, Manisty C, Sutton R, Mayet J, Francis DP (2007) Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart 93(4):476–482. doi:10.1136/hrt.2006.089656
Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, Kocovic DZ, Packer M, Clavell AL, Hayes DL, Ellestad M, Trupp RJ, Underwood J, Pickering F, Truex C, McAtee P, Messenger J (2002) Cardiac resynchronization in chronic heart failure. N Engl J Med 346(24):1845–1853. doi:10.1056/NEJMoa013168
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Iliadis, C., Lee, S., Kuhr, K. et al. Functional status and quality of life after transcatheter mitral valve repair: a prospective cohort study and systematic review. Clin Res Cardiol 106, 1005–1017 (2017). https://doi.org/10.1007/s00392-017-1150-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1150-x