Abstract
Health-related quality of life (HRQoL) is increasingly used as an outcome measure in surgery. This concept is of particular importance to intervention on the mitral valve (MV), in view of guidelines recommending early intervention on patients even if they are asymptomatic. Transcatheter MV procedures are continuously evolving and requires robust assessment, of which HRQoL is an important parameter. This chapter reviews all available literature surrounding HRQoL outcomes in patients undergoing transcatheter MV interventions. While certain aspects of the literature were lacking, for example the lack of baseline HRQoL measurements in the majority of studies, most studies confirm that HRQoL benefits of transcatheter MV interventions is generally acceptable, with certain populations showing better HRQoL when compared to age- and gender-matched normal populations. This chapter also provides ideas for future research into HRQoL in transcatheter MV interventions, including establishing a common HRQoL instrument for disease-specific use, running randomised studies with baseline and follow-up HRQoL measured at specific predefined timepoints, and other innovative research areas including correlation of HRQoL with physical activity monitors, physiological biomarkers and radiological markers (e.g. leaflet stress from MRI and echocardiography) used as innovative markers of functional outcome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Increasingly, emphasis has been placed on health-related quality of life (HRQoL) as a measure of outcome in surgery. Defined as a “multi -dimensional assessment of an individual’s perception of the physical, psychological, and social aspects of life that can be affected by a disease process and its treatment”, it provides a more nuanced look at the outcomes following surgery when compared to crude mortality and morbidity rates. It is also necessary for the calculation and evaluation of cost-effectiveness as well as acting as a more precise indicator of patient-centred care, with significant promise to improve healthcare provision [1] – this has been recognised by the United Kingdom’s Department of Health with the consolidation of efforts to collect and publish HRQoL outcomes for common procedures [2].
While not routinely collected in cardiothoracic or valve surgery currently, this concept is particularly applicable to intervention on the mitral valve (MV), including transcatheter MV procedures, for a few reasons. Firstly, AHA/ACC and ESC/EACTS guidelines recommend early intervention on severe degenerative mitral regurgitation (MR) even if patients are asymptomatic [3,4,5]. Measurement and maintenance of pre-operative HRQoL is therefore essential in maintaining the confidence of patients and referring cardiologists. Secondly, transcatheter MV procedures are rapidly evolving and require robust assessment prior to widespread use. Knowledge of HRQoL outcomes in these new technologies will benefit both clinicians and patients in their decision-making.
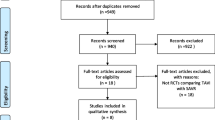
This chapter aims to provide readers with a comprehensive systematic review of all available literature detailing HRQoL outcomes in patients undergoing transcatheter MV interventions. This chapter will also make recommendations for clinical practice and future research.
MitraClip Implantation
The MitraClip, as its name suggests, is a clip that grasps the anterior and posterior leaflets of the mitral valve, creating a “double orifice” valve that reduces the extent of regurgitation. In the current literature on transcatheter MV interventions, the majority of studies (n = 20) reported on MitraClip implantation (Table 8.1 adapted from Tan et al. [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]), the largest group of studies on a single device. All showed significant HRQoL improvements post-implantation. Three studies compared MitraClip to conventional surgery [8, 10, 20] while two studies compared this device to conservative management [7, 14].
Studies Comparing Against Conventional Surgery
Buzzatti et al. compared conventional MV surgery in 35 retrospectively selected patients to 25 octogenarian patients who underwent MitraClip implantation [8]. Importantly, this older patient population showed significantly improved SF-36 physical scores but failed to show improvement in the mental components. On comparing with the conventional surgery group, both groups had similar post-operative physical and mental HRQoL scores. Due to the lack of baseline measurement in the conventional surgery group, it was not possible to compare HRQoL improvements between groups. This finding was supported by Rudolph et al., which observed significant improvement in MLHFQ scores in 104 patients with prohibitive surgical risk [20]. In a randomised controlled trial by Feldman et al., the MitraClip was compared to conventional surgery, showing HRQoL improvements in both groups [10]. Patients undergoing conventional procedures experienced a transient decrease in HRQoL 30-days post-surgery attributed to the invasive nature of the surgeries. In patients with life expectancy less than a year or two, this finding is likely to support the argument for percutaneous therapy.
Studies Comparing Against Conservative Management
Both studies from Arnold et al. and Krawczyk-Ożóg et al. showed that patients with MR secondary to HF treated conservatively had no difference in HRQoL at all follow-up timepoints [7, 14]. In contrast, patients treated with the MitraClip showed improvements in HRQoL post-operatively. Arnold et al. showed incrementally higher SF-36 scores at each timepoint, with early 1-month improvements sustained till the end of the 2-year follow-up period [7]. This was echoed in Krawczyk-Ożóg et al. which showed significant improvement in EQ-5D and SF-12v2 scores at follow-up, although the specific time of HRQoL measurement was not stated [14].
Studies Considering High-Risk or Frail Patients
A number of studies considered patients who were undergoing MitraClip implantation who were elderly, frail or of prohibitive surgical risk [9, 12, 15, 17, 20, 21, 24,25,26]. Edelman et al. was an early small cohort study looking at the use of MitraClip in 25 high-risk patients, showing improvements in MLHFQ and AQoL-6D scores from baseline [9]. This was also seen in a larger cohort study by Rudolph et al., 803 patients divided into groups based on NYHA functional class [21]. Baseline HRQoL varied between classes, with worsening HRQoL with increasing heart failure severity and class IV patients having the worst baseline EQ-5D scores. Although patients with class IV heart failure were also shown to have the worst HRQoL at 30-days post-MitraClip implantation, this was still significantly improved from baseline. Similarly, in a cohort study by Neuss et al., 157 very high-risk patients (all EuroSCORE >20) with severe heart failure showed persistent improvements in MLHFQ scores at 1-year post-MitraClip implantation. This HRQoL improvement was also shown in the EVEREST II trials performed by Glower et al., which studied a patient population with a significant proportion of patients in NYHA class III/IV [12]. In another prospective study in a high-risk population, Ussia et al. found significant improvement in all SF-12 components except for bodily pain [24]. Lim et al. evaluated treatment of MR in 141 patients at prohibitive surgical risk, finding improvements in both PCS and MCS of the SF-36 [15], and echoed in cohort studies by Van den Branden et al. [25] and Whitlow et al. [26]. This was also the case in a cohort study from Rudolph et al., which showed MLHFQ scores improving significantly in patients at prohibitive surgical risk. Again, scores improvements were comparable with those reported in MV surgery [20]. Finally, a post-approval study by Reichenspurner et al. considered the use of the MitraClip in both high-risk and low-risk groups of patients with degenerative MR. While overall HRQoL scores in the patient population improved at 12-months follow-up, the study unfortunately failed to determine if there was any significant differences between the improvements seen in either group [19].
Interestingly, a more recent study by Metze et al. showed while frail patients had similar improvements in SF-36 scores to non-frail patients after undergoing the MitraClip procedure, these frail patients showed significantly greater improvement MLHFQ scores. This suggests that patients previously considered unfit for conventional surgery should not only be considered for percutaneous therapy but might indeed benefit more from interventional therapies than fitter candidates, at least from a HRQoL point of view. This is also true for elderly candidates – while baseline HRQoL is worse with increasing age [22], HRQoL improvements are significant post-MitraClip intervention [15, 22] and comparable to population norms for the elderly population [15].
Miscellaneous Studies
The impact of anaemia was considered in a study by Hellhammer et al., which compared 41 anaemic patients to 39 patients without anaemia. While HRQoL improved in both groups, no significant difference was seen between the improvements in HRQoL between the groups [13]. Terhoeven et al. specifically observed the impact of MitraClip on the psychological and cognitive functioning of 40 patients using the SF-36, showing improved mental wellbeing post-MitraClip implantation [23].
Cardioband Implantation
The Cardioband Mitral system is a transcatheter device that aims to reduce annular reduction and thus reduce functional MR. Through deploying between 12 to 17 anchors around the mitral annulus, the Cardioband implant is affixed around the annulus. The implant is then used to cinch the diameter of the mitral annulus, improving the coaptation of the cusps and decreasing MR severity. Two prospective cohort studies reported outcomes on Cardioband implantation (Table 8.2) [27, 28]. Nickenig et al. showed that MLHFQ scores improved from baseline at 6-month follow-up [28]. This was also seen in a more recent 1-year follow-up study by Messika-Zeitoun et al., with improvement of MLHFQ scores at 6-months. This improvement was sustained at 12-months post-operatively [27].
Carillon Mitral Contour Device
The Carillon Mitral Contour system is a right-heart transcatheter MV repair system designed for patients with functional MR. It is deployed and positioned within the coronary sinus or great cardiac vein, with the double-anchor designed to apply pressure onto the mitral annulus and improve the coaptation of the cusps by this modification of the annulus’ shape. Three studies reported outcomes from the use of this device (Table 8.3 adapted from Tan et al. [6, 29, 31]).
Schofer et al. used the device as a therapeutic adjunct to standard care and showed 6-month post-intervention KCCQ scores to be significantly improved from baseline. In this score, the patient portion of the global assessment score was significantly improved in the majority of the 30 patients studied [29]. This was supported by the functional assessment of 14 patients after Carillon device implantation by Wołoszyn et al. [31]. KCCQ scores were improved at 1-month, comparable to the improvement seen by Schofer et al. [29]. This is likely due to the significant reduction in MR observed. A third study by Siminiak et al. observed the effectiveness of the Carillon system in improving functional MR. This study compared patients with permanent implants to those who had recaptured devices, and those with the permanent implants had higher HRQoL at 1-year follow-up [30].
Studies Including Other Percutaneous MV Interventions
Four studies reported outcomes from other percutaneous MV interventions (Table 8.4 adapted from Tan et al. [6, 32,33,34,35]). In a cohort study using the PASCAL repair system, Lim et al. showed early improvements in KCCQ and EQ-5D scores [33]. HRQoL improvements were seen in a study by Sorajja et al. which used a novel Tendyne prothesis, the only device designed to be an implanted MV valve replacement [35]. One study by MacHaalany et al. on the Viacor percutaneous transvenous mitral annuloplasty device was stopped prematurely after peri-operative complications and mortality, observing no significant HRQOL benefits [34].
Finally, in a registry study using patients undergoing any transcatheter intervention from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry, Arnold et al. looked at the changes in KCCQ scores at 30-day and 1-year post-intervention [32]. This registry study confirms the findings of the individual studies described in this chapter—HRQoL shows early improvement at 30-days and this improvement is maintained till 1-year follow-up. This study also performed a multivariate analysis of risk factors for lower HRQoL post-intervention, showing atrial fibrillation, permanent pacemakers, severe lung disease, long-term home oxygen therapy, and lower baseline HRQoL scores to be associated with poorer HRQoL at early follow-up.
Discussion
This chapter provides a comprehensive overview of the current state of literature detailing HRQoL after percutaneous MV interventions, with predictors of poor HRQoL after such interventions summarised in Fig. 8.1. There is an increasing burden of MV disease with an ageing population [36] and this population is usually deemed to be of high surgical risk and unable to withstand the stresses of invasive surgery. Indeed, up to 50% are declined for conventional MVr or MVR [37, 38]. Thus, there is increasing requirements for less invasive therapeutic approaches, with development of multiple transcatheter or percutaneous devices to meet this demand.
It is promising that most studies confirm that HRQoL improves significantly post-intervention. It is further important to note that the level of post-interventional HRQoL in the patient population is comparable to healthy age-matched populations, including both the elderly and high-risk populations.
Study Limitations
While most studies provided a breakdown of aetiology leading to MV pathology, majority of studies unfortunately did not analyse baseline or HRQoL improvements according to aetiology. Of the 29 studies, many were of observational design with only two (6.9%) having randomisation included in their study design. The absence of randomisation resulted in considerable differences between baseline characteristics of patient cohorts—the typical MV patient presents with multiple chronic co-morbidities and various sequelae from MV disease. Furthermore, HRQoL instruments used and follow-up periods were significantly different between studies, making it difficult to compare outcomes between patients, interventions, and studies.
Whilst the MitraClip was the first of its kind which was designed specifically for a high-risk population, there has been a lack of studies reporting HRQoL after the use of other devices. Of the 29 studies currently available in the literature, nine (31.0%) were on devices other than the MitraClip. Additionally, twelve of these studies (60.0%) reported significant involvement of Abbott Vascular, with authors disclosing links to the company [8, 11, 12, 15, 16, 20, 22, 25, 26] or direct funding [7, 10, 21]. This, while not conclusive, might suggest institutional bias, with increased emphasis on this device due to increased funding. Studies might also fail to report poor outcomes due to conflicts of interest.
Suggestions for Further Research
It is recognised that patients value HRQoL more than clinical variables which are of more interest to clinicians and academics. HRQoL should become an essential tool to evaluate patient-centred benefits in the assessment of established as well as novel transcatheter MV devices. While most studies included in this review used the SF-36 in the assessment of patients’ HRQoL, there is no consensus as to which instrument is best in determining HRQoL in this unique patient population undergoing transcatheter MV interventions and whether a separate disease-specific instrument is required altogether.
In this review, most studies support the fact that transcatheter MV interventions have a significant impact on both physical and mental functioning and this impact is maintained even in elderly and high surgical risk patients. The measurement of physical functioning should be improved further, especially with the improvement of technology in accelerometers and activity monitors. Further research should include activity monitors to monitor physical activity before and after intervention, providing concrete data to reinforce HRQoL conclusions. Wrist-worn accelerometers or even smartphone applications that exploit built-in accelerometers are increasingly available, and these should be incorporated in future studies [39, 40].
Quantifiable predictors of HRQoL changes must also be identified in future research. For example, physiological biomarkers [41] may allow more innovative analysis, correlating magnitude of improvement to changes in these markers. Radiological measures (e.g. leaflet stress from MRI and coaptation depth/degree of left ventricular remodeling from echocardiography) were not analysed in any of the studies and should be used as future markers of functional outcome.
Conclusion
Transcatheter MV interventions are performed on heterogenous populations, with both young and old patients, presenting with a wide range of co-morbidities. This study confirms that HRQoL benefits of transcatheter MV interventions is generally acceptable, with certain populations showing better HRQoL when compared to age- and/or gender-matched normal populations. This improvement is maintained even in high surgical risk, elderly, and frail patients, with innovative percutaneous designs limiting the invasiveness of these interventions (Fig. 8.2). However, there are limitations in the current literature. Future randomised studies would benefit from baseline and follow-up HRQoL measurements at specific time points—this is suggested to be done pre-operatively and at 1-month, 1-year and 5-years post-operatively, enabling the determining of early and late predictors of impaired HRQoL. A common HRQoL instrument should be established, or indeed designed, for disease-specific use in transcatheter MV intervention studies. This would further support detailed comparison between devices. Use of newer technologies such as physical activity monitors, physiological biomarkers and radiological markers (e.g. leaflet stress from MRI and echocardiography) should be used as innovative markers of functional outcome.
References
Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:f167.
Department of Health, Guidance on the routine collection of Patient Reported Outcome Measures (PROMs). 2010.
American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, Bonow RO, Carabello BA, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114(5):e84–231.
Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008;118(15):e523–661.
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardio-Thorac Surg. 2012;42(4):S1–44.
Tan MK, Jarral OA, Thong EH, Kidher E, Uppal R, Punjabi PP, et al. Quality of life after mitral valve intervention. Interact Cardiovasc Thorac Surg. 2017;24(2):265–72.
Arnold SV, Chinnakondepalli KM, Spertus JA, Magnuson EA, Baron SJ, Kar S, et al. Health status after transcatheter mitral-valve repair in heart failure and secondary mitral regurgitation: COAPT trial. J Am Coll Cardiol. 2019;73(17):2123–32.
Buzzatti N, Maisano F, Latib A, Taramasso M, Denti P, La Canna G, et al. Comparison of outcomes of percutaneous MitraClip versus surgical repair or replacement for degenerative mitral regurgitation in octogenarians. Am J Cardiol. 2015;115(4):487–92.
Edelman JJB, Dias P, Passage J, Yamen E. Percutaneous mitral valve repair in a high-risk Australian series. Heart Lung Circ. 2014;23(6):520–6.
Feldman T, Foster E, Glower DD, Kar S, Rinaldi MJ, Fail PS, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364(15):1395–406.
Franzen O, van der Heyden J, Baldus S, Schlüter M, Schillinger W, Butter C, et al. MitraClip® therapy in patients with end-stage systolic heart failure. Eur J Heart Fail. 2011;13(5):569–76.
Glower DD, Kar S, Trento A, Lim DS, Bajwa T, Quesada R, et al. Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. J Am Coll Cardiol. 2014;64(2):172–81.
Hellhammer K, Balzer J, Zeus T, Rammos C, Niebel S, Kubatz L, et al. Percutaneous mitral valve repair using the MitraClip® system in patients with anemia. Int J Cardiol. 2015;184:399–404.
Krawczyk-Ożóg A, Siudak Z, Sorysz D, Hołda MK, Płotek A, Dziewierz A, et al. Comparison of clinical and echocardiographic outcomes and quality of life in patients with severe mitral regurgitation treated by MitraClip implantation or treated conservatively. Postępy W Kardiologii Interwencyjnej. Adv Interv Cardiol. 2018;14(3):291.
Lim DS, Reynolds MR, Feldman T, Kar S, Herrmann HC, Wang A, et al. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol. 2014;64(2):182–92.
Maisano F, Franzen O, Baldus S, Schäfer U, Hausleiter J, Butter C, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol. 2013;62(12):1052–61.
Metze C, Matzik A-S, Scherner M, Körber MI, Michels G, Baldus S, et al. Impact of frailty on outcomes in patients undergoing percutaneous mitral valve repair. JACC Cardiovasc Interv. 2017;10(19):1920–9.
Neuss M, Schau T, Schoepp M, Seifert M, Hölschermann F, Meyhöfer J, et al. Patient selection criteria and midterm clinical outcome for MitraClip therapy in patients with severe mitral regurgitation and severe congestive heart failure. Eur J Heart Fail. 2013;15(7):786–95.
Reichenspurner H, Schillinger W, Baldus S, Hausleiter J, Butter C, Schäefer U, et al. Clinical outcomes through 12 months in patients with degenerative mitral regurgitation treated with the MitraClip® device in the ACCESS-EUrope Phase I trial. Eur J Cardiothorac Surg. 2013;44(4):e280–8.
Rudolph V, Knap M, Franzen O, Schlüter M, de Vries T, Conradi L, et al. Echocardiographic and clinical outcomes of MitraClip therapy in patients not amenable to surgery. J Am Coll Cardiol. 2011;58(21):2190–5.
Rudolph V, Huntgeburth M, von Bardeleben RS, Boekstegers P, Lubos E, Schillinger W, et al. Clinical outcome of critically ill, not fully recompensated, patients undergoing MitraClip therapy. Eur J Heart Fail. 2014;16(11):1223–9.
Taramasso M, Maisano F, Denti P, Latib A, La Canna G, Colombo A, et al. Percutaneous edge-to-edge repair in high-risk and elderly patients with degenerative mitral regurgitation: midterm outcomes in a single-center experience. J Thorac Cardiovasc Surg. 2014;148(6):2743–50.
Terhoeven V, Nikendei C, Cranz A, Weisbrod M, Geis N, Raake PW, et al. Effects of MitraClip on cognitive and psychological function in heart failure patients: the sicker the better. Eur J Med Res. 2019;24(1):14.
Ussia GP, Cammalleri V, Sarkar K, Scandura S, Immè S, Pistritto AM, et al. Quality of life following percutaneous mitral valve repair with the MitraClip System. Int J Cardiol. 2012;155(2):194–200.
Van den Branden BJ, Swaans MJ, Post MC, Rensing BJ, Eefting FD, Jaarsma W, et al. Percutaneous edge-to-edge mitral valve repair in high-surgical-risk patients: do we hit the target? JACC Cardiovasc Interv. 2012;5(1):105–11.
Whitlow PL, Feldman T, Pedersen WR, Lim DS, Kipperman R, Smalling R, et al. Acute and 12-month results with catheter-based mitral valve leaflet repair: the EVEREST II (Endovascular Valve Edge-to-Edge Repair) High Risk Study. J Am Coll Cardiol. 2012;59(2):130–9.
Messika-Zeitoun D, Nickenig G, Latib A, Kuck K-H, Baldus S, Schueler R, et al. Transcatheter mitral valve repair for functional mitral regurgitation using the Cardioband system: 1 year outcomes. Eur Heart J. 2019;40(5):466–72.
Nickenig G, Hammerstingl C, Schueler R, Topilsky Y, Grayburn PA, Vahanian A, et al. Transcatheter mitral annuloplasty in chronic functional mitral regurgitation: 6-month results with the Cardioband percutaneous mitral repair system. JACC Cardiovasc Interv. 2016;9(19):2039–47.
Schofer J, Siminiak T, Haude M, Herrman JP, Vainer J, Wu JC, et al. Percutaneous mitral annuloplasty for functional mitral regurgitation: results of the CARILLON Mitral Annuloplasty Device European Union Study. Circulation. 2009;120(4):326–33.
Siminiak T, Wu JC, Haude M, Hoppe UC, Sadowski J, Lipiecki J, et al. Treatment of functional mitral regurgitation by percutaneous annuloplasty: results of the TITAN Trial. Eur J Heart Fail. 2012;14(8):931–8.
Wołoszyn M, Jerzykowska O, Kałmucki P, Link R, Firek L, Kuzemczak M, et al. Functional assessment of patients after percutaneous mitral valvuloplasty with Carillon™ device: a preliminary report. Kardiol Pol. 2011;69(3):228–33.
Arnold SV, Li Z, Vemulapalli S, Baron SJ, Mack MJ, Kosinski AS, et al. Association of transcatheter mitral valve repair with quality of life outcomes at 30 days and 1 year: analysis of the transcatheter valve therapy registry. JAMA Cardiol. 2018;3(12):1151–9.
Lim DS, Kar S, Spargias K, Kipperman RM, O’Neill WW, Ng MK, et al. Transcatheter valve repair for patients with mitral regurgitation: 30-day results of the CLASP study. JACC Cardiovasc Interv. 2019;12(14):1369–78.
MacHaalany J, Bilodeau L, Hoffmann R, Sack S, Sievert H, Kautzner J, et al. Treatment of functional mitral valve regurgitation with the permanent percutaneous transvenous mitral annuloplasty system: results of the multicenter international Percutaneous Transvenous Mitral Annuloplasty System to Reduce Mitral Valve Regurgitation in Patients with Heart Failure trial. Am Heart J. 2013;165(5):761–9.
Sorajja P, Moat N, Badhwar V, Walters D, Paone G, Bethea B, et al. Initial feasibility study of a new transcatheter mitral prosthesis: the first 100 patients. J Am Coll Cardiol. 2019;73(11):1250–60.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005–11.
Taramasso M, Cioni M, Giacomini A, Michev I, Godino C, Montorfano M, et al. Emerging approaches of transcatheter valve repair/insertion. Cardiol Res Pract. 2010;2010:540749.
Preston-Maher GL, Torii R, Burriesci G. A technical review of minimally invasive mitral valve replacements. Cardiovasc Eng Technol. 2015;6(2):174–84.
Jarral OA, Kidher E, Patel VM, Nguyen B, Pepper J, Athanasiou T. Quality of life after intervention on the thoracic aorta. Eur J Cardiothorac Surg. 2016;49(2):369–89.
Tan MKH, Wong JKL, Bakrania K, Abdullahi Y, Harling L, Casula R, et al. Can activity monitors predict outcomes in patients with heart failure? A systematic review. Eur Heart J. 2019;5(1):11–21.
Bergler-Klein J, Gyöngyösi M, Maurer G. The role of biomarkers in valvular heart disease: focus on natriuretic peptides. Can J Cardiol. 2014;30(9):1027–34.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tan, M.K.H., Jarral, O.A. (2022). Transcatheter Mitral Valve Procedures. In: Athanasiou, T., Darzi, A., Oo, A.Y. (eds) Patient Reported Outcomes and Quality of Life in Cardiovascular Interventions. Springer, Cham. https://doi.org/10.1007/978-3-031-09815-4_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-09815-4_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-09814-7
Online ISBN: 978-3-031-09815-4
eBook Packages: MedicineMedicine (R0)