Abstract
Implantable cardioverter-defibrillator (ICD) has shown to reduce sudden cardiac death and overall mortality in patients with dilated cardiomyopathy. The recently published DANISH trial has shown conflicting outcomes on the long-term survival in patients with prophylactic implantation of ICD in Non-Ischemic Cardiomyopathy (NICM). Two independent reviewers searched MEDLINE, PUBMED, Ovid, CINAHL, clinicaltrials.gov, and Cochrane Registry for randomized control trials (RCT’s) comparing ICD to medical treatment (MT). Six RCT’s enrolling 3389 patients (ICD = 1554 and MT = 1835) were included for final analysis. The primary outcomes were mortality comparing ICD to MT, 231 vs 337 (OR = 0.74, CI = 0.62–0.90, p = 0.002, and I2 = 0%) favoring ICD. On comparing to amiodarone only, there were 47 deaths in the ICD arm vs 71 deaths in amiodarone arm, (OR = 0.66, CI = 0.44–0.98, p = 0.04, I2 0%), to placebo and usual care only (excluding amiodarone); there were 225 deaths in ICD patients compared to 266 in the placebo and usual care arm, (OR = 0.73, CI = 0.59–0.92, p = 0.007, I2 = 15%). The results of our analysis from these six RCTs clearly support the ongoing benefit of prophylactic ICD implantation and support current recommendations for ICD implantation in NICM patients. More RCT’s at a larger scale are needed to further elucidate benefits of both ICD and CRT-D in this post PARADIGM era where MT is at a pinnacle in reducing morbidity and mortality in heart failure patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to 2016 statistical updates published by the American Heart Association, there were roughly 5.7 million Americans older than 20 years of age who had heart failure in 2012, and this may be expected to rise to 46% by 2030 [1]. The prevalence of heart failure increases sharply with age [2, 3]. Almost 50% of patients diagnosed with heart failure die within five years of diagnosis [1, 4]. Historically, the two major causes of death in patients with heart failure are sudden cardiac death (SCD) and progressive pump failure [5, 6]. Nonsustained ventricular tachycardia and other malignant arrhythmias, which include sustained ventricular tachycardia and ventricular fibrillation, are not uncommon in patients with heart failure and cardiomyopathy. Presence of heart failure significantly increases overall mortality and SCD by five-fold, as shown by 38 years follow-up of patients in the Framingham Heart Study [7].
Mortality decline in heart failure patients is evident in this day, and age has been credited to evidence-based management to modify heart failure risk factors and the use of angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB), beta blockers, coronary revascularization, implantable cardioverter-defibrillators (ICDs), and cardiac resynchronization therapy (CRT) [8]. Primary prevention from SCD due to malignant arrhythmias is well established both in ischemic cardiomyopathy (ICM) and nonischemic cardiomyopathy (NICM) with the use of ICDs [9,10,11,12].
NICM accounts for 30–40% of heart failure patients, and SCD accounts for approximately 30% of deaths in this patient population [13]. NICM has several etiologies, and treatment varies significantly depending on its cause, as does disease progression in particular subgroups [14]. Patients with NICM are at high risk for malignant arrhythmias from VT and VF which are the cause of almost 80% of SCD in NICM [15]. The recently published DANISH trail by Kober et al. suggested that the rate of SCD was lowered by 50% with ICD therapy compared with those who received usual care [16]. It is imperative to identify the true value of the ICD in this specific patient populations with NICM that can achieve the supreme benefit from ICD implantation by reducing SCD and improving long-term survival, especially considering the fact that total survival rates for out-of-hospital sudden cardiac arrest episodes are less than 5% in most industrialized countries [15].
Lately, multiple meta-analyses have been published in attempt to answer a similar question raised by the DANISH study, which showed no benefit on all-cause mortality in patients with NICM, Table 1 [17,18,19,20,21]. Most recently published meta-analyses by Al-Khatib et al. [21] used only four studies while excluding the studies which compared ICD to antiarrhythmic therapy including amiodarone. They also excluded studies which used CRT-D in their analysis. We made our analysis more vigorous as we included those studies which used antiarrhythmic therapy including amiodarone and also used CRT-D and analyzed results from available trials to seek an answer to the factual benefits of ICD implantation compared to the medical treatment (MT = amiodarone + placebo + usual care) or individually to amiodarone or (placebo + usual care). We used amiodarone in our analysis as the most common cause of SCD is arrhythmias. Our outcomes focused on all-cause mortality, cardiovascular mortality, and SCD. Our study is more robust as we analyzed the benefits of ICD alone and CRT defibrillator (CRT-D) alone vs medical treatment (MT) on SCD or long-term survival.
Method
Search strategy
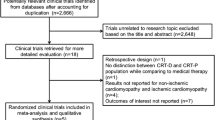
Systematic review was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, Fig. 1 [22].
Data sources
We conducted a broad systematic review of MEDLINE using PUBMED and Ovid, the Cochrane Library Registry, and CINAHL databases from their beginning through March 01, 2017, as well as clinicaltrials.gov for the last 5 years. We used Medical Subject Headings (MeSH) and keyword terms which included ICD*, Implantable Cardioverter Defibrillator, CRT*, Cardiac Resynchronization Therapy, Heart Failure, and Cardiomyopath*. We searched only for clinical trials which were in the English language. Our search was not limited to any specific geographical location, the New York Heart Association class of symptoms, or ventricular ejection fraction. We used Boolean operator “OR” and “AND” to combine search terms. The following search strategy was used (ICD* OR “Implantable Cardioverter Defibrillator”) AND (CRT* OR “Cardiac Resynchronization Therapy”) AND (“Heart failure” OR cardiomyopath*). All studies were added to the endnote, and duplicated studies were removed. An additional search was done through the references of the Agency for Healthcare Research and Quality for implantable defibrillator guide for primary prevention of sudden cardiac death [23].
Study selection protocol
Studies which met our following inclusion criteria were eligible to be included. (1) Prospective RCTs (2) comparing ICD or CRT-D implantation to usual care or amiodarone for the primary prevention of SCD in NICM (3) adult patients (age ≥ 18 years). We excluded those studies which were either nonrandomized or did not compare the ICD or CRT-D in the NICM population alone.
Data extraction quality assessment
Two independent reviewers (W.J.S. and M.R.) did the literature search and selected the studies. Data were extracted by four extractors (W.J.S., M.R., M.H.T., and V.M.) using the pre-defined data fields which were used in individual studies. W.J.S. cross-checked all the data to ensure that the data was entered correctly. Using the MeSH terms and keywords, a total of 537 studies were identified. After excluding duplications, 511 articles were recognized out of which, 501 were excluded. Ten clinical trials were identified which compared ICD or CRT-D to usual care or amiodarone for the primary prevention of SCD in NICM, and their full texts were reviewed. Four studies were excluded because they were nonrandomized trials. For the final analysis, six prospective RCT’s were included for meta-analysis as shown in PRISMA study flow diagram (Fig. 1).
The primary endpoint was (1) reduction in all-cause mortality after implantation of ICD or CRT-D compared to MT (placebo, usual care, or amiodarone), (2) cumulative mortality comparing amiodarone only to ICD and CRT-D, and (3) cumulative mortality comparing placebo and usual care to ICD and CRT-D. Secondary outcomes analyzed were (1) cumulative mortality in ICD group only compared to MT, (2) cumulative mortality in the CRT-D only compared to MT, (3) all-cause cardiovascular mortality comparing ICD and CRT-D to MT, and (4) effect on SCD of ICD and CRT-D vs. MT. We used odds ratios to calculate mortality.
Data synthesis and analysis
Statistical method
We used RevMan Version 5.3 Copenhagen to analyze our data and perform the meta-analysis. Random effect model was used for the analysis considering that most of the studies were performed at the beginning of the millennium, and one was performed within the last decade. Studies that we included in our analysis are the DANISH Study by Kober et al. [16], SCD-HeFT study by Bardy et al. [24], DEFINITE trial by Kadish et al. [25], COMPANION trial by Bristow et al. [26], AMIOVIRT by Strickberger et al. [27], and the CAT trial by Bänsch et al. [28]. Their baseline characteristics and salient features are summarized in Tables 2 and 3. Quality assessment of individual studies using the Cochrane risk of bias is summarized in Table 4.
Analysis of heterogeneity
We calculated the percentage of variability that was present inter-study (between studies) and intra-study (within each study) by using I2 statistics. We calculated trial heterogeneity with RevMan Version 5.3 Copenhagen. I2 value of > 50% was considered to be substantial as it is explained in the Cochrane Handbook for Systematic Reviews for Interventions, (Version 5.1.0, Part 2: General Methods for Cochrane Reviews) [29]. Sensitivity analysis was performed on outcomes where substantial heterogeneity was present.
Funding and affiliation
There was no funding for this study, and there is no affiliation with any industry.
Results and outcomes
A total of six randomized clinical trials were identified, and only patients with NICM were included in our analysis. A total of 3674 patients with NICM were recognized. In the COMPANION trial [26], 285 patients with NICM were randomized to receive CRT pacing only without a defibrillator, which we excluded from our analysis. Patients who received either ICD, CRT-D, or the MT were included in our final analysis, (n = 3389).
Mean age was 60 years with 72% males. Mean EF was 23.3%. The SCD-HeFT trial [24] compared amiodarone to ICD and placebo to ICD, and we included both the groups in our analysis. There were a total of 1554 patients in the ICD or CRT-D arm and 1835 in the medical management arm.
Primary outcomes
On comparing ICD and CRT-D to MT, there were a total of 231 deaths in the ICD and CRT-D group compared to 337 in the medical management group (OR = 0.74, CI = 0.62–0.90, p = 0.002, and I2 = 0%) (Fig. 2a). When comparing ICD and CRT-D to amiodarone only (excluding placebo and usual care), there were a total of 47 deaths in the ICD and CRT-D arm vs 71 deaths in amiodarone arm, (OR = 0.66, CI = 0.44–0.98, p = 0.04, I2 0%) (Fig. 2b). When comparing ICD and CRT-D to placebo and usual care only (excluding amiodarone), 225 deaths were seen in ICD and CRT-D arm compared to 266 in the placebo and usual care arm, (OR = 0.73, CI = 0.59–0.92, p = 0.007, I2 = 15%) (Fig. 2c).
Secondary outcomes
On individual analysis of ICD alone against MT, there were a total of 146 deaths in the ICD arm vs 249 in the MT arm, (OR = 0.74, CI = 0.58–0.93, p = 0.01, I2 = 0%) (Fig. 3a). On similar individual analysis of CRT-D compared to MT, there were a total of 85 deaths in the CRT-D arm compared to 88 deaths in the MT arm, (OR = 0.67, CI = 0.33–1.37, p = 0.27, and I2 = 74%) (Fig. 3b;a). When we analyzed mortality due to cardiovascular causes, there were 93 deaths in the ICD and CRT-D group compared to 126 in the MT, (OR = 0.69, CI = 0.48–0.99, p = 0.04, and I2 = 13%) (Fig. 3c). ICD and CRT-D when compared to MT for SCD revealed 28 deaths vs 62 deaths, (OR = 0.45, CI = 0.28–0.71, p = 0.0006, and I2 = 0%) (Fig. 3d).
a Cumulative all-cause mortality, ICD only vs medical management (usual care + placebo + amiodarone). b Cumulative all-cause mortality CRT-D only vs medical management (usual care + placebo + amiodarone). c Cumulative cardiovascular cause of mortality, ICD and CRT-D vs medical management (usual care + placebo + amiodarone). d Cumulative sudden cardiac death ICD and CRT-D vs medical management (usual care, placebo and amiodarone)
Discussion
ICD implantation has been a revolutionary advancement in the treatment of heart failure with reduced ejection fraction secondary to both ICM and NICM in the past decade [30]. Current guidelines recommend the use of the ICD as a primary preventive strategy for the sudden cardiac death [31,32,33]. These guidelines are supported by the meta-analysis that was published by Desai et al. that showed a significant reduction in mortality in patients with NICM receiving an ICD [34]. The recently published DANISH trial raised questions about the value of ICD implantation on all-cause mortality in NICM by suggesting that there was no difference in the long run in reducing deaths when comparing ICD implantation to medical management [16]. In our analysis, we have attempted to dissect the effects of ICD and CRT-D combined and individually against MT and also individually to amiodarone only and placebo or usual care. We also analyzed the effect of ICD and CRT-D on cardiovascular and SCD mortality.
The primary outcomes herein analyzed were the effect of combined ICD and CRT-D implantation against MT, and these revealed a significant reduction in mortality. Most previous trials to date have shown similar results. When we compared the combined effect of ICD and CRT-D against amiodarone, device implantation was found to be superior in reducing mortality. When ICD and CRT-D were compared with usual care or placebo, a statistically significant reduction in mortality was noted in the defibrillator group. This again strongly supports that ICD and CRT-D are superior to medical management in reducing all-cause mortality in NICM.
Secondary outcomes analyzed included the individual effect of ICD on mortality when compared to MT; we again observed a significant reduction in mortality favoring ICD implantation. On comparing CRT-D only with MT, no significant difference in the mortality was noted (Fig. 3b), but there were only two studies [16, 26] which had reported these data. There was also substantial heterogeneity with the I2 statistic of 74%.
Other secondary outcomes studied include mortality due to all cardiovascular causes in the ICD and CRT-D implantation group compared to MT. This also revealed a significant reduction in mortality due to cardiovascular causes favoring ICD and CRT-D. On comparing the effect of ICD and CRT-D implantation on SCD against MT, these again showed a significant reduction in the number of deaths, supporting the use of ICD and CRT-D for prophylactic implantation.
The results of our analysis are robust at a granular level from these six randomized trials clearly support the ongoing benefit of prophylactic ICD implantation in NICM. The only question raised is the benefit of prophylactic implantation of CRT-D in patients with NICM. Our results cannot be generalized because of the existence of significant heterogeneity that was present when CRT-D alone was compared to MT.
Conclusion
Considering today’s aging population, advancements in medical treatment through the use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta blockers, aldosterone antagonists, and now also neprilysin inhibitors have medically assisted the reduction in morbidity and mortality in this specific patient population. Our data and analyses support current guidelines, which recommend the use of an ICD for primary prevention in patients with NICM. More RCT’s at a larger scale would be required to elucidate further the benefits of both ICD and CRT-D in this post PARADIGM era, where medical treatment is at a pinnacle in reducing mortality in patients with heart failure.
Abbreviations
- ICD:
-
Implantable cardioverter-defibrillator
- CRT:
-
Cardiac resynchronization therapy
- CRT-D:
-
Cardiac resynchronization therapy-defibrillator
- NICM:
-
Nonischemic cardiomyopathy
- MT:
-
Medical treatment
- ICM:
-
Ischemic cardiomyopathy
- RCT:
-
Randomized control trial
- MACE:
-
Major adverse cardiovascular events
- MeSH:
-
Medical subject headings
References
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, Moy CS 3rd, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB (2016) Heart Disease and Stroke Statistics-2016 update: a report from the American Heart Association. Circulation 133(4):e38–360. https://doi.org/10.1161/cir.0000000000000350
Ho KK, Pinsky JL, Kannel WB, Levy D (1993) The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 22(4 Suppl A):6a–13a. https://doi.org/10.1016/0735-1097(93)90455-A
Bleumink GS, Knetsch AM, Sturkenboom MC, Straus SM, Hofman A, Deckers JW, Witteman JC, Stricker BH (2004) Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure: The Rotterdam Study. Eur Heart J 25(18):1614–1619. https://doi.org/10.1016/j.ehj.2004.06.038
Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ (2004) Trends in heart failure incidence and survival in a community-based population. JAMA 292(3):344–350. https://doi.org/10.1001/jama.292.3.344
The CONSENSUS Trial Study Group (1987) Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 316(23):1429–1435. https://doi.org/10.1056/nejm198706043162301
The SOLVD Investigators (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 325(5):293–302. https://doi.org/10.1056/nejm199108013250501
Kannel WB, Wilson PW, D'Agostino RB, Cobb J (1998) Sudden coronary death in women. Am Heart J 136(2):205–212. https://doi.org/10.1053/hj.1998.v136.90226
Merlo M, Pivetta A, Pinamonti B, Stolfo D, Zecchin M, Barbati G, Di Lenarda A, Sinagra G (2014) Long-term prognostic impact of therapeutic strategies in patients with idiopathic dilated cardiomyopathy: changing mortality over the last 30 years. Eur J Heart Fail 16(3):317–324. https://doi.org/10.1002/ejhf.16
Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO (2008) ACC/AHA/HRS 2008 guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: executive summary. Heart Rhythm 5(6):934–955. https://doi.org/10.1016/j.hrthm.2008.04.015
Hua W, Niu H, Fan X, Ding L, Xu YZ, Wang J, Chen K, Wang F, Zhang S (2012) Preventive effectiveness of implantable cardioverter defibrillator in reducing sudden cardiac death in the Chinese population: a multicenter trial of ICD therapy versus non-ICD therapy. J Cardiovasc Electrophysiol 23(Suppl 1):S5–S9. https://doi.org/10.1111/j.1540-8167.2012.02435.x
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346(12):877–883. https://doi.org/10.1056/NEJMoa013474
Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, Fain E, Gent M, Connolly SJ (2004) Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med 351(24):2481–2488. https://doi.org/10.1056/NEJMoa041489
Pimentel M, Rohde LE, Zimerman A, Zimerman LI (2016) Sudden cardiac death markers in non-ischemic cardiomyopathy. J Electrocardiol 49(3):446–451. https://doi.org/10.1016/j.jelectrocard.2016.03.012
Shehata ML, Turkbey EB, Vogel-Claussen J, Bluemke DA (2008) Role of cardiac magnetic resonance imaging in assessment of nonischemic cardiomyopathies. Topics in magnetic resonance imaging: TMRI 19(1):43–57. https://doi.org/10.1097/RMR.0b013e31816fcb22
Albouaini K, Mudawi T, Pyatt JR, Wright DJ (2009) Implantable cardioverter defibrillator: what a hospital practitioner needs to know. Eur J Intern Med 20(6):591–597. https://doi.org/10.1016/j.ejim.2009.06.006
Kober L, Thune JJ, Nielsen JC, Haarbo J, Videbaek L, Korup E, Jensen G, Hildebrandt P, Steffensen FH, Bruun NE, Eiskjaer H, Brandes A, Thogersen AM, Gustafsson F, Egstrup K, Videbaek R, Hassager C, Svendsen JH, Hofsten DE, Torp-Pedersen C, Pehrson S (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375(13):1221–1230. https://doi.org/10.1056/NEJMoa1608029
Wolff G, Lin Y, Karathanos A, Brockmeyer M, Wolters S, Nowak B, Furnkranz A, Makimoto H, Kelm M, Schulze V (2017) Implantable cardioverter/defibrillators for primary prevention in dilated cardiomyopathy post-DANISH: an updated meta-analysis and systematic review of randomized controlled trials. Clin Res Cardiol : Off J German Card Soc 106(7):501–513. https://doi.org/10.1007/s00392-017-1079-0
Stavrakis S, Asad Z, Reynolds D (2017) Implantable cardioverter defibrillators for primary prevention of mortality in patients with non-ischemic cardiomyopathy: a meta-analysis of randomized controlled trials. J Cardiovasc Electrophysiol 28(6):659–665. https://doi.org/10.1111/jce.13204
Shun-Shin MJ, Zheng SL, Cole GD, Howard JP, Whinnett ZI, Francis DP (2017) Implantable cardioverter defibrillators for primary prevention of death in left ventricular dysfunction with and without ischaemic heart disease: a meta-analysis of 8567 patients in the 11 trials. Eur Heart J 38(22):1738–1746. https://doi.org/10.1093/eurheartj/ehx028
Luni FK, Singh H, Khan AR, Malik SA, Khawaja O, Riaz H, Lee W, Kabour A, Richards M, Aasbo J (2017) Mortality effect of ICD in primary prevention of nonischemic cardiomyopathy: a meta-analysis of randomized controlled trials. J Cardiovasc Electrophysiol 28(5):538–543. https://doi.org/10.1111/jce.13192
Al-Khatib SM, Fonarow GC, Joglar JA, Inoue LYT, Mark DB, Lee KL, Kadish A, Bardy G, Sanders GD (2017) Primary prevention implantable cardioverter defibrillators in patients with nonischemic cardiomyopathy: a meta-analysis. JAMA cardiology 2(6):685–688. https://doi.org/10.1001/jamacardio.2017.0630
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed) 339(jul21 1):b2700. https://doi.org/10.1136/bmj.b2700
Uhlig K, Balk EM, Earley A, Persson R, Garlitski AC, Chen M, Lamont JL, Miligkos M, Avendano EE (2013) AHRQ technology assessments. In: Assessment on implantable defibrillators and the evidence for primary prevention of sudden cardiac death. Agency for Healthcare Research and Quality (US), Rockville (MD)
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352(3):225–237. https://doi.org/10.1056/NEJMoa043399
Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JH (2004) Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 350(21):2151–2158. https://doi.org/10.1056/NEJMoa033088
Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM (2004) Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 350(21):2140–2150. https://doi.org/10.1056/NEJMoa032423
Strickberger SA, Hummel JD, Bartlett TG, Frumin HI, Schuger CD, Beau SL, Bitar C, Morady F (2003) Amiodarone versus implantable cardioverter-defibrillator: randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic nonsustained ventricular tachycardia—AMIOVIRT. J Am Coll Cardiol 41(10):1707–1712. https://doi.org/10.1016/S0735-1097(03)00297-3
Bansch D, Antz M, Boczor S, Volkmer M, Tebbenjohanns J, Seidl K, Block M, Gietzen F, Berger J, Kuck KH (2002) Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: the Cardiomyopathy Trial (CAT). Circulation 105(12):1453–1458. https://doi.org/10.1161/01.CIR.0000012350.99718.AD
Higgins JPT GS (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0
Taylor AL, Ziesche S, Yancy C, Carson P, D'Agostino R Jr, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN (2004) Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 351(20):2049–2057. https://doi.org/10.1056/NEJMoa042934
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Revista espanola de cardiologia (English ed) 69(12):1167. https://doi.org/10.1016/j.rec.2016.11.005
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL (2013) 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128(16):1810–1852. https://doi.org/10.1161/CIR.0b013e31829e8807
Desai AS, Fang JC, Maisel WH, Baughman KL (2004) Implantable defibrillators for the prevention of mortality in patients with nonischemic cardiomyopathy: a meta-analysis of randomized controlled trials. JAMA 292(23):2874–2879. https://doi.org/10.1001/jama.292.23.2874
Acknowledgements
Muhammad Hassan Tahir (M.H.T.) and Varun Mairyala (V.M.) helped to extract the data from the papers and enter into the pre-specified data sheets.
Author information
Authors and Affiliations
Contributions
Waqas Javed Siddiqui: concept/design, data collection, data analysis and interpretation, drafting, critical revision, statistics
Sandeep Aggarwal: concept/design, data analysis and interpretation, critical revision
Muhammad Rafique: data collection, drafting
Swaiman Singh: drafting
Steven Kutalek: critical revision, approval of article
Howard J Eisen: critical revision, approval of article
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The manuscript does not contain clinical studies or patient data.
Rights and permissions
About this article
Cite this article
Siddiqui, W.J., Aggarwal, S., Rafique, M. et al. Prophylactic use of the implantable cardioverter-defibrillator and its effect on the long-term survival, cardiovascular and sudden cardiac death in nonischemic cardiomyopathy patients—a systematic review and meta-analysis. Heart Fail Rev 23, 181–190 (2018). https://doi.org/10.1007/s10741-018-9671-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-018-9671-6