Abstract
Introduction
Cardiac arrest is the major cause of sudden death in developed countries. Extracorporeal cardiopulmonary resuscitation (ECPR) employs extracorporeal membrane oxygenation (ECMO) in patients without return of spontaneous circulation (ROSC) by conventional cardiopulmonary resuscitation (CPR). Aim of the current study was to assess short- and long-term outcome in patients treated with ECPR in our tertiary center and to identify predictors of outcome.
Methods
We retrospectively collected data of all patients treated with ECPR at our institution from 2002 to 2013. Outcome was assessed according to patient records; good neurological outcome was defined as cerebral performance category 1 or 2. Quality of life data was collected using EQ-5 questionnaire. Uni- and multivariate analysis was applied to identify predictors of outcome.
Results
One-hundred and seventeen patients were included into the study. Weaning from ECMO was successful in 61 (52 %) patients. Thirty-day survival endpoint was achieved by 27 (23 %) patients. Good neurological outcome was present in 17 (15 %) patients. Multivariate analysis revealed baseline serum lactate as the strongest predictor of outcome, whereas age and out-of-hospital CPR did not predict outcome. The optimal lactate cut-off to discriminate outcome was determined at 4.6 mmol/l [HR 3.55 (2.29–5.49), p < 0.001, log-rank test].
Conclusion
ECPR represents a treatment option in patients without ROSC after conventional CPR rescuing 15 % of patients with good neurological outcome. Serum lactate may play a crucial role in patient selection for ECPR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac arrest (CA) is the major cause of sudden death in developed countries and outcome is often dismal [38]. Despite cardiopulmonary resuscitation (CPR), only the minority of patients return to their former daily life and lifestyle [8, 19]. Optimization of CPR has been attempted using mechanical chest compression devices. However, several randomized trials ev idenced no survival benefit in comparison to conventional CPR [29]. Extracorporeal CPR (ECPR) employs extracorporeal membrane oxygenation (ECMO) in patients without return of spontaneous circulation (ROSC) by conventional CPR [2, 27, 33]. ECMO provides adequate temporary perfusion and oxygenation to organs in cardiac arrest patients and therefore increases the rate of successful defibrillation, prevents re-arrest due to ischemia-triggered myocardial dysfunction, and—most importantly—enables subsequent coronary interventions without limitation of mechanical CPR in patients without ROSC [6, 21]. Of note, the incidence of acute coronary syndrome (ACS) has been reported to be high in CA patients, and it has been noted that the imminent use of percutaneous coronary intervention (PCI) improves outcome [20, 35].
Kagawa et al. reported data of 86 consecutive patients with rapid-response ECMO in cases with refractory cardiac arrest due to ACS [17]. Of note, in 71 % of the cases intra-arrest PCI was performed and mild hypothermia was induced in 37 % of the patients. Thirty-day mortality was 29 % in this cohort. In addition, Kagawa and coworkers could convincingly show that the intra-arrest PCI success, the time interval from collapse to the initiation of ECMO, and in-hospital cardiac arrest were associated with superior 30-day survival [17]. No data are available regarding the long-term prognosis of these patients.
In clinical use the decision to employ ECPR has to be made quickly. Very limited data are available to select parameters that guide the clinician to decide whether to institute ECMO therapy or not. Furthermore, in the acute situation during CPR only a limited number of variables can be assessed. Therefore, the first aim of the present study was to assess the prognostic value of clinical parameters and laboratory values before ECMO employment. We aimed especially to identify parameters which can be in most cases immediately assessed during CPR and may therefore be useable for decision making under these special circumstances. Secondly, another aim was to investigate the long-term prognosis and quality of life of patients that have been treated with ECPR in our tertiary referral center.
Methods
Study patients
We retrospectively collected data of all patients treated with ECPR at our institution from 2002 to 2013. This included both out-of-hospital (OH) patients and in-hospital (IH) CA patients. The study was approved by the local institutional ethics board (University Hospital Jena). According to local regulations no consent of the patients was needed in this retrospective registry. All patients that provided quality of life data gave written informed consent.
Inclusion criteria for ECPR
When CPR was performed, a quick evaluation was conducted to verify eligibility for ECPR by the cardiologist on duty based on internal standard operation procedures (per telephone if not in-house). The main criterion for ECPR was age between 18 and 74 years; however, also older patients were treated based on individual decisions. The estimated interval between collapse and start of CPR should not have been longer than 20 min and the presumed underlying disease should be of cardiac origin or due to pulmonary embolism. A failure to achieve ROSC within 20 min of conventional CPR by professional medical personnel qualified for ECPR. Malignant comorbidities and an initial pH below 7.0 were defined as exclusion criteria. However, after retrospective analysis of the data, we noticed that also patients with exclusion criteria still underwent ECPR and therefore included them into the data analysis.
Data collection
Data pertaining to CPR, primary rhythm, comorbidities, laboratory values, catecholamine doses, weaning from ECMO including ECMO settings, 30-day survival, and cerebral outcome were collected from medical records and patient charts. In addition, data were obtained whether patients underwent OH-CPR or IH-CPR. Favorable neurological outcome was defined as cerebral performance category (CPC) of 1 (good performance) and 2 (moderate disability) on a 5-point scale at the time of hospital discharge [30].
Follow-up
Patients were contacted to evaluate the current survival status. Patients alive were asked to complete a standardized questionnaire to evaluate the health related quality of life (HRQoL) using the EuroQOL-EQ-5D-5L questionnaire [31]. Briefly, this questionnaire collects information about HRQoL in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each of these dimensions is classified in five levels of severity. In addition, a visual analogue scale allows the patient to grade its HRQoL on a scale between 0 and 100.
ECMO system
The ECMO system comprised a centrifugal pump, membrane oxygenator, heat exchanger, and bypass cannulas, as previously described [11, 16]. Two different systems have been used: Biocal 370 (Medtronic, Minneapolis, MN) and Lifebridge (Zoll Lifebridge, Germany).
ECPR management
Cardiologists and cardiopulmonary technicians, as well as assistance personal were trained to set up and manage the ECMO systems with a delay minimum. In cases of OH-CA, the cardiologist receiving the telephone call from the emergency medical services decided about the indication for ECPR. Ideally, the patient was directly transferred to the catheterization laboratory. If the patient arrived before the personal came in during night or weekend shifts, he was brought under ongoing resuscitation to the emergency department and then transferred to the catheterization laboratory to implement the ECMO system. In case of IH-CA, patients in whom ROSC could not be achieved after 20 min, patients were transferred to the catheterization laboratory for initiation of ECMO. The femoral vein (21F) and artery (19F) were percutaneously cannulated, and ECMO was started. Heparin was also administered (100 IU/kg) immediately after cannulation to maintain an activated clotting time of 160–200 s. Subsequently, coronary angiography was performed including PCI, if necessary. In comatose patients, mild hypothermia was induced according to the discretion of the intensive care specialist and the primary rhythm. ECMO sheaths were removed percutaneously.
Statistical analysis
Since most continuous variables were not normally distributed for reasons of uniformity medians (with first and third quartiles) were used for presentation. Categorical variables are presented as numbers and percentages. The Mann–Whitney U test for continuous variables and Chi square test for dichotomous variables were used as appropriate to identify risk factors associated with 30-day survival and to analyze HRQoL. Two logistic regression models were created, first a model using all relevant factors in our database and a second one using only variables available during CPR (short history, physical examination and laboratory measurements possible in blood gas analysis). Variables with univariable association to 30-day mortality (p < 0.1) were included in the multivariable stepwise regression models. Age and OH-CPR were forced into these models. Statistical analysis was performed with MedCalc for Windows, version 14.12.0 (MedCalc Software, Ostend, Belgium). A p value of <0.05 was considered statistically significant.
Results
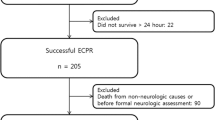
The baseline characteristics of the study population are presented in Table 1. One-hundred and seventeen patients were included into the study. Weaning from ECMO support with restoration of independent circulation was successful in 61 (52 %) of the patients. Thirty-day survival endpoint was achieved by 27 (23 %) of the patients. However, good neurological outcome (CPC 1 or 2) was present in only 17 (15 %) patients.
As depicted in Table 1, 34 patients (29 %) were treated following OH-CA. Thirty-day mortality did not differ between patients treated with OH-CA and IH-CA (82 vs. 68 %; p = 0.26). Survivors and non-survivors differed regarding their serum levels of creatinine, lactate and hemoglobin. There was a trend towards a better survival of older patients. Regarding the comorbidities, patients with previously diagnosed arterial hypertension were more frequent in the survivor group. Comparing the groups with OH-CA and IH-CA distinct differences were evident: The group with IH-CA was older, had a different body composition and more frequently a positive history of diabetes mellitus. The OH-CA group was younger, presented more frequently with ventricular fibrillation and had higher lactate levels.
Patients with or without myocardial infarction as cause of CA had no differences in survival (30-day mortality 78 vs. 76 %; p = 0.91) but patients with CA post-surgery or -intervention had a lower 30-day mortality than other patients (63 vs. 82 %; p = 0.04).
More detailed information about the circumstances of the CPR was available in 66 (56 %) of the patients. The median duration of resuscitation was 30 (IQR 20–60) minutes. When grouping patients according to the median age (61 years), older patients were resuscitated significantly shorter [30 (15;44) min vs. 43 (30;68) min; p = 0.007). Comparing patients according to their survival status, surviving patients were resuscitated significantly shorter [17 (10; 30) min vs. 40 (30;75) min; p < 0.001]. Within the group with IH-CA, 32 patients (38 %) were treated following procedures such as transcutaneous aortic valve implantation (n = 21), surgical coronary artery bypass grafting or surgical valve repair (n = 8), other non-heart surgery (n = 2) or Mitraclip® implantation (n = 1).
ECMO was initiated with a flow of 4.5 (IQR: 3.5;5.0) L/min. The therapy with ECMO was maintained for 26 (IQR: 6;83) h. Initial flow rates did not differ between survivors and non-survivors.
Table 2 shows univariable and multivariable analysis of parameters predicting 30-day mortality. As presented in Table 2 only high serum lactate levels (data available in n = 110 patients) remained in the final model with significant association to 30-day mortality. Since in most of the cases the clinician has limited information available in the acute setting, another model was constructed with variables that are acutely available (Table 3). Here, high serum lactate levels and low hemoglobin levels independently predicted unfavorable outcome.
Since lactate was the strongest predictor of outcome, the optimal cut-off value was calculated using Youden-index in ROC-analysis. Figure 1 presents outcome applying the optimal lactate cut-off of 4.6 mmol/L [hazard ratio 3.55 (2.29–5.49), p < 0.001 by log-rank test] revealing a mortality difference of 88 vs. 44 %.
In addition, in Table 4 different parameters were evaluated regarding their prognostic relevance under ongoing therapy. Different laboratory values including creatinine were evaluated as well as limb complications and the need of the transfusion of blood products. Again, only lactate levels remained significant in the multivariate analysis.
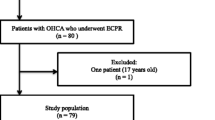
As presented, 27 patients survived the 30-day mortality endpoint. These patients were followed up for a median of 405 days. Two patients (7 %) died within one-year following CPR (Fig. 2). All patients discharged with a good neurological outcome (followed up for a median of 641 days) were alive one year after CPR. Patients with good neurological outcome were resuscitated in three cases as OH (9 % of all OH) and in 14 cases IH (17 % of all IH). Ten patients with good neurological outcome returned the HRQoL questionnaire revealing no or minimal impairment: health assessment was in median 80 % (IQR: 70; 95 %), no impairment in the categories mobility, self-care, daily life, pain and anxiety was detectable (median assessment 4 or 5).
Discussion
The current study provides information about a large cohort of patients in a tertiary center treated with ECMO-assisted CPR regarding short and long-term prognosis. In summary, in patients undergoing CPR with no ROSC after 20 min and therefore a predicted mortality of nearly 100 % use of ECPR resulted in about a quarter of the patients in a positive 30-day outcome. Furthermore, patients surviving the acute phase have excellent prognosis with minimal persisting abnormalities.
So far, limited data are available regarding the treatment of patients with ECMO following CA [13, 16]. As recently summarized [26], the idea of using an extracorporeal pump to support the failing circulation with oxygenated blood dates back to 1937 [7]. After transportable, battery-powered heart–lung machines became available, several pioneers used it for IH-CA, reporting 15 long-term survivors out of 39 patients on emergency bypass in 1976 [25]. The majority of these patients had pulmonary embolism limiting the comparability of these initial report. Looking at newer reports, Avalli et al. reported a case series of 42 patients with IH-CA and OH-CA: Discharged from the intensive care unit were 46 % of IH-CA and 5 % of OH-CA. Since also long-term prognosis was better in patients with IH-CA Avalli and coauthors concluded that patients with witnessed IH-CA benefit more from ECMO treatment compared to those who experienced an OH-CA [1]. This is in line with several recent retrospective case series presenting survival rates of 26–39 % for IH-CA [4, 18, 34]. Expectedly, survival for OH-CA is inferior with a reported rate of 4–39 % [9, 18, 22–24]. However, Chen et al. and Shin et al. convincingly reported in matched cohort propensity analyses, that ECMO-assisted CPR is superior to conventional CPR [3, 34]. Our short-term outcome data, the neurological status as well as the long-term results are at least consistent with these reports. In our patient cohort, there was no difference for better survival and better neurological outcome in patients treated with IH-CA. Distinct differences between the groups were evident: patients following IH-CA were older and had more comorbidities but patients with OH-CA had higher lactate levels indicating that the comparability of these groups is limited. In parallel, also patients post-surgery or post-interventional were characterized by a worse prognosis, most likely to a severely ill cohort mainly following TAVI. At this point it seems relevant that IH-CA patients are much more likely to have witnessed CA with a shorter duration to advanced cardiac life support and a shorter time until start of ECPR and that comorbidities are known to the treating physician implicating a bias in decision for ECMO implantation.
One major aim of the study was to evaluate potential parameters possibly guiding the physician before ECMO institution. Especially parameters that might be immediately present at the time point of decision making regarding ECPR were of special interest including parameters available in the initial blood gas analysis but without knowing the detailed patients’ history. Different values predicted outcome in univariate analysis, however, only serum lactate and hemoglobin remained statistically significant in the final multivariate model. One should expect that older age is a potent predictor of impaired outcome in this setting, too. Surprisingly, there was a trend towards better survival of older patients in our study. To further analyze this, patients were grouped according to the mean age revealing that older patients were significantly shorter resuscitated than younger patients before ECMO institution. This can be explained by a possible selection bias. Although cases that did not receive ECMO support during the study period were not registered, one could speculate that the physician on duty might have declined ECMO support in older patients with long resuscitation time and might have offered ECMO treatment in younger patients with otherwise deleterious circumstances. Since age and the circumstances of IH-CA or OH-CA seem to be crucial predictors of outcome the multivariable analysis was correspondingly adjusted, revealing insignificant values. The limited number of cases precludes a separate analysis of patients with IH-CA and OH-CA which would be otherwise desirable.
In conclusion, hemoglobin levels, and especially serum lactate levels predict outcome of ECMO treatment in patients undergoing CPR. Although these findings are not surprising, this is to the best of our knowledge the first comprehensive analysis of potential predictors. The optimal cut-off value has been calculated to 4.6 mmol/L; however, this needs to be confirmed in future studies. The only available risk prediction model for patients with ECMO following CA has recently been published by Park et al.: In their retrospective study, in multivariate logistic regression, age ≤66 years, shockable arrest rhythm, CPR to ECMO pump-on time ≤38 min, post-ECMO arterial pulse pressure >24 mm Hg, and post-ECMO Sequential Organ Failure Assessment score ≤14 were independent predictors for survival to discharge [28]. There are some distinct differences compared to our study. Park et al. studied more patients but included parameters before and after ECMO institution without including laboratory values. Future studies or multicenter registries are needed to comprehensively assess prognostic parameters before and after decision making of EPCR employment to especially reveal the role of age and duration of CPR as well as other (laboratory) values in relation to short- and long-term prognosis [12, 14, 15]. We also provide data regarding laboratory and other parameters after ECPR implementation. Of note, the only predictor in multivariate analysis is serum lactate, again underlining the striking potential of this parameter as indicator of tissue perfusion.
Another aim of the study was to assess long-term prognosis of these patients. In the setting of CPR, mortality rates are high. However, patients surviving the critical phase of the intensive care unit stay and the first month following resuscitation have excellent prognosis. Patients were also asked to return a HRQoL questionnaire. Although predominantly satisfied patients return such documents, it is important to note that 9 % of the overall cohort in patients without ROSC during the first 20 min presented with good quality of life in long-term follow-up. To date, this is the first assessment of quality of life in such a cohort. These data are in line with a study by Johnson et al. reporting good neurological outcome of 75 % (n = 3) of patients that survived discharge after 6 months [10, 37].
The field of CPR-assisted with more invasive strategies is currently investigated regarding different aspects, including ECMO, hypothermia, mechanical CPR with chest compression systems and also early reperfusion in the catheterization laboratory. Of note, Stub and coworkers presented the CHEER-trial (mechanical CPR, Hypothermia, ECMO and Early Reperfusion) showing feasibility of such an invasive protocol in a single center with high survival rates (54 %) [36]. Also the SAVE-J study published by Sakamoto et al. revealed an improved neurological outcome in patients with OH-CA with shockable rhythm treated by a treatment bundle including ECPR, therapeutic hypothermia and intra-aortic balloon counterpulsation [32]. Müller and Lubnow recently summarized [26] that mortality for patients under CPR may be decreased if all facets of patient care are taken into account from the onset of collapse until weaning from ECMO: first, automatic mechanical chest compression device for transport to the hospital; second, implementation of effective intra-arrest hypothermia with a core temperature of 32.3 °C at ECMO initiation; third, avoiding hyperoxia and; fourth, early PCI to treat cardiac ischemia. The feasibility of such a protocol has been demonstrated by Fagnoul [5], however, larger studies implementing such strategies are warranted.
Our study has several strengths and limitations. First, we present data of a comparably large cohort with long-term data but with retrospective data collection. However, some data regarding CPR circumstances such as CPR duration and exact etiology of CA are incomplete. Second, our database reflects daily routine in an experienced tertiary center, but we did not register patients who did not receive ECMO therapy. Third, although there were clear in- and exclusion criteria regarding patient selection, these criteria were ignored in several patients on an individual basis. Fourth, due to the design as a registry, data collection following ECMO initiation was too heterogeneous to allow analysis of these parameters. Future studies and registries need to answer this question.
Conclusions
In conclusion, ECPR represents a treatment option in patients without ROSC after conventional CPR rescuing 15 % of patients with good neurological outcome. Multivariate analysis revealed serum lactate as potent predictor of outcome. Future (randomized) studies need to determine the role of ECPR in different settings and multicenter registries need to explore long-term prognosis and risk prediction possibilities.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CA:
-
Cardiac arrest
- CPC:
-
Cerebral performance category
- CPR:
-
Cardiopulmonary resuscitation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- ECMO:
-
Extracorporeal membrane oxygenation
- HRQoL:
-
Health related quality of life
- IH:
-
In-hospital (cardiac arrest)
- OH:
-
Out-of-hospital (cardiac arrest)
- PCI:
-
Percutaneous coronary intervention
- ROSC:
-
Return of spontaneous circulation conventional
References
Avalli L, Maggioni E, Formica F, Redaelli G, Migliari M, Scanziani M, Celotti S, Coppo A, Caruso R, Ristagno G, Fumagalli R (2012) Favourable survival of in-hospital compared to out-of-hospital refractory cardiac arrest patients treated with extracorporeal membrane oxygenation: an Italian tertiary care centre experience. Resuscitation 83:579–583. doi:10.1016/j.resuscitation.2011.10.013
Chen B, Chang YM (2008) CPR with assisted extracorporeal life support. Lancet 372:1879. doi:10.1016/S0140-6736(08)61805-X (author reply 1879-1880)
Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, Chen WJ, Huang SC, Chi NH, Wang CH, Chen LC, Tsai PR, Wang SS, Hwang JJ, Lin FY (2008) Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 372:554–561. doi:10.1016/S0140-6736(08)60958-7
Chen YS, Yu HY, Huang SC, Lin JW, Chi NH, Wang CH, Wang SS, Lin FY, Ko WJ (2008) Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med 36:2529–2535. doi:10.1097/CCM.0b013e318183f491
Fagnoul D, Taccone FS, Belhaj A, Rondelet B, Argacha JF, Vincent JL, Backer DD (2013) Extracorporeal life support associated with hypothermia and normoxemia in refractory cardiac arrest. Resuscitation 84:1519–1524. doi:10.1016/j.resuscitation.2013.06.016
Ferrari M, Kruzliak P, Spiliopoulos K (2015) An insight into short- and long-term mechanical circulatory support systems. Clin Res Cardiol 104:95–111. doi:10.1007/s00392-014-0771-6
Gibbon J (1937) Artificial maintenance of life during experimental occlusion of the pulmonary artery. Arch Surg 34:1105–1131
Group S-Ks (2007) Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet 369:920–926. doi:10.1016/S0140-6736(07)60451-6
Haneya A, Philipp A, Diez C, Schopka S, Bein T, Zimmermann M, Lubnow M, Luchner A, Agha A, Hilker M, Hirt S, Schmid C, Muller T (2012) A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation 83:1331–1337. doi:10.1016/j.resuscitation.2012.07.009
Johnson NJ, Acker M, Hsu CH, Desai N, Vallabhajosyula P, Lazar S, Horak J, Wald J, McCarthy F, Rame E, Gray K, Perman SM, Becker L, Cowie D, Grossestreuer A, Smith T, Gaieski DF (2014) Extracorporeal life support as rescue strategy for out-of-hospital and emergency department cardiac arrest. Resuscitation 85:1527–1532. doi:10.1016/j.resuscitation.2014.08.028
Jung C, Ferrari M, Gradinger R, Fritzenwanger M, Pfeifer R, Schlosser M, Poerner TC, Brehm BR, Figulla HR (2008) Evaluation of the microcirculation during extracorporeal membrane-oxygenation. Clin Hemorheol Microcirc 40:311–314
Jung C, Figulla HR, Ferrari M (2010) High frequency of organ failures during extracorporeal membrane oxygenation: is the microcirculation the answer? Ann Thorac Surg 89:345–346 (author reply 346)
Jung C, Franz M, Figulla HR, Sonntag S, Hug M, Mudra H, Bauerschmitt R, Kleber FX, Feindt P, Mehlhorn U, Vahl C, Bruns HJ, Ferrari M (2015) Percutaneous extracorporeal life support in patients with circulatory failure: results of the German Lifebridge Registry. J Invasive Cardiol 27:93–97
Jung C, Fuernau G, de Waha S, Eitel I, Desch S, Schuler G, Figulla HR, Thiele H (2015) Intraaortic balloon counterpulsation and microcirculation in cardiogenic shock complicating myocardial infarction: an IABP-SHOCK II substudy. Clin Res Cardiol. doi:10.1007/s00392-015-0833-4
Jung C, Fuernau G, Muench P, Desch S, Eitel I, Schuler G, Adams V, Figulla HR, Thiele H (2015) Impairment of the endothelial glycocalyx in cardiogenic shock and its prognostic relevance. Shock 43:450–455. doi:10.1097/SHK.0000000000000329
Jung C, Schlosser M, Figulla HR, Ferrari M (2008) Providing macro- and microcirculatory support with the lifebridge system during high-risk PCI in cardiogenic shock. Heart Lung Circ 18:296–298
Kagawa E, Dote K, Kato M, Sasaki S, Nakano Y, Kajikawa M, Higashi A, Itakura K, Sera A, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S (2012) Should we emergently revascularize occluded coronaries for cardiac arrest?: rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation 126:1605–1613. doi:10.1161/CIRCULATIONAHA.111.067538
Kagawa E, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S, Nakama Y, Dai K, Takayuki O, Ikenaga H, Morimoto Y, Ejiri K, Oda N (2010) Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation 81:968–973. doi:10.1016/j.resuscitation.2010.03.037
Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide A, Implementation Working Group for the All-Japan Utstein Registry of the F, Disaster Management A (2010) Nationwide public-access defibrillation in Japan. N Engl J Med 362:994–1004. doi:10.1056/NEJMoa0906644
Knafelj R, Radsel P, Ploj T, Noc M (2007) Primary percutaneous coronary intervention and mild induced hypothermia in comatose survivors of ventricular fibrillation with ST-elevation acute myocardial infarction. Resuscitation 74:227–234. doi:10.1016/j.resuscitation.2007.01.016
Laurent I, Monchi M, Chiche JD, Joly LM, Spaulding C, Bourgeois B, Cariou A, Rozenberg A, Carli P, Weber S, Dhainaut JF (2002) Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol 40:2110–2116
Le Guen M, Nicolas-Robin A, Carreira S, Raux M, Leprince P, Riou B, Langeron O (2011) Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care 15:R29. doi:10.1186/cc9976
Leick J, Liebetrau C, Szardien S, Fischer-Rasokat U, Willmer M, van Linden A, Blumenstein J, Nef H, Rolf A, Arlt M, Walther T, Hamm C, Mollmann H (2013) Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin Res Cardiol 102:661–669. doi:10.1007/s00392-013-0580-3
Maekawa K, Tanno K, Hase M, Mori K, Asai Y (2013) Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med 41:1186–1196. doi:10.1097/CCM.0b013e31827ca4c8
Mattox KL, Beall AC Jr (1976) Resuscitation of the moribund patient using portable cardiopulmonary bypass. Ann Thorac Surg 22:436–442
Muller T, Lubnow M (2013) The future of E-CPR: a joint venture. Resuscitation 84:1463–1464. doi:10.1016/j.resuscitation.2013.08.004
Nagao K, Hayashi N, Kanmatsuse K, Arima K, Ohtsuki J, Kikushima K, Watanabe I (2000) Cardiopulmonary cerebral resuscitation using emergency cardiopulmonary bypass, coronary reperfusion therapy and mild hypothermia in patients with cardiac arrest outside the hospital. J Am Coll Cardiol 36:776–783
Park SB, Yang JH, Park TK, Cho YH, Sung K, Chung CR, Park CM, Jeon K, Song YB, Hahn JY, Choi JH, Choi SH, Gwon HC, Suh GY (2014) Developing a risk prediction model for survival to discharge in cardiac arrest patients who undergo extracorporeal membrane oxygenation. Int J Cardiol 177:1031–1035. doi:10.1016/j.ijcard.2014.09.124
Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, Lamb SE, Slowther AM, Woollard M, Carson A, Smyth M, Whitfield R, Williams A, Pocock H, Black JJ, Wright J, Han K, Gates S, collaborators Pt (2014) Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. doi:10.1016/S0140-6736(14)61886-9
Pfeifer R, Jung C, Purle S, Lauten A, Yilmaz A, Surber R, Ferrari M, Figulla HR (2011) Survival does not improve when therapeutic hypothermia is added to post-cardiac arrest care. Resuscitation 82:1168–1173. doi:10.1016/j.resuscitation.2011.05.024
Rasanen P, Roine E, Sintonen H, Semberg-Konttinen V, Ryynanen OP, Roine R (2006) Use of quality-adjusted life years for the estimation of effectiveness of health care: a systematic literature review. Int J Technol Assess Health Care 22:235–241. doi:10.1017/S0266462306051051
Sakamoto T, Morimura N, Nagao K, Asai Y, Yokota H, Nara S, Hase M, Tahara Y, Atsumi T, Group S-JS (2014) Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation 85:762–768. doi:10.1016/j.resuscitation.2014.01.031
Scholz KH, Figulla HR, Schroder T, Hering JP, Bock H, Ferrari M, Kreuzer H, Hellige G (1995) Pulmonary and left ventricular decompression by artificial pulmonary valve incompetence during percutaneous cardiopulmonary bypass support in cardiac arrest. Circulation 91:2664–2668
Shin TG, Choi JH, Jo IJ, Sim MS, Song HG, Jeong YK, Song YB, Hahn JY, Choi SH, Gwon HC, Jeon ES, Sung K, Kim WS, Lee YT (2011) Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med 39:1–7. doi:10.1097/CCM.0b013e3181feb339
Spaulding CM, Joly LM, Rosenberg A, Monchi M, Weber SN, Dhainaut JF, Carli P (1997) Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med 336:1629–1633. doi:10.1056/NEJM199706053362302
Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, Hockings L, Shaw J, Duffy SJ, Burrell A, Cameron P, Smit DV, Kaye DM (2014) Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. doi:10.1016/j.resuscitation.2014.09.010
Zeymer U, Hochadel M, Hauptmann KE, Wiegand K, Schuhmacher B, Brachmann J, Gitt A, Zahn R (2013) Intra-aortic balloon pump in patients with acute myocardial infarction complicated by cardiogenic shock: results of the ALKK-PCI registry. Clin Res Cardiol 102:223–227. doi:10.1007/s00392-012-0523-4
Zobel C, Dorpinghaus M, Reuter H, Erdmann E (2012) Mortality in a cardiac intensive care unit. Clin Res Cardiol 101:521–524. doi:10.1007/s00392-012-0421-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts to declare.
Rights and permissions
About this article
Cite this article
Jung, C., Janssen, K., Kaluza, M. et al. Outcome predictors in cardiopulmonary resuscitation facilitated by extracorporeal membrane oxygenation. Clin Res Cardiol 105, 196–205 (2016). https://doi.org/10.1007/s00392-015-0906-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0906-4