Abstract
Purpose
Previous studies have shown that the new nutritional and immunological status scoring systems of the Naples prognostic score (NPS), controlling nutritional status score (CONUT), and the older prognostic nutritional index (PNI) are independent predictors in colorectal cancer. This study compares the prognostic value of NPS, CONUT, and PNI in T1–2N0 colorectal cancer.
Methods
We retrospectively evaluated 305 consecutive stage I (T1-2N0M0) colorectal cancer patients who underwent radical surgery from January 2010 to December 2015 at our hospital. The NPS results were divided into 3 groups (0, 1, and 2 groups), and the PNI and CONUT results were divided into 2 groups (low and high groups).
Results
The patients with low PNI had worse overall survival (OS) and disease-free survival (DFS) than those with high PNI (P < 0.001 and P < 0.001, respectively). Multivariate analysis showed that PNI was independently associated with OS and DFS (P < 0.001 and P < 0.001, respectively), but NPS and CONUT results were not.
Conclusion
The PNI is an independent predictor in stage I colorectal cancer, but NPS and CONUT results are not.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer and one of the most common causes of cancer death worldwide [1]. Treatment strategies and prognoses for CRC are mainly based on the American Joint Committee on Cancer (AJCC) TNM pathological stages [2, 3]. Both stage I (T1-2N0M0) and stage II (T3-4N0M0) CRC, in which regional lymph node metastases are absent, have a good prognosis. For stage II disease, some risk factors have been published, and treatment strategies based on those risk factors could significantly improve survival. However, few risk factors have been published for stage I disease, even though recurrence is possible. If treatment strategies could be based on risk factors for stage I disease, as they are for stage II disease, patient outcomes might improve.
Studies have shown that malnutrition and immunological status play a critical role in development of cancers [4, 5]. Therefore, several scores based on nutritional and immunological status have been established to predict the prognosis of CRC. The prognostic nutritional index (PNI) was established in 1980 and reported as an independent predictor for CRC outcomes [6, 7]. Iseki et al. [8] first reported in 2015 that the controlling nutritional status score (CONUT) was an independent outcome predictor for patients with CRC undergoing surgery. In addition, the Naples prognostic score (NPS) was established in 2017 and reported to be an independent outcome predictor for patients with CRC undergoing surgery [9]. Galizia et al. [9] argued that the prognostic value of the NPS was better than that of both CONUT and PNI. Most previous studies assessing the prognostic value of CONUT, NPS, and PNI used patients with disease stages I to IV [7, 9, 10]. However, we suggest that the prognostic values of those indexes should be assessed separately at each stage. Disease progression at different stages produces different nutritional and immunological statuses which may lead to different prognostic values or cut-off values. If the prognostic values and cut-off values of stage I CRC are clarified, it will help the clinicians to provide different treatment strategies or follow-up systems to improve the outcomes. The aim in this study was to evaluate and compare the prognostic value of PNI, CONUT, and NPS in stage I CRC.
Patients and methods
Patients
We studied the medical records of 367 patients who were diagnosed with stage I (T1-2N0M0) CRC and underwent a curative resection at Ajou University Hospital from January 2010 to December 2015. The inclusion criteria were as follows: (1) histologically confirmed adenocarcinoma, (2) stage I according to the 8th edition of the AJCC TNM, and (3) radical surgery. The exclusion criteria were as follows: (1) history of other cancers (n = 39), (2) chemotherapy or radiation therapy before surgery (n = 12), (3) death within 1 month after surgery (n = 2), and (4) non-adenocarcinoma or unknown histology (n = 9). Finally, 305 patients were enrolled in the study.
Data collection
The clinicopathological data analyzed were sex, age, body mass index (BMI), location, histology, tumor size, number of retrieved lymph nodes, lymphatic invasion, and perineural invasion.
Blood samples were analyzed for albumin, cholesterol, neutrophil count, lymphocyte count, and monocyte count less than 2 weeks before surgery. The PNI, neutrophil-to-lymphocyte ratio (NLR), and lymphocyte-to-monocyte ratio (LMR) were calculated using the following formulas: PNI = 10 × albumin (g/dl) + 0.005 × total lymphocyte count (/mm3); NLR = neutrophil count/lymphocyte count; LMR = lymphocyte count/monocyte count. CONUT was calculated using albumin, total lymphocyte count, and total cholesterol (Table 1). The NPS was calculated using albumin, total cholesterol, NLR, and LMR (Table 1).
Patients were seen every 3–6 months for the first 2 years after surgery, every 6 months for the next 3 years, and every year thereafter. Routine physical examinations and carcinoembryonic antigen (CEA) assays were performed at each follow-up visit. Abdominopelvic computed tomography scanning (CT), chest X-ray, and colonoscopy were performed every year and when recurrence was suspected.
Recurrence was determined by radiographic examination and/or histological confirmation through biopsy.
The cut-off date for follow-up was July 2020, and the median follow-up time was 87.0 months (range, 3–125 months). During this period, 21 patients (6.89%) died, and 16 patients (5.25%) experienced recurrence. Overall survival (OS) was defined as the period from surgery to death from any cause or to the last follow-up. Disease-free survival (DFS) was defined as the period from surgery to recurrence, death, or last follow-up.
This study had full ethical approval from the Institutional Review Board of Ajou University School of Medicine.
Statistical analysis
Using X-tile 3.6.1 software (Yale University, New Haven, CT, USA), we determined the cut-off value for a continuous PNI of 49.3, which we identified from the minimum P-value according to the OS (Supplementary Fig. S1) [11]. The total CONUT score cut-off value was set at 3, which is in line with most previous studies [8] [12, 13]. We then divided the patients into high (PNI > 49.3) and low (PNI ≤ 49.3) PNI groups and high (score ≥ 3) and low (score < 3) CONUT groups. Patients were divided by NPS score into group 0, group 1, and group 2, which is in line with the previous study [9]. A Pearson’s x2 or Fisher’s exact test was performed to assess differences between PNI and clinicopathological characteristics. Survival curves were evaluated using the Kaplan–Meier method and were compared using log-rank test. Independent predictors were determined using multivariate Cox regression analyses of OS and DFS. The variables with P < 0.20 in univariate analysis were included in multivariate analysis. P < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 25.0 (IBM, Armonk, NY, USA) and GraphPad Prism 7 (GraphPad Software Inc., La Jolla, CA, USA).
Results
Clinicopathological characteristics
Table 2 shows that the median age was 63 (range: 25–87), and 183 males and 122 females were included in the cohort. The CONUT was normal (score 0–1) for 224 (73.44%) patients, light (score 2–4) for 80 (26.23%) patients, moderate (score 5–8) for 1 (0.33%) patient, and severe for none. By NPS score, group 0 (score 0) comprised 77 (25.25%), group 1 (score 1–2) was 199 (65.24%), and group 2 (score 3–4) was 29 (9.51%) patients. There were 38 (12.46%) patients with PNI ≤ 49.3 and 267 (87.54%) patients with PNI > 49.3.
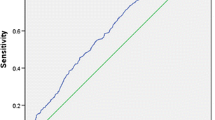
Survival analysis according to the PNI, CONUT, and NPS
The low PNI group had significantly worse OS and DFS than the high PNI group (P < 0.001 and P < 0.001, respectively) (Fig. 1A and B). The high CONUT group also had significantly worse OS and DFS than did the low CONUT group (P = 0.020 and P = 0.045, respectively) (Fig. 2A and B). However, OS and DFS did not differ among the three NPS groups (P = 0.201 and P = 0.478, respectively) (Fig. 3A and B).
Univariate and multivariate analyses for OS and DFS
The univariate analysis for OS showed that P value for age (hazard ratio [HR], 4.846; 95% confidence interval [CI], 1.630–14.405; P = 0.005), histology (HR, 3.020; 95% CI, 0.702–12.983; P = 0.137), location (HR, 1.848; 95% CI, 0.778–4.385; P = 0.164), perineural invasion (HR, 10.461; 95% CI, 1.380–79.304; P = 0.023), albumin (HR, 0.188; 95% CI, 0.025–1.406; P = 0.104), PNI (HR, 0.118; 95% CI, 0.050–0.278; P < 0.001), and CONUT (HR, 3.373; 95% CI, 1.135–10.026; P = 0.029) (Table 3). In multivariate analysis, only PNI (HR, 0.141; 95% CI, 0.054–0.371; P < 0.001) was significantly associated with OS (Model 2, Table 4).
Univariate analysis for DFS showed that P values for location (HR, 2.336; 95% CI, 0.849–6.427; P = 0.100), perineural invasion (HR, 18.461; 95% CI, 2.432–140.108; P = 0.005), CEA (HR, 2.659; 95% CI, 0.758–9.330; P = 0.127), albumin (HR, 0.141; 95% CI, 0.019–1.069; P = 0.058), PNI (HR, 0.097; 95% CI, 0.036–0.260; P < 0.001), and CONUT (HR, 3.353; 95% CI, 0.955–11.766; P = 0.059) were less than 0.2 (Table 3). In multivariate analysis, both perineural invasion (HR, 20.084; 95% CI, 2.126–189.717; P = 0.009) and PNI (HR, 0.105; 95% CI, 0.037–0.297; P < 0.001) were significantly associated with DFS (Model 5, Table 4).
Re-determined the NPS and survival analysis
Using the X-tile software, re-determined the NPS: albumin (normal: ≥ 4.2 g/dL), total cholesterol (normal: > 189 mg/dL), NLR (normal: ≤ 2.3), and LMR (normal: > 4.9). Survival analysis revealed OS significant difference among the three new-NPS groups (P = 0.002), but DFS did not differ among the three new-NPS groups (P = 0.559) (Fig. 4A and B). In the univariate analysis, the new-NPS was significantly associated with OS (P = 0.036), but not in multivariate analysis (P = 0.085). About DFS, in the univariate analysis, the new-NPS was not significantly associated with DFS (P = 0.586).
Survival analysis of PNI in colon and rectal cancer
In colon cancer, the patients with low PNI had significantly worse OS and DFS compared to the patients with high PNI (P < 0.001 and P < 0.001, respectively) (Fig. 5 A and B). Similarly, in rectal cancer, the low PNI group had significantly worse OS and DFS (P < 0.001 and P < 0.001, respectively) (Fig. 6A and B).
Relationships between PNI and clinicopathological characteristics
In the low PNI group, the proportions of patients with age > 63, CEA > 5.0 ng/ml, and albumin < 3.5 g/dl were significantly larger than in the high PNI group (P = 0.001, P = 0.029, and P = 0.002, respectively) (Table 5).
Discussion
Although stage I (T1-2N0M0) CRC generally has a good prognosis because it has superficial tumor invasion and absence of regional lymph node metastasis, a chance of recurrence remains after radical resection. Due to the low incidence of recurrence and death, regular postoperative follow-up usually is not performed in clinical practice, resulting in lack of follow-up data for stage I disease [14]. Therefore, few studies consider stage I disease, and the risk factors have not been sufficiently evaluated.
Nutritional and immunologic statuses are closely associated with tumor growth, metastasis, and recurrence. Various nutritional and immunological status indicators that can be calculated from host serum markers have been established to predict prognosis [7,8,9]. If those easy-to-use serum indicators effectively predict outcome, clinical management of malignancies could be improved. The PNI, which is calculated using serum albumin and total lymphocyte count, has been reported as a predictor in various cancers including CRC [7, 15, 16]. The CONUT, which is based in serum albumin, total lymphocyte count, and total cholesterol concentration, also has been reported to be independently associated with the survival rate of patients with various cancers including CRC [17,18,19]. Since 2017, the NPS based on serum albumin, total cholesterol concentration, NLR, and LMR has been reported as a predictor in CRC [9, 20]. Most previous studies evaluated those indicators in cohorts containing patients in stages I to IV. Disease progression at different stages produce different nutritional and immunological statuses, and treatment strategies at each stage are also different. Therefore those indicators should be evaluated at each stage. Although stage I CRC has a good prognosis, treatment strategies based on risk factors may further improve the survival.
Serum albumin is produced by hepatocytes, and its production is inhibited by cancer-related pro-inflammatory cytokines such as interleukin-6, interleukin-1, and tumor necrosis factor-α, which eventually leads to cancer cachexia [21]. Serum albumin, which represents both nutrition status and disease severity, has been reported to be independently associated with survival rate of several cancers [22]. In the present study, all of the patients were not given nutritional supplementation before surgery, and only 3 (0.98%) patients with albumin < 3.5 g/dl. In the multivariate analysis, considered interactions between albumin and other scoring systems, we found that serum albumin was not independently associated with OS or DFS. Lymphocytes play a key role in cellular immunity. A low lymphocyte count can indicate poor immunologic function, and an insufficient immune response will promote tumor progression [23, 24]. In the present study, the PNI, which was calculated using albumin, total lymphocyte count, was independently associated with both OS and DFS; patients with low PNI had significantly worse OS and DFS than those with high PNI. Therefore, the prognostic value of PNI which represents nutritional and immunologic status was better than that of albumin in patients with stage I CRC. In addition, because our cohort included colon and rectal cancer, we conducted survival analysis according to the tumor location. We found the low PNI group had significantly worse OS and DFS both in the colon and rectal cancer.
In the present study, the cut-off values of PNI, CONUT, and NPS were in line with previous studies [7,8,9], but the results showed that PNI had a better prognostic value than CONUT and NPS in stage I CRC. In addition, unlike PNI and CONUT that had been reported as risk factors in various cancers, the NPS had been established and evaluated only in the two studies about CRC [9, 20]. Therefore, we re-determined the NPS and found it still was not associated with OS or DFS. Among the previous studies of CONUT, the study by Ahiko et al. [25] included the largest number of patients with stage I disease (n = 224) but also included 606 patients with stage II–IV disease. About NPS, the study by Galizia et al. [9] evaluated the 562 patients with CRC, which included 139 patients with stage I disease. Although those studies found that CONUT and NPS results were independently associated with OS and DFS, we suggest that the prognostic value of these indexes be assessed separately at each stage, because disease progression at different stages produces different nutritional and immunological statuses, which could affect the prognostic value of these indexes. Their cohorts contained only a small proportion of stage I patients, meaning that their cohorts had more severe disease than those in our study, in other words, their nutrition and immune conditions might be worse than in our cohort, which could improve the prognostic value of CONUT and NPS results. Although previous studies reported that the new CONUT and NPS indicators were predictors in CRC, the present study showed that these new indicators were not independent risk factors for stage I CRC, which is not robust and requires further research.
In summary, the PNI is a robust and effective risk factor in stage I CRC. In stage I CRC, the patients with low PNI might benefit from efforts to improve nutritional and immunological status before surgery, and a strong follow-up system should be followed during the postoperative period.
Some limitations of this study should be mentioned. First, this study was a retrospective single-center study with a small cohort, producing likely selection bias. Future multi-center, large-scale cohort studies or prospective, large-scale cohort studies are warranted to establish whether our results are robust. Second, in this study, C-reactive protein was not collected from most patients, so we did not include the modified Glasgow prognostic score which has been reported as a predictor in CRC [26, 27]. Despite those limitations, this is the first study to our knowledge to evaluate the prognostic significance of PNI, CONUT, and NPS results in patients with stage I CRC.
Conclusion
This study showed that the PNI is a simple and effective predictor of long-term survival in patients with stage I CRC, whereas CONUT and NPS are not. In stage I CRC, follow-up strategies and treatment plans based on PNI could bring great benefits to clinical practice.
Data availability
The dataset of the current study is available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Siegel RL, Miller KD, Goding Sauer A et al (2020) Colorectal cancer statistics, 2020. CA Cancer J Clin 70:145–164. https://doi.org/10.3322/caac.21601
Benson AB, Venook AP, Al-Hawary MM et al (2018) NCCN Guidelines Insights: Colon Cancer, Version 2.2018. J Natl Compr Canc Netw 16:359–369. https://doi.org/10.6004/jnccn.2018.0021
Benson AB, Venook AP, Al-Hawary MM et al (2020) NCCN Guidelines Insights: Rectal Cancer, Version 6.2020. J Natl Compr Canc Netw 18:806–815. https://doi.org/10.6004/jnccn.2020.0032
Zitvogel L, Pietrocola F, Kroemer G (2017) Nutrition, inflammation and cancer. Nat Immunol 18:843–850. https://doi.org/10.1038/ni.3754
Alwarawrah Y, Kiernan K, MacIver NJ (2018) Changes in nutritional status impact immune cell metabolism and function. Front Immunol 9:1055. https://doi.org/10.3389/fimmu.2018.01055
Buzby GP, Mullen JL, Matthews DC et al (1980) Prognostic nutritional index in gastrointestinal surgery. Am J Surg 139:160–167. https://doi.org/10.1016/0002-9610(80)90246-9
Sun G, Li Y, Peng Y et al (2019) Impact of the preoperative prognostic nutritional index on postoperative and survival outcomes in colorectal cancer patients who underwent primary tumor resection: a systematic review and meta-analysis. Int J Colorectal Dis 34:681–689. https://doi.org/10.1007/s00384-019-03241-1
Iseki Y, Shibutani M, Maeda K et al (2015) Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS ONE 10:e0132488. https://doi.org/10.1371/journal.pone.0132488
Galizia G, Lieto E, Auricchio A et al (2017) Naples prognostic score, based on nutritional and inflammatory status, is an independent predictor of long-term outcome in patients undergoing surgery for colorectal cancer. Dis Colon Rectum 60:1273–1284. https://doi.org/10.1097/DCR.0000000000000961
Takagi K, Buettner S, Ijzermans JNM (2020) Prognostic significance of the controlling nutritional status (CONUT) score in patients with colorectal cancer: a systematic review and meta-analysis. Int J Surg 78:91–96. https://doi.org/10.1016/j.ijsu.2020.04.046
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 10:7252–7259. https://doi.org/10.1158/1078-0432.CCR-04-0713
Yamamoto M, Saito H, Uejima C et al (2019) Prognostic value of combined tumor marker and controlling nutritional status (CONUT) score in colorectal cancer patients. Yonago Acta Med 62:124–130. https://doi.org/10.33160/yam2019.03.017
Yang C, Wei C, Wang S et al (2019) Combined features based on preoperative controlling nutritional status score and circulating tumour cell status predict prognosis for colorectal cancer patients treated with curative resection. Int J Biol Sci 15:1325–1335. https://doi.org/10.7150/ijbs.33671
Costas-Chavarri A, Nandakumar G, Temin S et al (2019) Treatment of patients with early-stage colorectal cancer: ASCO resource-stratified guideline. J Glob Oncol 5:1–19. https://doi.org/10.1200/JGO.18.00214
Park S, Ahn HJ, Yang M et al (2020) The prognostic nutritional index and postoperative complications after curative lung cancer resection: a retrospective cohort study. J Thorac Cardiovasc Surg 160(276–285):e271. https://doi.org/10.1016/j.jtcvs.2019.10.105
Xishan Z, Ye Z, Feiyan M et al (2020) The role of prognostic nutritional index for clinical outcomes of gastric cancer after total gastrectomy. Sci Rep 10:17373. https://doi.org/10.1038/s41598-020-74525-8
Xie H, Nong C, Yuan G et al (2020) The value of preoperative controlling nutritional status score in evaluating short-term and long-term outcomes of patients with colorectal cancer following surgical resection. J Cancer 11:7045–7056. https://doi.org/10.7150/jca.49383
Kuroda D, Sawayama H, Kurashige J et al (2018) Controlling nutritional status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer 21:204–212. https://doi.org/10.1007/s10120-017-0744-3
Takagi K, Yagi T, Umeda Y et al (2017) Preoperative controlling nutritional status (CONUT) score for assessment of prognosis following hepatectomy for hepatocellular carcinoma. World J Surg 41:2353–2360. https://doi.org/10.1007/s00268-017-3985-8
Miyamoto Y, Hiyoshi Y, Daitoku N et al (2019) Naples prognostic score is a useful prognostic marker in patients with metastatic colorectal cancer. Dis Colon Rectum 62:1485–1493. https://doi.org/10.1097/DCR.0000000000001484
Cabrerizo S, Cuadras D, Gomez-Busto F et al (2015) Serum albumin and health in older people: review and meta analysis. Maturitas 81:17–27. https://doi.org/10.1016/j.maturitas.2015.02.009
Gupta D, Lis CG (2010) Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 9:69. https://doi.org/10.1186/1475-2891-9-69
Inoda S, Hirohashi Y, Torigoe T et al (2011) Cytotoxic T lymphocytes efficiently recognize human colon cancer stem-like cells. Am J Pathol 178:1805–1813. https://doi.org/10.1016/j.ajpath.2011.01.004
Iseki Y, Shibutani M, Maeda K et al (2017) The impact of the preoperative peripheral lymphocyte count and lymphocyte percentage in patients with colorectal cancer. Surg Today 47:743–754. https://doi.org/10.1007/s00595-016-1433-2
Ahiko Y, Shida D, Horie T et al (2019) Controlling nutritional status (CONUT) score as a preoperative risk assessment index for older patients with colorectal cancer. BMC Cancer 19:946. https://doi.org/10.1186/s12885-019-6218-8
Park JH, Watt DG, Roxburgh CS et al (2016) Colorectal cancer, systemic inflammation, and outcome: staging the tumor and staging the host. Ann Surg 263:326–336. https://doi.org/10.1097/SLA.0000000000001122
Tokunaga R, Sakamoto Y, Nakagawa S et al (2017) Comparison of systemic inflammatory and nutritional scores in colorectal cancer patients who underwent potentially curative resection. Int J Clin Oncol 22:740–748. https://doi.org/10.1007/s10147-017-1102-5
Author information
Authors and Affiliations
Contributions
Seung Yeop Oh contributed to the design of this paper, analysis of data, revising this paper, and final approval. Guangzhe Pian contributed to the design of this paper, analysis of data, revising this pater, and final approval.
Corresponding author
Ethics declarations
Ethics approval
This study had full ethical approval from the Institutional Review Board of Ajou University School of Medicine.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pian, G., Oh, S.Y. Comparison of nutritional and immunological scoring systems predicting prognosis in T1-2N0 colorectal cancer. Int J Colorectal Dis 37, 179–188 (2022). https://doi.org/10.1007/s00384-021-04043-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-04043-0