Abstract
Background
Anastomotic leakage (AL) is one of the most significant complications after colorectal surgery, affecting length of stay, patient morbidity, mortality, and long-term oncological outcome. Serum C-reactive protein (CRP) level rises in infective and inflammatory states. Elevated CRP has been shown to be associated with anastomotic leak.
Objective
Perform a meta-analysis of current CRP data in AL after colorectal surgery.
Data sources
MEDLINE, EMBASE, CINAHL, CENTRAL databases
Study selection
Comparative studies studying serum CRP levels in adult patients with and without AL after colorectal surgery.
Intervention(s)
Elective and emergency open, laparoscopic or robotic colorectal excisions for cancer and benign pathology.
Main outcome measures
Mean serum CRP measurements between post-operative days (POD) 1 through 7 in patients with and without AL. Perform ROC analysis to determine cut-off CRP values to indicate AL.
Results
Twenty-three studies with 6647 patients (482 AL). Pooled mean time to diagnosis of AL was 7.70 days. AL associated with higher CRP on POD1 (mean difference (MD) 15.19, 95% CI 5.88–24.50, p = 0.001), POD2 (MD 51.98, 05% CI 37.36–66.60, p < 0.00001), POD3 (MD 96.92, 95% CI 67.96–125.89, p < 0.00001), POD4 (MD 93.15, 95% CI 69.47–116.84, p < 0.00001), POD5 (MD 112.10, 95% CI 89.74–134.45, p < 0.00001), POD6 (MD 98.38, 95% CI 80.29–116.46, p < 0.00001), and POD7 (MD 106.41, 95% CI 75.48–137.35, p < 0.00001) compared with no AL. ROC analysis identified a cut-off CRP of 148 mg/l on POD3 with sensitivity and specificity of 95%. On POD4 through POD7, cut-off levels were 123 mg/l, 115 mg/l, 105 mg/l, and 96 mg/l, respectively, with sensitivity and specificity of 100%.
Limitations
Study heterogeneity, some characteristics unreported, no RCT
Conclusions
AL is associated with higher CRP levels on each post-operative day compared to no AL after colorectal surgery. The cut-off CRP values can be used to predict AL to expedite investigation and treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anastomotic leakages (AL) complicate between 3 and 17% of colorectal surgeries involving an anastomosis and are associated with morbidity, utilization of resources and even mortality [1,2,3,4]. AL can worsen long-term oncological outcomes, particularly local recurrence, following colorectal cancer resections [5].
Enhanced recovery after surgery (ERAS) protocols has improved perioperative outcomes of colorectal surgery and contributed to prompt recognition of postoperative complications including AL [6, 7]. Early diagnosis of AL can lead to timely treatment and potentially better outcomes [8, 9]. Conversely, reassurance of absence of AL may facilitate early discharge from hospital or reversal of defunctioning ileostomy [10,11,12].
C-reactive protein (CRP) is a serum protein which is elevated during an inflammatory or infective process and is elevated in AL [13,14,15,16,17]. Since the last meta-analysis of serum CRP in AL in 2013 [17], the number of studies has tripled. We amalgamate current data to understand CRP in the early diagnosis of AL and calculate a cut-off CRP level.
We aimed to conduct a meta-analysis to evaluate the association between serum CRP level and AL after colorectal surgery, and to determine a cut-off CRP value for AL.
Materials and methods
Design and study selection
Eligibility criteria, methodology, and investigated outcome parameters were defined in a review protocol. The methods of this study followed standards of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [18].
All comparative studies investigating serum CRP levels in patients with and without an AL following colorectal resections involving an anastomosis were included. An AL was defined as radiological or operative evidence of defect in the enteric wall at the site of the anastomosis. We considered AL treated conservatively or surgically. Adult male and female patients (18 years or greater) who had open, laparoscopic, or robotic colorectal resection for benign or malignant colorectal pathologies including inflammatory bowel disease, symptomatic diverticular disease, colorectal cancer, or other indication were considered. Elective and emergency colorectal procedures were considered.
Studies reporting postoperative serum CRP values for patients with and without ALs or septic complications were included. Studies not reporting AL outcomes separately from other septic complications were excluded.
Outcome measures
The primary outcome parameter was mean CRP level in mg/L on post-operative days (POD) one to seven.
Search strategy
Thesaurus headings, search operators, and limits were used to develop a search strategy and the search was carried out by two independent authors (DEY, EP) via MEDLINE, EMBASE, CINAHL, and CENTRAL databases (latest search 15 June 2020). The World Health Organization International Clinical Trials Registry http://apps.who.int/trialsearch/, ClinicalTrials.govhttp://clinicaltrials.gov/ and ISRCTN Register http://www.isrctn.com/ were queried for unfinished or unpublished studies. The search terms and strategy are in Appendix 1.
Selection of studies
Two reviewers (DEY, EP) independently executed a preliminary review of titles and abstracts identified through the literature search. Full-text analysis of remaining studies was undertaken and data extraction of studies meeting our inclusion criteria was carried out. Discrepancies were discussed with a third author (SH).
Data extraction and management
An electronic data extraction spreadsheet was prepared in accordance with Cochrane’s recommendations for intervention reviews. The reviewers independently extracted the following data from the studies:
-
Study-related data (first author, publication year, country of research, journal of publication, study design, surgical procedure, surgical approach, and sample sizes)
-
Demographic and clinical information (age, gender, body mass index, use of neoadjuvant radiotherapy, smoking status, cancer staging, level of anastomosis, site of anastomosis)
-
Outcome data
Discrepancies discussed with another author (SH).
Assessment of risk of bias
Two authors independently assessed the methodological quality and risk of bias (DY, EP) using the Newcastle-Ottawa scale (NOS) [19]. The NOS allows authors to evaluate observational studies, specifically considering the method of study group selection, comparability of the groups, and determination of the outcome. The highest score (nine points) denotes lowest risk; moderate risk scores seven or eight, while a high risk of bias would fetch six points. Disagreements were adjudicated by a third author (SH).
Summary measures and synthesis
The primary outcome was mean serum CRP measurements. Thus, mean difference (MD) was calculated between AL and non-AL. Where mean values were not available, the method described by Hozo et al. was used to estimate mean and standard deviation (SD) based on median and interquartile range (IQR) values [20].
The unit of analysis was the individual patient. Where available, attrition and other missing data was recorded. Authors were contacted where information for our outcome was not reported. Our calculations followed the intention-to-treat principle.
One author (DY) used Review Manager 5.3 software to perform the meta-analysis [21]. The calculations were independently analysed by another author (SH). Random-effects modelling was used for analysis. Forest plots with 95% confidence intervals (CI) were used to display the results of each of the calculations.
Cochran Q test (Χ2) was used to assess heterogeneity between studies. To quantify heterogeneity, I2 values were calculated. An I2 value of less than 50% suggests heterogeneity may not be important in this analysis; between 50 and 75% suggests moderate heterogeneity and between 75 and 100%, there may be substantial heterogeneity. Funnel plots were constructed to screen for publication bias where more than ten studies were available for any single outcome.
Leave-one-out sensitivity analysis was performed to gauge the influence of each study on overall effect size and heterogeneity.
For the secondary objective of this study, we performed a ROC curve analysis using MedCalc 13.0 software. We used the method described by DeLong et al. [22] to calculate standard error of the area under the curve (AUC) and an exact Binomial Confidence Interval for the AUC. We calculated associated sensitivity and specificity for all possible threshold values of CRP level and determined the optimal criterion value as cut-off value of CRP for an AL.
The method described by DeLong et al. [22] was used to analyse the ROC curves. MedCalc 13.0 software was used to determine the standard error of the Area Under the Curve (AUC) and to calculate an exact Binomial Confidence Interval for the this. For each threshold value of CRP level, sensitivity and specificity were calculated to understand the best cut-off value for CRP in AL.
Results
The literature search strategy resulted in 1102 articles (Fig. 1). A total of 1008 articles were excluded as they were irrelevant to our research question. Ninety-four potentially eligible studies were further evaluated of which 71 studies were excluded: 38 did not provide serum CRP for AL patients, 10 were review articles, 7 were letters to editor, 6 did not define CRP values (instead utilizing ratios or other inflammatory markers), 3 stated pre-operative CRP values, 3 defined a CRP level as dichotomous with variable cut-off points, 3 reported on the same data set, 2 did not provide numerical data for analysis, and the remaining 2 did not have full text available. Therefore, 23 comparative studies were deemed appropriate for inclusion (Fig. 1). They were all observational studies, with twenty prospective cohort, two retrospective cohort, and one retrospective case-matched cohort comparison study reporting a combined total of 6647 patients who had colorectal resections with primary anastomosis, amongst whom 482 had AL (Table 1) [3, 4, 14, 15, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. Table 1 summarizes data for the included studies (country of origin, journal of publication, study design). Table 2 shows the characteristics of the study populations. All patients underwent either emergency or elective laparoscopic, robotic, or open colorectal surgery for cancer, diverticular disease or inflammatory bowel disease or other indication (Table 2). The pooled mean time to diagnosis of AL was 7.70 ± 1.91 days.
Methodological appraisal
Table 3 summarizes the NOS methodological assessment of the studies. Twelve studies had low risk of bias and 11 studies had moderate risk of bias.
Outcome synthesis
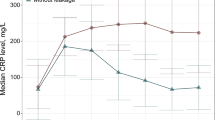
Figures 2 and 3 summarize the results of the outcome calculations.
Forest plots of comparison of CRP on post-operative days. a Day 1, b Day 2, c Day 3, d Day 4, e Day 5, f Day 6, and g Day 7. The solid squares denote the mean difference (MD). The horizontal lines represent the 95% confidence intervals (CIs), and the diamond denotes the pooled effect size. M-H, Mantel Haenszel test
CRP on POD 1
Fourteen studies (2830 patients) were included. Mean serum CRP levels in the AL and no AL groups were 114.45 ± 32.51 and 95.82 ± 29.48, respectively. AL was associated with higher mean CRP level when compared with no AL (MD 15.19, 95% CI 5.88–24.50, p = 0.001). Heterogeneity between studies was moderate (I2 = 67%, p = 0.0002) (Fig. 2a).
CRP on POD 2
Fourteen studies (4559 patients) were included. Mean serum CRP level in AL group was 201.55 ± 29.90 and 145.36 ± 30.67 in the no AL group. AL was associated with higher mean CRP compared to no AL (MD 51.98, 95% CI 37.36–66.60, p < 0.00001). Heterogeneity between studies was significant (I2 = 77%, p < 0.00001) (Fig. 2b).
CRP on POD 3
Twenty studies (5598 patients) were included. Mean serum CRP level in AL and no AL groups were 224.09 ± 51.38 and 122.78 ± 32.05, respectively. AL was associated with higher mean CRP level on POD 3 when compared with no AL (MD 96.92, 95% CI 67.96–125.89, p < 0.00001). There was significant heterogeneity between studies (I2 = 91%, p < 0.00001) (Fig. 2c).
CRP on POD 4
Eleven studies (2955 patients) were included. Mean CRP level in the AL group was 203.84 ± 38.40 whereas it was 104.58 ± 17.06 in the group without AL. AL was associated with higher mean CRP than non-AL (MD 93.15, 95% CI 69.47–116.84, p < 0.00001). There was significant heterogeneity between studies (I2 = 86%, p < 0.00001) (Fig. 2d).
CRP on POD 5
Seven studies (1838 patients) were included. Mean serum CRP level in the AL group was 187.49 ± 35.20 while it was 65.31 ± 23.76 in the no AL group. AL was associated with higher mean CRP level on POD 5 when compared with no AL group (MD 112.10, 95% CI 89.74–134.45, p < 0.00001). There was significant heterogeneity between studies (I2 = 58%, p < 0.00001) (Fig. 2e).
CRP on POD 6
Nine studies (3473 patients) were included. Mean serum CRP level in the AL group was 176.9 ± 32.62 while it was 70.59 ± 20.04 in the no AL group. AL was associated with higher mean CRP level than non-AL (MD 98.38, 95% CI 80.29–116.46, p < 0.00001). There was moderate heterogeneity between studies (I2 = 53%, p < 0.00001) (Fig. 2f).
CRP on POD 7
Eight studies (2143 patients) were included. Mean serum CRP level in AL and no AL groups were 189.29 ± 25.31 and 77.73 ± 23.79, respectively. AL was associated with higher mean CRP level on POD 7 when compared with no AL group (MD 106.41, 95% CI 75.48–137.35, p < 0.00001). There was significant heterogeneity between studies (I2 = 80%, p < 0.00001) (Fig. 2g).
Sensitivity analysis
Leave-one-out sensitivity analysis did not demonstrate any difference in the direction of pooled effect size and no particular study caused skewing. Funnel plots for POD 1 through 4 did not suggest publication bias (Fig. 3).
ROC curve analysis
Outcomes are presented in Fig. 4 and Table 4.
CRP on POD 1
A cut-off CRP level of 110 was shown through ROC analysis to have a sensitivity of 60% (95% CI 32–84%) and specificity of 73% (95% CI 45–92%). The AUC was 0.66 (95% CI 0.47–0.82, P = 0.1110).
CRP on POD 2
A cut-off CRP level of 184 was shown through ROC analysis to have a sensitivity of 71% (95% CI 42–92%) and specificity of 100% (95% CI 77–100%). AUC was 0.91 (95% CI 0.74–0.98, P < 0.0001).
CRP on POD 3
A cut-off CRP level of 148 was shown through ROC analysis to have a sensitivity of 95% (95% CI 75–99%) and specificity of 95% (95% CI 75–95%). AUC was 0.95 (95% CI 0.83–0.99, P < 0.0001).
CRP on POD 4
A cut-off CRP level of 123 was shown through ROC analysis to have a sensitivity of 100% (95% CI 72.0–100%) and specificity of 100% (95% CI 72.0%–100%). AUC was 1.00 (95% CI 0.85–1.00, P < 0.0001).
CRP on POD 5
A cut-off CRP level of 115 was shown through ROC analysis to have a sensitivity of 100% (95% CI 63–100%) and specificity of 100% (95% CI 63–100%). AUC was 1.00 (95% CI 0.79–1.00, P < 0.0001).
CRP on POD 6
A cut-off CRP level of 105 was shown through ROC analysis to have a sensitivity of 100% (95% CI 66–100%) and specificity of 100% (95% CI 66–100%). AUC was 1.00 (95% CI 0.82–1.00, P < 0.0001).
CRP on POD 7
A cut-off CRP level of 96 was shown through ROC analysis to have a sensitivity of 100% (95% CI 59–100%) and specificity of 100% (95% CI 59–100%). AUC was 1.00 (95% CI 0.77–1.00, P < 0.0001).
Discussion
After colorectal surgery, AL can worsen patient morbidity and mortality outcomes [1,2,3,4, 42]. Post-operative serum CRP level can be utilized to predict occurrence of an AL following colorectal resection with primary anastomosis. [8, 43]. We performed a meta-analysis of 23 comparative studies reporting a total of 6647 patients undergoing colorectal resections and primary anastomoses, of whom 482 had ALs. Meta-analysis showed AL was associated with significantly higher serum CRP level on POD 1 through 7 compared to patients who did not have AL. The heterogeneity between studies was moderate in the analysis of CRP level on POD 1, 5, and 6 indicating variable reporting by included studies on these POD. Heterogeneity was high regarding analysis of CRP level on POD 2, 3, 4, and 7 indicating our findings on these days may be less robust.
Our ROC curve analysis determined a threshold CRP level of 148 mg/l on POD 3 with sensitivity and specificity of 95%, and cut-off CRP levels of 123 mg/l on day 4, 115 mg/l on day 5, 105 mg/l on day 6, and 96 mg/l on day 7 for AL with sensitivity and specificity of 100%. We believe our meta-analysis is currently the most comprehensive meta-analysis of literature with inclusion of nearly 7000 patients pooled from 23 studies and i++ndependent MD analyses of CRP levels on 7 consecutive PODs and determined cut-off points on each day. We have demonstrated sensitivity and specificity of 100% associated with our cut-off values on POD 4 to 7 which are higher than those reported by previous meta-analyses Previous meta-analyses have investigated the utility of serum CRP in diagnosing either a post-operative infectious complication or AL. Singh et al. conducted a meta-analysis of 2483 patients who had colorectal resections across seven studies, and the authors found the most sensitive and specific CRP level cut-off values were 172, 124, and 144 mg/L on POD 3, 4 and 5, respectively, with pooled sensitivities of 76%, 79%, and 72% and pooled specificity of 76%, 70%, and 79%, respectively [17]. Our provided cut-off values are nearly comparable with findings of Singh et al. [17] and our higher sensitivity and specificities on the aforementioned PODs further confirms the robustness of these cut-off CRP values. Adamina et al. calculated pooled ROCs and found the best sensitivity and specificity profile of CRP on POD 4 cut-off of 96 mg/L (sensitivity 76%, specificity 61%), but the study was hampered by heterogeneity of the study populations, with different cut-offs for different types of operations (POD 4 cut-off 123 mg/L for open colonic cancer resection (sensitivity 68%, specificity 75%)) [44]. In 2015, Warschow et al. presented a meta-analysis of 1832 patients across six studies and determined the best specificity and sensitivity were on POD 4 with a cut-off level of 135 mg/L, which demonstrated an odds ratio of 11.7 against those who did not have infectious complications. However, a sub-group analysis for AL was not done [45]. Although their cut-off value was lower than our cut-off value, demonstration of the highest sensitivity and specificity on POD4 is consistent with our findings. Gans et al. analyzed the post-operative CRP in 2215 patients who had abdominal surgery; their meta-analysis calculated the threshold CRP on POD 3 of 159 mg/L provided the best sensitivity and specificity (77% sensitivity and 77% specificity) for post-operative infectious complications [46]. Cousins et al. performed a meta-analysis encompassing 2692 patients across 11 studies and demonstrated a cut-off CRP of 130 mg/L or less on POD 3 to have a pooled negative predictive value of 96.7% [47]. Considering that our sample size is much larger in comparison to previous meta-analysis, our findings are much less susceptible to type 2 error. Therefore, we encourage use of our reported cut-off values in prediction of AL.
A number of studies utilized ROC to determine a cut-off CRP level on POD 3 for AL and reported cut-off CRP levels ranging from 149 to 245 mg/L [15, 36,37,38]. Our determined value of POD 3 falls within those reported ranges. Our cut-off value on POD 4 is similar to Ortega-Deballon et al. who found a CRP level of 125 mg/L on POD 4 was the best cut-off point for AL [40]. However, our threshold value on POD 5 is lower than what reported by Reynolds et al. who determined a cut-off point of 132 mg/L on POD 5 [36].
Time to diagnosis of AL in the literature varies, but is typically reported as between seven and 10 days after operation [28]. In our analysis, pooled mean time to diagnosis of AL was 7.70 days ±1.91, with some citing diagnosis as early as 1 day and some as late as 30 days [28, 29]. Thus, in terms of a clinical application of this study, our cut-off levels would still potentially give a diagnostic advantage if CRP level was used as a cue towards further investigations to diagnose AL or reassurance to facilitate earlier discharge.
Randomized controlled trials in the context of AL, a postoperative outcome as compared to an intervention, is not possible. Therefore, the current study represents the best possible available evidence (level 2). Nevertheless, future studies are required to address shortcomings of available evidence. The included studies did not report use of preoperative radiotherapy, level of anastomosis, height of anastomosis, or whether the anastomosis was hand-sewn or stapled. We were therefore unable to consider our outcomes in relation to these potential confounders. Moreover, we were not able to analyse our findings with respect to other important confounder such as emergency or elective nature of surgery, benign or malignant pathology, or the presence of sepsis in the initial operation which can potentially have independent impact on the outcomes. Considering the findings of our study, we encourage use of our cut-off CRP values on POD 4 through 7 as a decision-making tool to predict AL in patients with primary anastomoses after colorectal surgery. The cut-off CRP values, albeit 100% sensitive and specific, warn of the presence of AL, but do not diagnostic in themselves.
Any interpretation of these results should be tempered by the limitations of the study. The studies included were all observational, which are liable to selection bias. Many baseline characteristics of study populations were not reported by the included studies. Twelve studies had moderate risk of bias. Some studies reported their data using median and interquartile range (IQR) or total range and an estimation of mean and standard deviation were calculated using an equation described by Hozo et al. [20], which is a potential source of bias.
Conclusions
This meta-analysis demonstrated AL is associated with significantly higher serum CRP levels on POD 1 through 7 compared with those with no AL after colorectal surgery. Considering the sensitivity and specificity of our determined cut-off CRP levels (100%), we do not hesitate to recommend use of our cut-off CRP levels on POD 4 through 7 to predict AL in order to allow prompt investigation and treatment or reassurance. Future studies should report the outcomes with respect to use of preoperative radiotherapy, level of anastomosis, height of anastomosis, or comparing hand-sewn and stapled anastomoses.
References
Thornton M, Joshi H, Vimalachandran C, Heath R, Carter P, Gur U, Rooney P (2011) Management and outcome of anastomotic leaks. Int J Color Dis 26:313–320
Bertelsen CA, Andreasen AH, Jorgensen T, Harling H (2010) Anastomotic leakage after curative anterior resection for rectal cancer: short and long-term outcome. Color Dis 12:e76–e81
Matthiessen P, Hallbrook O, Andersson M, Rutegard J, Sjodahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Color Dis 6:462–469
Waterland P, Ng J, Jones A, Broadley G, Nicol D, Patel H, Pandey S (2016) Using CRP to predict anastomotic leakage after open and laparoscopic colorectal surgery: is there a difference? Int J Color Dis 31(4):861–868
Koedam TW, Bootsma B, Diejen C, van de Brug T, Kazemier G, Cuesta M, Furst A, Lacy A, Haglind E, Tuynman J, Daams F, Bonjer H (2020) Oncological outcomes after anastomotic leakage after surgery for colon or rectal cancer: increased risk of local recurrence. Ann Surg. https://doi.org/10.1097/SLA.0000000000003889
Ni X, Jia D, Chen Y, Wang L, Suo J (2019) Is the Enhanced Recovery after Surgery (ERAS) program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg 23:1502–1512
Brown JK, Singh K, Dumitru R, Chan E, Kim MP (2018) The benefits of enhanced recovery after surgery programs and their application in cardiothoracic surgery. Methodist Debakey Cardiovasc J 14(2):77–88
Macarthur DC, Nixon SJ, Aitken RJ (1998) Avoidable deaths still occur after large bowel surgery: Scottish audit of surgical mortality, Royal College of Surgeons of Edinburgh. Br J Surg 85(1):80–83
Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P (1999) Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg 189(6):554–559
Lasithiotakis K, Aghahoseini A, Alexander D (2016) Is early reversal of defunctioning ileostomy a shorter, easier and less expensive operation? World J Surg 40:1737–1740. https://doi.org/10.1007/s00268-016-3448-7
Bakx R, Busch ORC, van Geldere D, Bemelman WA, Slors JFM, van Lanschot JJB (2003) Feasibility of early closure of loop ileostomies: a pilot study. Dis Colon Rectum 46:1680–1684
Menegaux F, Jordi-Galais P, Turrin N, Chigot J (2002) Closure of small bowel stomas on postoperative day 10. Eur J Surg 168:713–715
Lane JC, Wright S, Burch J, Kennedy RH, Jenkins JT (2013) Early prediction of adverse events in enhanced recovery based upon the host systemic inflammatory response. Color Dis 15(2):224–230
Lagoutte N, Facy O, Ravoire A, Chalumeau C, Jonval L, Rat P, Ortega-Deballon P (2012) C-reactive protein and procalcitonin for the early detection of anastomotic leakage after elective colorectal surgery: pilot study in 100 patients. J Visc Surg 149:e345–e349
Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, McMillan DC (2012) C-reactive protein as a marker of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol 19:4168–4177
Paradis T, Zorigbaatar A, Trepanier M, Fiore JF Jr, Fried GM, Feldman LS, Lee L (2020) Meta-analysis of the diagnostic accuracy of C-reactive protein for infectious complications of laparoscopic versus open colorectal surgery. J Gastrointest Surg 24(6):1392–1401
Singh PP, Zeng ISL, Srinivasa S, Lemanu DP, Connoly AB, Hill AG (2013) Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg 83(Suppl 1):23
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta analyses: the PRISMA statement. J Clin Epidemiol 62(7):1006–1012
Wells G, Shea B, O’Connell D, Paterson J, Welch V, Losos M, Tugwell P (2019) The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. Ottawa Hospital Research Institute http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 9 July 2020
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Review Manager (RevMan) [Computer Program]. Version 5.3 (2014) Copenhagen: the Nordic Cochrane Centre, The Cochrane Collaboration
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):836–845
The Italian ColoRectal Anastomotic Leakage (iCral) Study Group (2020) Anastomotic leakage after elective colorectal surgery: a prospective multicentre observational study on the use of the Dutch leakage score, serum procalcitonin and serum C-reactive protein for diagnosis. BJS Open 4(3):499–507
Messias BA, Botelho RV, Saad SS, Mocchetti ER, Turke KC, Waisberg J (2020) Serum C-reactive protein is a useful marker to exclude anastomotic leakage after colorectal surgery. Sci Rep 10(1):1687
Guevara-Morales G, Regalado-Torres MA, Cantarell-Castillo E, Castro-Salas R, Maldonado-Barron R, Castellanos-Juarez JC (2018) Utility of C-reactive protein in the early diagnosis of anastomotic leakage in colorectal surgery. Cirurgia y Cirujanos 86:381–385
Pantel HJ, Jasak LJ, Ricciardi R, Marcello PW, Roberts PL, Schoetz DJ Jr (2019) Should they stay or should they go? The utility of C-reactive protein in predicting readmission and anastomotic leak after colorectal resection. Dis Colon Rectum 62(2):241–247
Sparreboom CL, Komen N, Rizopoulos D, Verhaar AP, Dik WA, Wu Z, van Westreenen HL, Doorneborsch PG, Dekker JWT, Menon AG, Daams F, Lips D, van Grevenstein WMU, Karsten TM, Bayon Y, Peppelenbosch MP, Wolthuis AM, D’Hoore A, Lange JF (2020) A multicentre cohort study of serum and peritoneal biomarkers to predict anastomotic leakage after rectal cancer resection. Color Dis 22(1):36–45
Stearns AT, Liccardo F, Tan K-N, Sivikroz E, Aziz O, Jenkins JT, Kennedy RH (2019) Physiological changes after colorectal surgery suggest that anastomotic leak is an early event: a retrospective cohort study. Color Dis 21(3):297–306
Fukada M, Matsuhashi N, Takahashi T, Imai H, Tanaka Y, Yamaguchi K, Yoshida K (2019) Risk and early predictive factors of anastomotic leakage in laparoscopic low anterior resection for rectal cancer. World J Surg Oncol 17(1):178
Munoz JL, Alvarez MO, Cuquerella V, Miranda E, Pico C, Flores R, Resalt-Pereira M, Moya P, Perez A, Arroyo A (2018) Procalcitonin and C-reactive protein as early markers of anastomotic leak after laparoscopic colorectal surgery within an enhanced recovery after surgery (ERAS) program. Surg Endosc 32(0):4003–4010
Rybakov E, Shelygin Y, Tarasov M, Sukhina M, Zarodniuk I, Alexeev M, Chernyshov S (2018) Risk factors and inflammatory predictors for anastomotic leakage following total mesorectal excision with defunctioning stoma. Pol Przegl Chir 90(3):31–36
Zawadzki M, Krzystek-Korpacka M, Gamian A, Witkievicz W (2018) Serum cytokines in early prediction of anastomotic leakage following low anterior resection. Videosurg Other Miniinvasive Tech 13(1):33–43
Bilgin IA, Hatipoglu E, Aghayeva A, Arikan AE, Incir S, Torun MM, Dirican A, Erguney S (2017) Predicting value of serum procalcitonin, C-reactive protein, drain fluid culture, drain fluid interleukin-6 and tumor necrosis factor-alpha levels in anastomotic leakage after rectal resection. Surg Infect 18(3):350–356
Mik M, Dziki L, Berut M, Trzcinski R, Dziki A (2018) Neutrophil to lymphocyte ratio and c-reactive protein as two predictive tools of anastomotic leak in colorectal cancer open surgery. Dig Surg 35(1):77–84
Reynolds IS, Boland MR, Reilly F, Deasy A, Majeed MH, Deasy J, Burk JP, McNamara DA (2017) C-reactive protein as a predictor of anastomotic leak in the first week after anterior resection for rectal cancer. Color Dis 19:812–818
Kostic Z, Slavkovic D, Mijuskovic Z, Panisic M, Ignjatovic M (2015) C-reactive protein in drainage fluid as a predictor of anastomotic leakage after elective colorectal resection. Vojnosanitetski pregled 73:228–233. https://doi.org/10.2298/VSP141031017K
Zawadzki M, Czarnecki R, Rzaca M, Obuszko Z, Velchuru VR (2015) C-reactive protein and procalcitonin predict anastomotic leaks following colorectal cancer resections—a prospective study. Videosurg Other Miniinvasive Tech 10(4):567–573
Garcia-Granero A, Frasson M, Flor-Lorente B, Blanco F, Puga R, Carratala A, Garcia-Granero E (2013) Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum 56:475–483
Almeida AB, Faria G, Moreira H, Pinto-de-Sousa J, Correia-da-Silva P, Maia JC (2012) Elevated serum c-reactive protein as a predictive factor for anastomotic leakage in colorectal surgery. Int J Surg 10(2):87–91
Ortega-Deballon P, Radais F, Facy O, D’Athis P, Masson D, Charles PE, Cheynel N, Favre J-P, Rat P (2010) C-reactive protein is early predictor of septic complications after elective colorectal surgery. World J Surg 38:808–814
Woeste G, Muller C, Bechstein WO, Wullstein C (2010) Increased serum levels of C-reactive protein precede anastomotic leakage in colorectal surgery. World J Surg 34:140–146
Leahy J, Schoetz D, Marcello P, Read T, Hall J, Roberts P, Rocco R (2014) What is the risk of clinical anastomotic leak in the diverted colorectal anastomosis? J Gastrointest Surg 18:1812–1816
Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P (1999) Management of anastomotic leakage after nondivertied large bowel resection. J Am Coll Surg 189(6):554–559
Adamina M, Steffen T, Tarantino I, Buetner U, Schmied BM, Warschkow R (2015) Meta-analysis of the predictive value of C-reactive protein for infectious complications in abdominal surgery. Br J Surg 102:590–598
Warschkow R, Beutner U, Steffen T, Muller SA, Schmied B, Guller U, Tarantino I (2012) Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg 256:245–250
Gans SL, Atema JJ, van Dieren S, Groot Koerkamp B, Boermeester MA (2015) Diagnostic value of C-reactive protein to rule out infectious complications after minor abdominal surgery: a systematic review and meta-analysis. Int J Color Dis 30(7):861–873
Cousin F, Ortega-Deballon P, Bourredjem A, Doussot A, Giaccaglia V, Fournel I (2016) Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery: a meta-analysis. Ann Surg 264(2):252–256
Author information
Authors and Affiliations
Contributions
Data acquisition: Peterknecht, Elizabeth; Yeung, Denise; Hajibandeh, Shahin; Hajibandeh, Shahab.
Drafting of manuscript: Yeung, Denise; Hajibandeh, Shahab; Hajibandeh, Shahin.
Critical revision of manuscript: Hajibandeh, Shahin; Torrance, Andrew.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOC 62 kb)
Rights and permissions
About this article
Cite this article
Yeung, D.E., Peterknecht, E., Hajibandeh, S. et al. C-reactive protein can predict anastomotic leak in colorectal surgery: a systematic review and meta-analysis. Int J Colorectal Dis 36, 1147–1162 (2021). https://doi.org/10.1007/s00384-021-03854-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03854-5