Abstract
Background
The aim of the study was to determine factors predicting lymph node metastasis in patients with T1 or T2 colon cancer.
Methods
A total of 906 patients with T1 or T2 colon cancer who underwent colon resection with regional lymphadenectomy in a tertiary hospital, from January 2008 to December 2013, were analyzed. The prognostic factors for LN metastasis and the risk factors for survival were analyzed.
Results
There were 728 patients (80.4%) without lymph node metastasis (LN-negative group) and 178 patients (19.6%) with lymph node metastasis (LN-positive group). Tumor invasion depth (P < 0.001), lymphatic invasion (P < 0.001), and perineural invasion (P = 0.008) were significantly different between the two groups. During the median follow-up period of 69 months, the 5-year disease-free survival rate was 98.6% for the LN-negative group and 92.8% for the LN-positive group (P ≤ 0.001). In multivariate analysis, influencing factors associated with disease-free survival rate were LN metastasis (P = 0.001) and perineural invasion (P = 0.040). Female, depth of tumor invasion (P = 0.001), and lymphatic invasion (P < 0.001) were significant independent predictive factors for lymph node metastasis in multivariate analysis.
Conclusion
Positive LN status predicted poor disease-free survival in patients with early cancer. This suggests that depth of tumor invasion ≥ sm2 and the presence of lymphatic invasion in early colon cancer provide useful information to determine which patients would benefit from radical surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prognosis of colon cancer is related to tumor node metastasis stage, and depth of tumor invasion into the bowel wall is an essential component of colon cancer staging systems.[1] Early colon cancer is defined as cancer with depth of invasion limited to the mucosa or submucosa regardless of the presence or absence of lymph node (LN) metastasis.[2] Mucosal cancers in which the cancer cells are localized to the mucosa have little risk of LN metastasis, but patients with submucosal cancers experience about 10% LN metastasis.[3] In other words, submucosal cancer may result in LN metastasis after endoscopic resection. Despite the limited depth of tumor invasion into the bowel, prognosis for patients with LN metastasis may be worse than that of those without.[1] Therefore, risk of LN metastasis should be assessed to consider whether additional surgical colon resection should be performed. The risk factors of LN metastasis in early colon cancer remain unknown. This study analyzed the prognostic factors for LN metastasis in patients who had early colon cancer treated with radical surgery and tried to confirm the treatment with a large number of data.
Patients and methods
This is a single-center, retrospective cohort study. From January 2008 to December 2013, a total of 1516 patients underwent colon resection for early colon cancer (T1, T2). Patients with the following were excluded: palliative surgery (n = 23), surgery for recurrence or metachronous tumors (n = 8), stage IV disease (n = 1), familial adenomatous polyposis or hereditary nonpolyposis colorectal cancer (n = 41), no residual tumor on pathologic report after preoperative polypectomy (n = 119), or no result of accurate depth on pathologic report (n = 398). A total of 906 patients were ultimately analyzed and divided into a lymph node-negative group and a lymph node-positive group (Fig. 1).
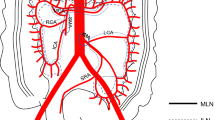
All patients underwent a standard colectomy and regional lymphadenectomy according to tumor location. Resected specimens were evaluated for macroscopic ulceration, tumor size, differentiation, depth of tumor invasion (sm1: submucosa invasion depth < 1000 μm; sm2: submucosa invasion depth ≥ 1000, < 2000 μm; sm3: submucosa invasion depth ≥ 2000 μm), number of lymph nodes retrieved, number of lymph node metastases, lymphatic invasion, perineural invasion, and vascular invasion.
After surgery, the patients were assessed with physical examinations, a serum carcinoembryonic antigen assay, and laboratory findings once every 3 months for the first 2 years. Abdominopelvic computed tomography and chest computed tomography were performed every 6 months. Esophagogastroduodenoscopy and colonoscopy were performed the first year and then biannually for 5 years thereafter.
Statistical analyses were conducted using SPSS software version 25 (IBM Corp., Armonk, NY, USA). Differences between groups were tested using the chi-square test or Fischer’s exact test. Student’s t test was applied to continuous variables. The associations between LN positivity and clinicopathologic factors were assessed using logistic regression analysis. Factors determined to be significant in univariate analyses were analyzed with multivariate logistic regression, and an OR and 95% CI were calculated for each factor. The overall and disease-free survival rates were calculated using the Kaplan-Meier method. A P value < 0.05 was considered statistically significant.
Results
Patient demographics and clinicopathologic characteristics
There were 728 patients (80.4%) without lymph node metastasis (LN-negative group) and 178 patients (19.6%) with lymph node metastasis (LN-positive group). The median age was 60 years (range 50–71). There were 532 men (58.7%) and 374 (41.3%) women. There were more men in the LN-negative group and more women in the LN-positive group (62.0:38.0 vs. 45.5:54.5, P < 0.001). Routes of access were open surgery (13.9%), hand-assisted laparoscopic surgery (13.8%), laparoscopic surgery (47.1%), single-port-assisted laparoscopic surgery (25.1%), and robotic surgery (0.1%). Most patients had a single tumor (94.2%). Other comparisons showed no significant differences between the groups. The demographics and characteristics of patients are presented in Table 1.
Surgical outcomes
Regarding histological type, poorly differentiated, undifferentiated, and mucinous adenocarcinomas were identified in the LN-positive group, representing a significant difference compared with the LN-negative group (P = 0.045). Tumor invasion depth was significantly different between the two groups (P < 0.001). The median number of LNs retrieved was 18.5, and there was no significant difference between the groups. Lymphatic invasion was observed in 71 patients (41.5%) in the LN-positive group, significantly more frequently than the 90 (13.1%) patients in the LN-negative group (P < 0.001). The proportions of patients with LN metastasis were sm1 3.7% (1/27), sm2 9.6% (10/104), sm3 13.0% (19/146), and T2 23.5% (148/629). Perineural invasion was identified in 11 patients (6.7%) in the LN-positive group, significantly more frequently than the 16 patients (2.5%) in the LN-negative group (P = 0.008). No difference was observed between the two groups in gross type, tumor size, or vascular invasion. The pathology outcomes are shown in Table 2.
Factors influencing lymph node metastasis
Influencing factors associated with LN metastasis are presented in Table 3. In univariate analysis, female, depth of tumor invasion, lymphatic invasion, and perineural invasion were significant predictive factors for lymph node metastasis. Multivariate analysis showed that female, depth of tumor invasion (P = 0.001), and lymphatic invasion (P < 0.001) were significant independent predictive factors for lymph node metastasis.
When grouping by number of factors influencing LN metastasis identified in our study, of the 178 patients that were LN positive, there were no patients in the no-risk group (P = 0.035), 108 patients with one factor were in the low-risk group (14.7%, P < 0.001), and 70 patients with two factors were in the high-risk group (45.8%, P < 0.001) (Fig. 2).
Survival and prognostic factors
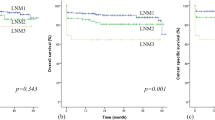
Influencing factors associated with disease-free survival rates are presented in Table 4. The median follow-up was 69 months (range 40–99). In multivariate analysis, influencing factors associated with disease-free survival rate were LN metastasis (P = 0.001) and perineural invasion (P = 0.040). The 5-year disease-free survival rate was 98.6% for the LN-negative group and 92.8% for the LN-positive group (P ≤ 0.001) (Fig. 3).
Discussion
Colonoscopy has been widely performed as a screening test for early colon cancer, and the frequency of detection of early colon cancer is gradually increasing. LN metastasis in colon cancer is an important factor in prognosis. When the tumor is confined to the mucosal layer, LN metastasis does not occur because there are no lymphatic vessels in the layer. Accordingly, depth of submucosal invasion is a significant predictor of LN metastasis.[4,5,6,7,8,9,10] Han et al. [4] reported a 19.3% risk of LN metastasis in patients with depth of invasion > 1900 μm. Mou et al. [11] stated that 14.6% of patients with invasion depth > 1000 μm had LN metastasis. According to previous studies, the incidence of LN metastasis in early cancer with depth of submucosal invasion ≥ 1000 μm was approximately 10% [4], in agreement with our results. We demonstrated incidence of LN metastasis for all patients of 19.7% according to depth of invasion. The proportions of patients with LN metastasis were sm1 3.7%, sm2 9.6%, sm3 13.0%, and T2 23.5%. LN metastasis for two group sm1 vs. sm2, 3, T2 was 3.7% and 20.1% (P = 0.045%). The deeper was the depth, the higher was the rate of LN metastasis. Thus, a favorable outcome can be expected if radical surgery with lymphadenectomy is performed in patients with sm2 colon cancer.
Several studies have attempted to evaluate predictive factors of LN metastasis.[1, 12,13,14,15] In the present study, the presence of lymphatic invasion or perineural invasion was a significant predictive factor.[1] These factors are still controversial. Chok et al. [16] suggested that half of patients with lymphovascular invasion experience lymph node metastasis. Han et al. [4] reported that lymphatic invasion was associated with higher risk of LN metastasis in univariate analysis but not in multivariate analysis. Yim et al. [17] reported that the most powerful clinicopathological parameter for predicting LN metastasis was lymphatic invasion. Huh et al. [1] reported that the presence of lymphovascular or perineural invasion was associated with lymph node metastasis. Similarly, our results showed that lymphatic invasion and perineural invasion were significant in univariate analysis, but perineural invasion was not statistically significant in multivariate analysis.
Based on our findings, when grouping by number of factors influencing LN metastasis, the higher was the risk factor count, the higher was the LN metastasis probability.
This study has some limitations. It was a single-center, retrospective study with type 2 error. In the historical pathologic report, 398 patients who did not have a definite value for depth were excluded, reducing the sample size. Furthermore, tumor budding was investigated as a risk factor but was excluded due to other studies. The findings of this study should be further verified using a larger sample.
Conclusions
In conclusion, our study indicates that depth of tumor invasion ≥ sm2 and lymphatic invasion are significant independent factors predicting LN metastasis in patients with T1 and T2 colon cancer. In addition, we found that LN metastasis and perineural invasion were significantly correlated with disease-free survival. Our study suggests that the depth of tumor invasion ≥ sm2 and the presence of lymphatic invasion in early colon cancer provide useful information to determine which patients would benefit from radical surgery.
References
Huh JW, Kim HR, Kim YJ (2010) Lymphovascular or perineural invasion may predict lymph node metastasis in patients with T1 and T2 colorectal cancer. J Gastrointest Surg 14:1074–1080
(1983) General rules for clinical and pathological studies on cancer of the colon, rectum and anus. Part II. Histopathological classification. Japanese Research Society for Cancer of the Colon and Rectum. Jpn J Surg 13:574–598
Park YJ, Kim WH, Paeng SS, Park JG (2000) Histoclinical analysis of early colorectal cancer. World J Surg 24:1029–1035
Han J, Hur H, Min BS, Lee KY, Kim NK (2018) Predictive factors for lymph node metastasis in submucosal invasive colorectal carcinoma: a new proposal of depth of invasion for radical surgery. World J Surg 42:2635–2641
Kikuchi R, Takano M, Takagi K, Fujimoto N, Nozaki R, Fujiyoshi T, Uchida Y (1995) Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum 38:1286–1295
Ishikawa Y, Akishima-Fukasawa Y, Ito K, Akasaka Y, Yokoo T, Ishii T, Toho Study Group for Cancer Biological B (2008) Histopathologic determinants of regional lymph node metastasis in early colorectal cancer. Cancer 112:924–933
Ueno H, Mochizuki H, Hashiguchi Y, Shimazaki H, Aida S, Hase K, Matsukuma S, Kanai T, Kurihara H, Ozawa K, Yoshimura K, Bekku S (2004) Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology 127:385–394
Volk EE, Goldblum JR, Petras RE, Carey WD, Fazio VW (1995) Management and outcome of patients with invasive carcinoma arising in colorectal polyps. Gastroenterology 109:1801–1807
Seitz U, Bohnacker S, Seewald S, Thonke F, Brand B, Braiutigam T, Soehendra N (2004) Is endoscopic polypectomy an adequate therapy for malignant colorectal adenomas? Presentation of 114 patients and review of the literature. Dis Colon Rectum 47:1789–1796 discussion 1796-1787
Kudo S, Kashida H, Tamura T, Kogure E, Imai Y, Yamano H, Hart AR (2000) Colonoscopic diagnosis and management of nonpolypoid early colorectal cancer. World J Surg 24:1081–1090
Mou S, Soetikno R, Shimoda T, Rouse R, Kaltenbach T (2013) Pathologic predictive factors for lymph node metastasis in submucosal invasive (T1) colorectal cancer: a systematic review and meta-analysis. Surg Endosc 27:2692–2703
Rasheed S, Bowley DM, Aziz O, Tekkis PP, Sadat AE, Guenther T, Boello ML, McDonald PJ, Talbot IC, Northover JM (2008) Can depth of tumour invasion predict lymph node positivity in patients undergoing resection for early rectal cancer? A comparative study between T1 and T2 cancers. Colorectal Dis 10:231–238
Bayar S, Saxena R, Emir B, Salem RR (2002) Venous invasion may predict lymph node metastasis in early rectal cancer. Eur J Surg Oncol 28:413–417
Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR (2002) Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum 45:200–206
Goldstein NS, Hart J (1999) Histologic features associated with lymph node metastasis in stage T1 and superficial T2 rectal adenocarcinomas in abdominoperineal resection specimens. Identifying a subset of patients for whom treatment with adjuvant therapy or completion abdominoperineal resection should be considered after local excision. Am J Clin Pathol 111:51–58
Chok KS, Law WL (2007) Prognostic factors affecting survival and recurrence of patients with pT1 and pT2 colorectal cancer. World J Surg 31:1485–1490
Yim K, Won DD, Lee IK, Oh ST, Jung ES, Lee SH (2017) Novel predictors for lymph node metastasis in submucosal invasive colorectal carcinoma. World J Gastroenterol 23:5936–5944
Author information
Authors and Affiliations
Contributions
Study proposal, design, analysis, data collection, and writing of manuscript are attributed to You Jin Lee and Jung Wook Huh. Responsibility to correspondence is attributed to Jung Wook Huh and Woo Yong Lee. All authors attributed to the enrollment of patients and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, Y.J., Huh, J.W., Shin, J.K. et al. Risk factors for lymph node metastasis in early colon cancer. Int J Colorectal Dis 35, 1607–1613 (2020). https://doi.org/10.1007/s00384-020-03618-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03618-7