Abstract
Purpose
Preoperative short-course radiotherapy (PSRT) and preoperative long-course radiotherapy (PLRT) are standard treatment regimens for locally advanced rectal cancer. However, whether the efficacy and safety of PSRT with delayed surgery (more than 4 weeks) are superior to those of PLRT remains unresolved and was explored in this meta-analysis.
Methods
Studies published in PubMed, Embase, the Cochrane Library, and ClinicalTrials.gov databases were systematically searched. RevMan 5.3 was used to calculate pooled hazard ratios (HR) and relative risk (RR).
Results
Seven studies including 4973 patients were identified in the meta-analysis. Pooled statistics showed that there was no statistically significant difference in overall survival (HR = 1.30, 95% CI 0.58–2.89, P = 0.52) or disease-free survival (HR = 1.10, 95% CI 0.73–1.66, P = 0.64) between the preoperative short-course and long-course radiotherapy groups. Moreover, pathological complete remission, early postoperative complications, treatment-related grade 3/4 toxicity, local recurrence, and distant metastasis were similar between the two groups. Interestingly, a subgroup analysis revealed that preoperative short-course radiotherapy without adjuvant chemotherapy not only resulted in lower treatment-related grade 3/4 toxicity than the long-course radiotherapy group (RR = 0.19, 95% CI 0.08–0.48, P < 0.01) but also resulted in significantly lower overall survival and pathological complete remission (P = 0.02, P < 0.01, respectively). Disappointingly, pooled statistics observed few advantages over long-course radiotherapy in short-course radiotherapy with the adjuvant chemotherapy subgroup.
Conclusions
PSRT with delayed surgery was as effective as PLRT for the management of locally resectable rectal cancer. However, not adding additional chemotherapy to PSRT not only significantly decreased grade 3/4 toxicity but also decreased pathological complete remission and overall survival.
Trial registration
The protocol for this meta-analysis was prospectively registered with PROSPERO (CRD42019133641)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to global cancer statistics in 2018 [1], Asia (followed by Europe and USA) had the highest number of cancer cases and highest cancer-related death rate worldwide (both sexes). Colorectal cancer is the third leading cause of new cases, accounting for 10.2% of the world, and is the second leading cause of cancer-related death following lung cancer. With the rapid development of radiation technology, preoperative radiotherapy, which has been shown to increase local control without improving the survival rate, is currently recognized as the standard treatment modality for locally advanced rectal cancer [2,3,4,5,6].
Although both the latest National Comprehensive Cancer Network guidelines version 3.2018 (NCCN 2018 V3) [7] and the European Society for Medical Oncology (ESMO) guidelines [8] recommend preoperative short-course radiotherapy (PSRT) as one of the standard treatments for locally advanced rectal cancer, neither explicitly provides an optimal interval between the end of short-course radiotherapy and surgery. Additionally comparisons of the efficiency and safety between PSRT with delayed surgery and preoperative long-course radiotherapy (PLRT) have provided controversial results. To be consistent with previous studies [9, 10], in our meta-analysis, we defined the time interval for delayed radiotherapy as at least 4 weeks from the completion of radiation. Randomized controlled trials (RCTs) have provided conflicting results regarding the benefit of PSRT with delayed surgery. Bujko et al. [11] and Markovina et al. [12] reported that patients undergoing PSRT after which surgery was delayed for more than 4 weeks had better survival than those undergoing PLRT concomitant with chemotherapy, while Kairevičė et al. [13] and Latka et al. [14] came to the opposite conclusion. The results regarding treatment-related grade 3/4 toxicity, postoperative complications (PCs), downstaging, and pathological complete remission (pCR) have also been inconsistent [11, 12, 15,16,17,18]. Therefore, we performed this meta-analysis to explore the efficiency and safety of PSRT with delayed surgery versus preoperative conventional radiotherapy for locally resectable rectal cancer.
Materials and methods
Search strategy
Eligible studies published in PubMed, Embase, the Cochrane Library, and ClinicalTrials.gov were systematically searched without limits for language. The search date ranged from inception to May 1, 2019. The search strategy included the following terms: “rectal neoplasms/radiotherapy,” “rectal neoplasms/surgery,” “radiotherapy, adjuvant,” “conventional chemoradiotherapy,” “long-course radiotherapy,” “short-course radiotherapy,” and “preopera*” and combinations of these terms constructed using the Boolean operators “AND” and “OR”. Relevant articles were also extracted manually from the references of retrieved publications. Two reviewers (Qiaoli Wang and Yongping Huang) independently searched the aforementioned databases for eligible articles.
Inclusion criteria
Our inclusion criteria were designed according to Participants, Intervention, Comparison and Outcomes, Study design (PICOS) principles, as follows: (1) P: patients diagnosed with rectal cancer by biopsy; (2) I: experimental group: PSRT (5 × 5Gy) followed by delayed surgery at least 4 weeks later, ignoring whether adjuvant or consolidation chemotherapy was given; control group: PLRT (total dose at least 45 Gy at 1.8–2 Gy/f) followed by surgery at least 4 weeks later regardless of whether the adjuvant or consolidation chemotherapy was given; (3) C: comparison of the efficacy and side effects of the experimental and the control group treatment; (4) O: overall survival (OS), disease-free-survival (DFS), treatment-related grade 3/4 toxicity, early postoperative complications (PCs; defined as reversible complications related to surgery, such as anastomotic leakage, wound infection, intra-abdominal infection, ileus, and other complications requiring re-operation), local recurrence (LR; defined as an intrapelvic recurrence following primary rectal cancer resection, with or without distal metastasis), distant metastasis (DM; documented in any organ) and pathological complete rate (pCR); and studies reporting one of these outcomes were included; and (5) S: randomized controlled trials (RCTs) and non-RCTs.
Exclusion criteria
The exclusion criteria were as follows: (1) patients with clinical stage IV or synchronous distant metastases; (2) the preoperative radiation dose did not meet the inclusion criteria; (3) the time interval to surgery was less than 4 weeks in either the PSRT or PLRT arm; (4) single arms, reviews, case reports, letters, comments, etc.; and (5) studies lacking relevant statistics.
Data extractions
Data were independently extracted by two reviewers (Wang Qiaoli and Huang Yongping) and recorded in a standard extraction form. The relevant information extracted from the selected studies is listed as follows: (1) baseline characteristics: name of the first author, year of publication, resources and study year, follow-up time, number of patients, study type, clinical stage of the tumor, tumor location, interventions, comparison, and ages; (2) outcomes: OS, DFS, treatment-related grade 3/4 toxicity, PCs, LR, DM, and pCR. Disagreements between the two authors were resolved by a group discussion.
Data analysis
Where a meta-analysis was judged to be appropriate, pooled statistics analyses were performed using Review Manager software 5.3 (RevMan 5.3) supplied by the Cochrane Collaboration. Dichotomous variables were calculated as the relative risk (RR). Hazard ratios (HR) were selected as the effect indicator to pool survival statistics based on the method published by Tierney et al. [19]. Additionally, 95% confidence intervals (CI) were calculated for count data. If the HR could not be extracted directly from the eligible articles, Engauge Digitizer software was used to extract relevant information. We used the Mantel-Haenszel method to estimate the typical RR and risk difference. χ2 and I2 test statistics were used to investigate heterogeneity. If the P value of the χ2 test was < 0.10 and the I2 value was > 50%, the random effects model was used (significant heterogeneity). In contrast, the fixed effects model was used in cases with no significant heterogeneity. A sensitivity analysis was performed to confirm the robustness of the results by omitting one study at a time.
The subgroup analysis was based on chemotherapy in the PSRT group to reduce some heterogeneity of the treatment effect. The two subgroups were classified as follows: one, the subgroup was the PSRT plus pre/postoperative adjuvant chemotherapy subgroup, and two, the PSRT without adjuvant chemotherapy subgroup. Thus, the effect of chemotherapy in the PSRT group could be clearly observed.
The protocol for this meta-analysis was prospectively registered with PROSPERO (CRD42019133641).
Quality assessment and risk of bias
The risk of bias was assessed by two reviewers (Wang and Huang), and discrepancies were resolved by a group discussion. The quality of the RCTs was evaluated by the Cochrane risk of bias assessment tool, which includes seven items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Each item was assessed as having a high, low, or unclear risk of bias [20]. The quality of the non-RCTs was evaluated by the Newcastle-Ottawa Scale (NOS), which contains three perspectives: selection, comparability, and the outcomes of studies. We identified each “high” quality item with a “star.” “Comparability” had a maximum of two “stars,” and the rest of the items had a maximum of one “star” each [21]. Studies with six or more stars were considered high quality [10].
Results
Study selection
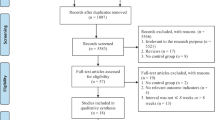
A total of 1278 records were selected by searching PubMed, Embase, the Cochrane Library, and ClinicalTrials.gov databases, and 268 duplicates were eliminated. After the titles and abstracts were screened, 983 irrelevant records were excluded. Further exclusion was achieved by scanning the full texts of the remaining 27 articles. Then, 20 articles were excluded, including 2 meta-analyses, 2 reviews, 4 articles with undesirable fraction doses or tumor clinical stage, 2 articles with incomplete and duplicated data, and 10 articles with unsatisfactory interval times between radiation and surgery. Eventually, we included 7 appropriate studies [11, 13,14,15, 18, 22, 23] involving a total of 4973 patients. The flow diagram is shown in Fig. 1.
Characteristics of the included studies
Five of these studies [11, 13, 14, 18, 23] were RCTs, and the other two studies [15, 22] were not RCTs. According to the Cochrane bias assessment (Figs. 2 and 3), four of the five RCTs mentioned randomization and reported the generation of randomized sequences. The performance bias could not be assessed because it was too difficult to keep the radiotherapy regimens a secret between the participants and researchers. Blinding was adopted in only one study. The quality of the two non-RCTs was evaluated by the NOS. As shown in Table 1, the total number of stars of the two non-RCTs was no less than eight each. The basic information on the eligible studies included in our meta-analysis is listed in Table 2.
Primary endpoint
Overall survival
Five studies [11, 13,14,15, 23] reported the overall survival (OS). Of these five, four [11, 13, 14, 23] were RCTs that directly provided HR values for OS. Four articles [11, 13, 14, 23] reported the results of two RCTs at different follow-up times, so we extracted long-term follow-up results [13, 23]. We excluded the study conducted by Chung et al. [15] because we could not extract effective statistics from the step-like survival curve provided by the authors (the 95% CI of the HR was too broad to believe). The quality of pooled statistics was thus higher after this choice. Ultimately, two studies [13, 23], with a total of 655 patients, were analyzed. Significant heterogeneity was observed (I2 = 84%, P = 0.01); therefore, the random effects model was used. There were no statistically significant differences in OS between the PSRT with delayed surgery group and the PLRT group (pooled HR = 1.30, 95% CI 0.58–2.89, P = 0.52; Fig. 4). A subgroup analysis was performed to reduce some heterogeneity.
The subgroup analysis found that patients who underwent PLRT had better OS than those who underwent PSRT without pre/postoperative chemotherapy (HR = 2.05, 95% CI 1.13–3.72, P = 0.02). Moreover, patients who underwent PSRT with pre/postoperative chemotherapy had a similar OS to that found in patients in the PLRT group (pooled HR = 0.90, 95% CI 0.70–1.15, P = 0.41). The details are shown in Fig. 4.
Secondary endpoint
Disease-free survival
Five studies [11, 13,14,15, 23] reported the outcome of disease-free survival (DFS). We excluded the study conducted by Chung et al. [15] because statistics extracted from the step-like survival curve provided by the authors were unreliable (the 95% CI of HR was too broad to believe). Four of these five articles [11, 13, 14, 23] reported the results of two RCTs at different follow-up times, and we therefore extracted long-term follow-up results [13, 23]. Ultimately, two studies [13, 23], involving a total of 655 patients, were included. One of the articles directly provided the HR of DFS. We extracted the statistics of the other article [13] from the given survival curve based on the method described in Tierney et al. [19] using Engauge Digitizer software. A random effects model was used for high heterogeneity (I2 = 52%). No significant differences in DFS were found between the PSRT group and the PLRT group (pooled HR = 1.10, 95% CI 0.73–1.66, P = 0.64; Fig. 5).
The subgroup analysis showed that there were no significant differences between either the PSRT with or without adjuvant chemotherapy subgroup and the PLRT group (HR = 0.95, 95% CI 0.75–1.20, P = 0.67 vs HR = 1.48, 95% CI 0.85–2.57, P = 0.16, respectively).
Pathological complete remission
Five studies [11, 14, 15, 18, 22] were eligible for the analysis of pathological complete remission (pCR). Of these, three [11, 14, 18] were RCTs and the rest [15, 22] were retrospective cohort studies. The random effects model was used to pool the statistics (I2 = 80%, P < 0.01). There was no significant difference in pCR between the two groups (RR = 0.74, 95% CI 0.37–1.48, P = 0.39; Fig. 6). The results remained unchanged after sensitivity analysis.
The subgroup analysis showed that pCR was higher in the PLRT group than in the PSRT group without additional chemotherapy group (RR = 0.42, 95% CI 0.30–0.60, P < 0.01), whereas pCR showed an increasing trend in the PSRT with chemotherapy group (RR = 1.37, 95% CI 0.90–2.09, P = 0.14). Moreover, the subgroup analysis sharply decreased heterogeneity, and the I2 values in each subgroup were all 0%.
Early postoperative complications
Three studies [11, 14, 18], with a total of 815 patients, were included in the study of postoperative complications (PCs). No heterogeneity was observed (I2 = 0%, P = 0.74), and a fixed effects model was used. The incidence of PCs was similar in the two groups (RR = 1.21, 95% CI 0.93–1.57, P = 0.16; Fig. 7).
The subgroup analysis revealed no significant differences between the two PSRT subgroups (RR = 0.89, 95% CI 0.36–2.21, P = 0.80; RR = 1.25, 95% CI 0.95–1.65; P = 0.11, respectively).
Grade 3/4 toxicity
Three trials [11, 15, 18], with a total of 783 patients, reported treatment-related grade 3/4 toxicity. As shown in Fig. 8, treatment-related grade 3/4 toxicity was similar between the PSRT group and the PLRT group (RR = 0.78, 95% CI 0.24–2.49, P = 0.68). The random effects model was employed due to high heterogeneity (I2 = 87%, P < 0.01). The results changed after the sensitivity analysis; therefore, a further subgroup analysis was needed.
Intragroup heterogeneity decreased through the subgroup analysis (I2 = 39%, P = 0.20). As shown in Fig. 8, the PSRT without pre/postoperative chemotherapy group had a lower treatment-related grade 3/4 toxicity events than the PLRT group (RR = 0.19, 95% CI 0.08–0.48, P < 0.01). Patients who were treated with PSRT plus chemotherapy had similar treatment-related grade 3/4 toxicity to those treated with PLRT (RR = 1.31 95% CI 0.75–2.27, P = 0.34).
Local recurrence
Two articles [13, 15], with a total of 212 participants, were included in our meta-analysis. Heterogeneity was not present (I2 = 0, P = 0.53); therefore, a fixed effects model was employed. Pooled statistics showed a lack of a significant difference between the PSRT group and the PLRT group (RR = 1.27, 95% CI 0.39–4.15, P = 0.70; Fig. 9). Sensitivity analysis proved the synthesis results were robust.
The subgroup analysis showed no significant differences in the two subgroups (RR = 1.06, 95% CI 0.28–4.07, P = 0.93 vs RR = 2.79, 95% CI 0.18–42.42, P = 0.46, respectively).
Distant metastasis
Four articles [11, 13, 15, 23], with a total of 727 patients, were eligible for the distant metastasis (DM) analysis. Two [11, 23] of the four articles reported the results of an RCTs at different follow-up times, so we extracted long-term follow-up results [23]. Ultimately, three articles were analyzed. Considering the low heterogeneity, a fixed effects model was employed, as shown in Fig. 10 (I2 = 37%, P = 0.21). No significant differences were observed between the two groups (RR = 1.06, 95% CI 0.85–1.33, P = 0.58). The results remained unchanged after sensitivity analysis.
The subgroup analysis showed no significant differences in the two subgroups (RR = 1.39, 95% CI 0.79–2.43, P = 0.25 vs RR = 1.01, 95% CI 0.79–1.28, P = 0.94, respectively).
Discussion
Main results: Our meta-analysis revealed no statistically significant differences in terms of OS, DFS, pCR, treatment-related grade 3/4 toxicity, PCs, local recurrence (LR), or DM. The two subgroups were then divided based on whether additional chemotherapy was available in the PSRT arm. The subgroup analysis revealed no significant differences with regard to DFS, DM, PCs, or LR. The subgroup analysis revealed that compared with the long-course radiotherapy group, the preoperative short-course radiotherapy without adjuvant chemotherapy group had not only a lower treatment-related grade 3/4 toxicity (RR = 0.19, 95% CI 0.08–0.48, P < 0.01) but also a significantly lower OS and pCR (HR = 2.05, 95% CI 1.13–3.72, P = 0.02; RR = 0.42, 95% CI 0.30–0.60, P < 0.01, respectively). Interestingly, pCR showed an increasing trend in the PSRT with adjuvant chemotherapy group, but the difference was not significant (RR = 1.37, 95% CI 0.90–2.09, P = 0.14). Furthermore, patients treated with PLRT suffered from more treatment-related grade 3/4 toxicity than those treated with PSRT without chemotherapy (RR = 0.19, 95% CI 0.08–0.48, P < 0.01). In summary, our meta-analysis found that PSRT with delayed surgery had similar efficacy and side effects compared with PLRT and that adding additional chemotherapy to the PSRT group resulted in few advantages over the long-course radiotherapy group.
Although the most recent NCCN and ESMO guidelines both recommend PSRT and PLRT as standard treatment regimens for locally advanced rectal cancer, the oncology radiologists’ preferences for radiation vary significantly among different countries. In the USA, PSRT is rarely performed, and no more than 5% of locally advanced rectal cancer patients accepted PSRT compared with PLRT [24, 25] due to the lack of economic incentives, unfamiliarity with short discharge techniques, and uncertainty about the efficacy and side effects of such treatment [26]. Additionally, PSRT accounts for only 15% of radiation therapy methods in England [27]. For a large number of patients, PLRT is the first option. PSRT still has a low status in Europe, and patients receiving PSRT account for less than 20% of patients receiving PLRT [28, 29]. Therefore, the role of PSRT in the application of cancer treatment must be further elucidated.
Moreover, neither the NCCN guidelines nor the ESMO guidelines clearly provide an optimal time interval for the gap between the end of PSRT and surgery. There are two common time intervals at which short-course radiotherapy and surgery are performed: short-course radiotherapy followed immediately by surgery within 10 days (this method is more commonly practiced in Europe) and short-course radiotherapy followed by delayed surgery (at least 4 weeks after the last radiotherapy is completed).
One study reported that there was no survival advantage in patients treated with surgery within 2 weeks in the PSRT arm and that a 2-week time interval did not achieve a desirable R0 resection rate [30]. Some RCTs have shown that compared with PSRT followed by immediate surgery (within 10 days) PSRT followed by delayed surgery (at a less than a 4-week time interval) significantly improved tumor pCR, downstaging, and the R0 resection rate, and resulted in fewer PCs [16, 31]. The Stockholm III Trial [32] found that PSRT with delayed surgery (4 to 6 weeks after PSRT) resulted in greater tumor downstaging than PSRT with immediate surgery. A meta-analysis conducted by Wu et al. [10] showed conclusions consistent with these previous findings: PSRT followed by surgery (at least 4 weeks later) was superior to PSRT followed by immediate surgery in terms of pCR, downstaging, the R0 resection rate, and PCs. Disappointingly, however, no conclusive evidence has been presented to demonstrate that delaying surgery can improve survival.
Another study demonstrated that a delaying surgery by at least 6 weeks achieved maximal tumor regression and that the tumors in the PSRT group continued to shrink over the following 1 to 2 weeks [33]. Furthermore, the tumor regression grade was more significant when the time interval to surgery was prolonged to more than 8 weeks in the PSRT group [34]. Delayed surgery not only potentially provides sufficient time for tumor shrinkage but also allows opportunities for systemic therapy. A research conducted by Pettersson et al. [35] showed that performing surgery at an interval of 4–8 weeks in the PSRT group resulted in similar PCs compared with PLRT. Our study did not find advantages in the PSRT group with regard to pCR, and the results were not reversed even in the PSRT with chemotherapy subgroups. One possible reason for this finding was that the time interval between the procedures was not long enough, and the tumor response thus did not reach its peak. If a sufficient time interval is provided, the tumors in the PSRT group may be reduced to a minimum, which may increase pCR and the possibility of R0 resection and potentially improved local control.
Previous studies have supported the notion that PSRT with immediate surgery is as effective as PLRT in terms of efficacy and safety [36,37,38], whereas the results of comparison of PSRT with delayed surgery and traditional PLRT are still controversial. Two articles [13, 14] reported the results of the same randomized study with different follow-up times; both observed that PLRT resulted in longer DFS than the PSRT with delayed surgery group. Nevertheless, a retrospective cohort study showed the opposite result [12]. According to another study, 3-year OS was higher in patients who received PSRT with delayed surgery than in those who received conventional PLRT (73% vs 65%, respectively, P < 0.05) [11]. However, most of the studies have found that PSRT with delayed surgery is as effective as PLRT in terms of OS [12, 14,15,16, 39]. Our meta-analysis focused on the PSRT in which surgery was completed at least 4 weeks later versus conventional long-course chemoradiotherapy. Pooled statistics showed no significant differences between the two arms regarding survival.
Interestingly, our subgroup analysis found that additional chemotherapy cannot significantly improve OS in the PSRT with delayed surgery group (Fig. 4), and long-course radiotherapy concurrent with chemotherapy based on 5-Fu leads to higher OS and pCR compared with no additional chemotherapy in the PSRT with delayed surgery group. Unfortunately, the improvement of the OS reported in the PLRT group came at the cost of increased treatment-related grade 3/4 toxicity. In contrast, a single-arm retrospective study performed in the UK showed that PSRT plus adjuvant chemotherapy improved OS only in patients with two or more risk factors [40]. This observation may imply that chemotherapy provides advantages only in selected patients; otherwise, patients may suffer more from overtreatment.
A Cochrane systematic review demonstrated that preoperative chemoradiotherapy only improved local control, without providing a survival benefit [41]. In our subgroup analysis, we did not find that additional chemotherapy in the PSRT arm provides advantages with regard to LR but we did observe that OS was lower in the PSRT without chemotherapy subgroup. We believe that additional adjuvant chemotherapy is, theoretically, more conducive to the elimination of micrometastatic disease [25], but our meta-analysis does not indicate that the DM rate is lower in clinical practice.
Two studies showed that adjuvant chemotherapy following preoperative neoadjuvant therapy provided no survival benefit over preoperative neoadjuvant therapy alone [42, 43], while another study showed that adjuvant chemotherapy increased OS [44]. According to another study, adding consolidation chemotherapy added to postoperative therapy provided no benefit to OS in patients treated with PSRT who underwent an operation after 3 to 7 days [45]. This finding may also imply that adding additional chemotherapy before surgery may improve the survival rate more than adding it after surgery. Therefore, the optimal time to add chemotherapy to patients’ treatment plan remains unclear, and the time interval between the completion of short-course radiation and surgery may play an important role in survival. More RCTs are needed to illustrate whether the addition of chemotherapy to the PSRT with delayed surgery regimen is favorable. We expect the ongoing RAPIDO trial (NCT: 01558921) [46] in Sweden and a phase III ongoing trial in China (NCT: 02533271) [47] to clarify this issue.
The limitations of the current study should not be neglected, since five RCTs and two non-RCTs were included in our meta-analysis. First, the Cochrane risk of bias assessment showed that all RCTs exhibited some potential risk of bias (details shown in Fig. 2). Second, clinical heterogeneity was present in the included studies. Patients in most of the eligible studies were in clinical stage II–III, and the location of the tumor varied among patients. Third, the types of specific chemotherapy drugs were different across studies. Additionally, follow-up times and methods varied among different studies. For example, the results were tracked by telephone follow-up in Xiao’s [18] study, and two [13, 14] articles came from different stages of the same RCT (NCT: 00597311). Finally, the operative methods and quality were different in each study.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Ma B, Gao P, Song Y, Huang X, Wang H, Xu Q, Zhao S, Wang Z (2018) Short-course radiotherapy in neoadjuvant treatment for rectal cancer: a systematic review and meta-analysis. Clin Colorectal Cancer 17(4):320–330.e325. https://doi.org/10.1016/j.clcc.2018.07.014
Abraha I, Aristei C, Palumbo I, Lupattelli M, Trastulli S, Cirocchi R, De Florio R, Valentini V (2018) Preoperative radiotherapy and curative surgery for the management of localised rectal carcinoma. Cochrane Database Syst Rev 10:Cd002102. https://doi.org/10.1002/14651858.CD002102.pub3
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, Becker H, Raab HR, Villanueva MT, Witzigmann H, Wittekind C, Beissbarth T et al (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol 30(16):1926–1933. https://doi.org/10.1200/jco.2011.40.1836
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, Quirke P, Couture J, de Metz C, Myint AS, Bessell E, Griffiths G, Thompson LC, Parmar M (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet (London, England) 373(9666):811–820. https://doi.org/10.1016/s0140-6736(09)60484-0
Wang X, Zheng B, Lu X, Bai R, Feng L, Wang Q, Zhao Y, He S (2018) Preoperative short-course radiotherapy and long-course radiochemotherapy for locally advanced rectal cancer: meta-analysis with trial sequential analysis of long-term survival data. PLoS One 13(7):e0200142. https://doi.org/10.1371/journal.pone.0200142
National Comprehensive Cancer Network. Rectal Cancer (version 3.2018). https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf. Accessed August 7, 2018.
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rodel C, Cervantes A, Arnold D, Committee EG (2017) Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 28(suppl_4):iv22–iv40. https://doi.org/10.1093/annonc/mdx224
Liu SX, Zhou ZR, Chen LX, Yang YJ, Hu ZD, Zhang TS (2015) Short-course versus long-course preoperative radiotherapy plus delayed surgery in the treatment of rectal cancer: a meta-analysis. Asian Pac J Cancer Prev 16(14):5755–5762. https://doi.org/10.7314/APJCP.2015.16.14.5755
Wu H, Fang C, Huang L, Fan C, Wang C, Yang L, Li Y, Zhou Z (2018) Short-course radiotherapy with immediate or delayed surgery in rectal cancer: a meta-analysis. Int J Surg (London, England) 56:195–202. https://doi.org/10.1016/j.ijsu.2018.05.031
Bujko K, Wyrwicz L, Rutkowski A, Malinowska M, Pietrzak L, Krynski J, Michalski W, Oledzki J, Kusnierz J, Zajac L, Bednarczyk M, Szczepkowski M et al (2016) Long-course oxaliplatin-based preoperative chemoradiation versus 5 x 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: results of a randomized phase III study. Ann Oncol 27(5):834–842. https://doi.org/10.1093/annonc/mdw062
Markovina S, Youssef F, Roy A, Aggarwal S, Khwaja S, DeWees T, Tan B, Hunt S, Myerson RJ, Chang DT, Parikh PJ, Olsen JR (2017) Improved metastasis- and disease-free survival with preoperative sequential short-course radiation therapy and FOLFOX chemotherapy for rectal cancer compared with Neoadjuvant long-course chemoradiotherapy: results of a matched pair analysis. Int J Radiat Oncol Biol Phys 99(2):417–426. https://doi.org/10.1016/j.ijrobp.2017.05.048
Kairevičė L, Latkauskas T, Tamelis A, Petrauskas A, Pauzas H, Zvirblis T, Jarusevicius L, Saladzinskas Z, Pavalkis D, Janciauskiene R (2017) Preoperative long-course chemoradiotherapy plus adjuvant chemotherapy versus short-course radiotherapy without adjuvant chemotherapy both with delayed surgery for stage II-III resectable rectal cancer: 5-year survival data of a randomized controlled trial. Medicina (Kaunas, Lithuania) 53(3):150–158. https://doi.org/10.1016/j.medici.2017.05.006
Latkauskas T, Pauzas H, Kairevice L, Petrauskas A, Saladzinskas Z, Janciauskiene R, Gudaityte J, Lizdenis P, Svagzdys S, Tamelis A, Pavalkis D (2016) Preoperative conventional chemoradiotherapy versus short-course radiotherapy with delayed surgery for rectal cancer: results of a randomized controlled trial. BMC Cancer 16(1):927. https://doi.org/10.1186/s12885-016-2959-9
Chung MJ, Chung WK, Kim DW, Lee SH, Jeong SK, Hwang JK, Jeong CS (2016) Preoperative short vs. long course chemoradiation with delayed surgery for rectal cancer patients. Radiother Oncol 119:S602. https://doi.org/10.1016/s0167-8140(16)32530-0
Erlandsson J, Holm T, Pettersson D, Berglund A, Cedermark B, Radu C, Johansson H, Machado M, Hjern F, Hallbook O, Syk I, Glimelius B et al (2017) Optimal fractionation of preoperative radiotherapy and timing to surgery for rectal cancer (Stockholm III): a multicentre, randomised, non-blinded, phase 3, non-inferiority trial. Lancet Oncol 18(3):336–346. https://doi.org/10.1016/s1470-2045(17)30086-4
Latkauskas T, Pauzas H, Gineikiene I, Janciauskiene R, Juozaityte E, Saladzinskas Z, Tamelis A, Pavalkis D (2012) Initial results of a randomized controlled trial comparing clinical and pathological downstaging of rectal cancer after preoperative short-course radiotherapy or long-term chemoradiotherapy, both with delayed surgery. Colorect Dis 14(3):294–298. https://doi.org/10.1111/j.1463-1318.2011.02815.x
Xiao J, Teng WH, Liu S, Wei C, Liu WJ, Chen S, Zang WD (2018) Short-course radiotherapy with delayed surgery versus conventional chemoradiotherapy: comparison of short-term outcomes in patients with t3-4 rectal cancer. Int J Clin Exp Med 11(11):12149–12156
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. https://doi.org/10.1186/1745-6215-8-16
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 343:d5928. https://doi.org/10.1136/bmj.d5928
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Hoendervangers S, Couwenberg AM, Intven MPW, van Grevenstein WMU, Verkooijen HM (2018) Comparison of pathological complete response rates after neoadjuvant short-course radiotherapy or chemoradiation followed by delayed surgery in locally advanced rectal cancer. Eur J Surg Oncol 44(7):1013–1017. https://doi.org/10.1016/j.ejso.2018.03.014
Ciseł B, Pietrzak L, Michalski W, Wyrwicz L, Rutkowski A, Kosakowska E, Cencelewicz A, Spałek M, Polkowski W, Jankiewicz M, Styliński R, Bębenek M et al (2019) Long-course preoperative chemoradiation vs. 5 x 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: long-term results of the randomized Polish II study. Ann Oncol. https://doi.org/10.1093/annonc/mdz186
Chapman BC, Goodman K, Hosokawa P, Gleisner A, Cowan ML, Birnbaum E, Vogel JD (2019) Improved survival in rectal cancer patients who are treated with long-course versus short-course neoadjuvant radiotherapy: a propensity-matched analysis of the NCDB. J Surg Oncol 119(4):518–531. https://doi.org/10.1002/jso.25355
Narang AK, Meyer J (2018) Neoadjuvant short-course radiation therapy for rectal cancer: trends and controversies. Curr Oncol Rep 20(9):68. https://doi.org/10.1007/s11912-018-0714-x
Kusano AS, Voss JC, Bremjit PJ, Fichera A, Koh W, Kim EY, Apisarnthanarax S (2014) Preoperative short course radiation for locally advanced rectal cancer: a national opinion survey. Int J Radiat Oncol Biol Phys 90(1):S595
Morris EJA, Finan PJ, Spencer K, Geh I, Crellin A, Quirke P, Thomas JD, Lawton S, Adams R, Sebag-Montefiore D (2016) Wide variation in the use of radiotherapy in the management of surgically treated rectal cancer across the English National Health Service. Clin Oncol 28(8):522–531. https://doi.org/10.1016/j.clon.2016.02.002
Lutz MP, Zalcberg JR, Glynne-Jones R, Ruers T, Ducreux M, Arnold D, Aust D, Brown G, Bujko K, Cunningham C, Evrard S, Folprecht G et al (2016) Second St. Gallen European Organisation for Research and Treatment of Cancer Gastrointestinal Cancer Conference: consensus recommendations on controversial issues in the primary treatment of rectal cancer. Eur J Cancer (Oxford, England : 1990) 63:11–24. https://doi.org/10.1016/j.ejca.2016.04.010
Saralegui Y, Enriquez-Navascues JM, Ciria JP, Osorio M, Lacasta A, Elorza G, Garmendia M, Placer C (2017) Results of short term radiotherapy followed by radical surgery for rectal cancer: a long-term unicenter observational study. Cirugia esp 95(5):268–275. https://doi.org/10.1016/j.ciresp.2017.04.008
Tian X, Zhang X, Han C, Zhou B, Jiang K, Zhang Q, Chen Y (2015) Observation on the effect of preoperative radiotherapy on the local advanced middle and low rectal cancer. Cancer Res Clinic 27(12):810–813. https://doi.org/10.3760/cma.j.issn.1006-9801.2015.12.005
Pach R, Kulig J, Richter P, Gach T, Szura M, Kowalska T (2012) Randomized clinical trial on preoperative radiotherapy 25 Gy in rectal cancer--treatment results at 5-year follow-up. Langenbeck's Arch Surg 397(5):801–807. https://doi.org/10.1007/s00423-011-0890-8
Pettersson D, Lorinc E, Holm T, Iversen H, Cedermark B, Glimelius B, Martling A (2015) Tumour regression in the randomized Stockholm III Trial of radiotherapy regimens for rectal cancer. Br J Surg 102 (8):972–978; discussion 978. doi:https://doi.org/10.1002/bjs.9811
Lee SW, Lee JH, Lee IK, Oh ST, Kim DY, Kim TH, Oh JH, Baek JY, Chang HJ, Park HC, Kim HC, Chie EK, Nam TK, Jang HS (2018) The impact of surgical timing on pathologic tumor response after short course and long course preoperative chemoradiation for locally advanced rectal adenocarcinoma. Cancer Res Treat 50(3):1039–1050. https://doi.org/10.4143/crt.2017.252
Rega D, Pecori B, Scala D, Avallone A, Pace U, Petrillo A, Aloj L, Tatangelo F, Delrio P (2016) Evaluation of tumor response after short-course radiotherapy and delayed surgery for rectal cancer. PLoS One 11(8). https://doi.org/10.1371/journal.pone.0160732
Pettersson D, Cedermark B, Holm T, Radu C, Pahlman L, Glimelius B, Martling A (2010) Interim analysis of the Stockholm III trial of preoperative radiotherapy regimens for rectal cancer. Br J Surg 97(4):580–587. https://doi.org/10.1002/bjs.6914
Ansari N, Solomon MJ, Fisher RJ, Mackay J, Burmeister B, Ackland S, Heriot A, Joseph D, McLachlan SA, McClure B, Ngan SY (2017) Acute adverse events and postoperative complications in a randomized trial of preoperative short-course radiotherapy versus long-course chemoradiotherapy for T3 adenocarcinoma of the rectum: Trans-Tasman Radiation Oncology Group Trial (TROG 01.04). Ann Surg 265(5):882–888. https://doi.org/10.1097/sla.0000000000001987
McLachlan SA, Fisher RJ, Zalcberg J, Solomon M, Burmeister B, Goldstein D, Leong T, Ackland SP, McKendrick J, McClure B, Mackay J, Ngan SY (2016) The impact on health-related quality of life in the first 12 months: a randomised comparison of preoperative short-course radiation versus long-course chemoradiation for T3 rectal cancer (Trans-Tasman Radiation Oncology Group Trial 01.04). Eur J Cancer (Oxford, England : 1990) 55:15–26. https://doi.org/10.1016/j.ejca.2015.10.060
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski W, Bebenek M, Kryj M (2006) Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg 93(10):1215–1223. https://doi.org/10.1002/bjs.5506
Beppu N, Matsubara N, Noda M, Yamano T, Kakuno A, Doi H, Kamikonya N, Kimura F, Yamanaka N, Yanagi H, Tomita N (2015) Short-course radiotherapy with delayed surgery versus conventional chemoradiotherapy: a comparison of the short- and long-term outcomes in patients with T3 rectal cancer. Surgery 158(1):225–235. https://doi.org/10.1016/j.surg.2015.03.014
Loree JM, Kennecke HF, Renouf DJ, Lim HJ, Vickers MM, Speers CH, Cheung WY (2016) Effect of adjuvant chemotherapy on stage II rectal cancer outcomes after preoperative short-course radiotherapy. Clin Colorectal Cancer 15(4):352–359.e351. https://doi.org/10.1016/j.clcc.2016.04.003
McCarthy K, Pearson K, Fulton R, Hewitt J (2012) Pre-operative chemoradiation for non-metastatic locally advanced rectal cancer. Cochrane Database Syst Rev 12. https://doi.org/10.1002/14651858.CD008368.pub2
Loree JM, Kennecke HF, Lee-Ying RM, Goodwin RA, Powell ED, Tang PA, Price Hiller JA, Vickers MM, Cheung WY (2018) Impact of postoperative adjuvant chemotherapy following long-course chemoradiotherapy in stage II rectal cancer. Am J Clin Oncol 41(7):643–648. https://doi.org/10.1097/coc.0000000000000342
Baird DLH, Denost Q, Simillis C, Pellino G, Rasheed S, Kontovounisios C, Tekkis PP, Rullier E (2017) The effect of adjuvant chemotherapy on survival and recurrence after curative rectal cancer surgery in patients who are histologically node negative after neoadjuvant chemoradiotherapy. Colorect Dis 19(11):980–986. https://doi.org/10.1111/codi.13714
Dossa F, Acuna SA, Rickles AS, Berho M, Wexner SD, Quereshy FA, Baxter NN, Chadi SA (2018) Association between adjuvant chemotherapy and overall survival in patients with rectal cancer and pathological complete response after neoadjuvant chemotherapy and resection. JAMA Oncol 4(7):930–937. https://doi.org/10.1001/jamaoncol.2017.5597
Ngan SY, Burmeister B, Fisher RJ, Solomon M, Goldstein D, Joseph D, Ackland SP, Schache D, McClure B, McLachlan SA, McKendrick J, Leong T et al (2012) Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group Trial 01.04. J Clin Oncol 30(31):3827–3833. https://doi.org/10.1200/JCO.2012.42.9597
Nilsson PJ, van Etten B, Hospers GA, Påhlman L, van de Velde CJ, Beets-Tan RG, Blomqvist L, Beukema JC, Kapiteijn E, Marijnen CA, Nagtegaal ID, Wiggers T, Glimelius B (2013) Short-course radiotherapy followed by neo-adjuvant chemotherapy in locally advanced rectal cancer--the RAPIDO trial. BMC Cancer 13:279. https://doi.org/10.1186/1471-2407-13-279
Tang Y, Jin J, Ling N, Ren H, Wang WH, Song YW, Liu YP, Wang SL, Fang H, Li YX (2015) Phase III study of short-term radiotherapy followed by neoadjuvant chemotherapy versus preoperative long-term chemoradiotherapy in locally advanced rectal cancer. Ann Oncol 26:ix70. https://doi.org/10.1093/annonc/mdv523.96
Acknowledgments
The authors would like to thank Yunnan Cancer Hospital.
Funding
This study received financial support from Kunming Medical University Cancer Radiation Therapy Technology Innovation Team Construction Project Funding and Funding for the “Ten Thousand Plan” Youth Talent Project in Yunnan Province.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All the authors have complied with all applicable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qiaoli, W., Yongping, H., Wei, X. et al. Preoperative short-course radiotherapy (5 × 5 Gy) with delayed surgery versus preoperative long-course radiotherapy for locally resectable rectal cancer: a meta-analysis. Int J Colorectal Dis 34, 2171–2183 (2019). https://doi.org/10.1007/s00384-019-03433-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03433-9