Abstract
Background and aim
Sessile serrated adenoma/polyps (SSAPs) are suspected to have a high malignant potential, although few reports have evaluated the incidence of carcinomas derived from SSAPs using the new classification for serrated polyps (SPs). The aim of study was to compare the frequency of cancer coexisting with the various SP subtypes including mixed polyps (MIXs) and conventional adenomas (CADs).
Methods
A total of 18,667 CADs were identified between April 2005 and December 2011, and 1858 SPs (re-classified as SSAP, hyperplastic polyp (HP), traditional serrated adenoma (TSA), or MIX) were removed via snare polypectomy, endoscopic mucosal resection, or endoscopic sub-mucosal dissection.
Results
Among 1160 HP lesions, 1 (0.1 %) coexisting sub-mucosal invasive carcinoma (T1) was detected. Among 430 SSAP lesions, 3 (0.7 %) high-grade dysplasia (HGD/Tis) and 1 (0.2 %) T1 were detected. All of the lesions were detected in the proximal colon, with a mean tumor diameter of 18 mm (SD 9 mm). Among 212 TSA lesions, 3 (1 %) HGD/Tis were detected but no T1 cancer. Among 56 MIX lesions, 9 (16 %) HGD/Tis and 1 (2 %) T1 cancers were detected, and among 18,677 CAD lesions, 964 (5 %) HGD/Tis and 166 (1 %) T1 cancers were identified.
Conclusions
Among the resected lesions that were detected during endoscopic examination, a smaller proportion (1 %) of SSAPs harbored HGD or coexisting cancer, compared to CAD or MIX lesions. Therefore, more attention should be paid to accurately identifying lesions endoscopically for intentional resection and the surveillance of each SP subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Based on the findings of previous studies, the World Health Organization developed and published new classifications for serrated polyps (SPs), which include sessile serrated adenoma/polyps (SSAPs), traditional serrated adenomas (TSAs), and hyperplastic polyps (HPs) [1]. However, it has been reported that the majority of colorectal cancers develop from conventional adenomas (CADs) such as tubular-adenomas and tubulovillous-adenomas, which are derived from the “adenoma-carcinoma sequence” [2]. In contrast, 15–20 % of cancers are thought to develop via the “serrated polyp pathway” [3–5]. HPs including metaplastic polyps were previously classified as non-neoplastic polyps, although reports published after 1994 recommended intentional resection is recommended for large HPs in the proximal colon, as atypical HPs or high-grade dysplasia (HGD) indicates carcinogenesis from hyperplastic polyposis [6–10]. A report by Torlakovic et al. in 2003 was the first to suggest that neoplastic lesions lead to SSAPs, as well as various other precancerous lesions that originate from the serrated polyp pathways with variations in hMLH1 and hMSH2 [11]. Later molecular biological assessments of SSAP showed that they carried BRAF variants and allowed other SPs and CADs to be distinguished from SSAP [12]. In addition, SSAP is involved in tumor growth and carcinogenesis and shows various genetic changes including CpG-island methylation, DNA-methylation, and microsatellite instability (MSI) [13, 14]. Given the relationship between SSAPs and the precancerous lesions of sporadic MSI-high colorectal cancer, the malignant potential of SSAPs has recently been revised to high [9, 15], although there is little data on other SSAPs especially mixed polyps (MIXs). Moreover, it is unclear when it is appropriate to completely remove SP lesions, and thus multidisciplinary strategies for surveillance should consider the malignancy grade for each sub-classification. With respect to SP surveillance, a meta-analysis of studies involving SP with synchronous colorectal advanced neoplasia (adenoma ≧10 mm, villous component, high-grade dysplasia, or colorectal cancer) reported associated the high-risk group of SPs. In the high-risk SP, lesions were reported that those were large (≧10 mm) and located proximally to the splenic flex [16–18].
In screening colonoscopy, the detection rate of early cancer with SSAPs is thought to be extremely low, compared to that of early cancer with CADs. In addition, there are few reports regarding the frequency of early cancer in a large population sample. This may be because previous studies had a significant selection bias, resulting in the frequency of SP-derived colorectal cancer being overestimated. It is also difficult to uniformly collect all pathological examination data [19], and no consensus has been reached regarding standardized SSAP diagnostic criteria. Therefore, this study was designed to compare the frequencies with which cancer arises from each SP subtype, as well as CAD, in a large population sample.
Materials and methods
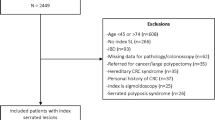
Between April 2005 and December 2011, our institution indicated endoscopic treatment for colorectal tumors with a >5 mm neoplastic lesion, regardless of whether it was diagnosed as classical HP via endoscopy as well as possible. Therefore, we searched our histopathologic specimen database for patients who underwent endoscopic treatment during the study period for the findings of key word which were “SP,” “HP,” “atypical HP,” “metaplastic polyp,” “atypical metaplastic polyp,” “serrated adenoma,” “SSAP,” or “mixed polyps.” Of the cases that were returned by this search, we only included those in which “snare polypectomy,” “endoscopic mucosal resection (EMR),” or “endoscopic sub-mucosal dissection (ESD)” were performed. Lesions that were extracted via “cold biopsy” or “hot biopsy” were excluded, as the biopsy material was unsatisfactory (it only included the mucosal surface) and might be not suitable for a pathological diagnosis of SSAP, HP, or MIX [20]. To eliminate any bias due to the diagnostic pathologists, a single specialized gastroenterology pathologist re-classified all of the relevant lesions in 2012 (Fig. 2).
Because it is rare for the case of remaining non-cancerous portions in advanced colorectal cancer, it is difficult to identify serrated carcinoma via pathology. Thus, derived cancers were those in which the cancerous and non-cancerous parts coexisted, and all target lesions in this study were extracted as early colorectal cancers that were sub-mucosal invasive carcinoma (T1) and including HGDs which were often diagnosed the intra-mucosal carcinoma (Tis) in Japanese pathological criteria.
All non-serrated CADs that were excised during the same period (and using the same methods) were also extracted from our hospital database and selected as the comparators for this study. In HGD and early cancer with CADs were all diagnosed by the same specialized pathologist, who distinguished early cancer with non-serrated CAD from Mixed SPs. All de novo cancers were excluded from the present study.
Analysis 1
During the study period (in which there was no standardized national pathology criteria), 1858 SP lesions were removed at our hospital and were diagnosed by multiple pathologists. These lesions were subsequently re-assessed by a single specialized gastroenterology pathologist, using the new pathological classifications, and the number of re-classified SPs and lesions were examined.
Analysis 2
The clinical characteristics and background factors associated with each sub-classified SP found in a whole lesion were reviewed, as were the non-serrated CAD lesions as appropriate comparators with SP.
Analysis 3
We compared the frequency and clinical characteristics of the HGD/Tis and T1 that were excised with each SP subtype or CAD.
Pathological classification of CAD and SP subtypes
CADs included tubular-adenoma, tubulovillous-adenoma, or villous adenoma with low-grade dysplasia. All serrated lesions were reviewed and re-classified as HP, SSAP, or TSA. Mixed polyps (MIX; previously known as mixed type serrated [21]) were defined as lesions with mixed characteristics, including SSAP and TSA; SSAP and CAD; TSA and CAD; or SSAP, TSA, and CAD (if they contained some serrated parts) [21]. Figure 1 shows 2 representative views of HP and SSAP. Typical pathological features of HPs include elongated straight crypts, epithelial serration limited to the upper half of the crypts, and basally located small nuclei without atypia (Fig. 1a), while those of SSAP are distorted crypts with dilated bases that result in an L-shape or inverted T-shape (Fig. 1b) [3]. Adding to noticed all of the findings crypt dilatation and irregular branching crypts. Typical pathological features of TSA are a villiform configuration with multiple ectopic crypts (villo-microglandular appearance) (Fig. 2).
Statistical analysis
Fisher’s exact test was used in order to compare the frequencies of cancer types coexisting with MIX vs SSAP or with MIX vs CAD. Two-sided p values of less than 0.05 were considered to be statistically significant.
Results
After the re-classification after the pathological review, 19 % (273/1430) of the HP lesions were re-classified as SSAPs, and 25 % (86/339) of the serrated adenomas were re-classified as SSAPs. However, 81 % (1156/1430) of the HP lesions and 73 % (249/339) of the serrated adenomas were not re-classified (Fig. 3).
Table 1 summarized the prevalence and clinical background factors of each SP subtype. The least common subtype was MIX (0.3 %). SP subtypes and CAD lesions were typically observed more frequently in male and in patients who were >60 years old. Table 2 lists the clinical data regarding the location, form, and size for each resected lesion. SSAPs and CADs were observed more frequently in the proximal colon (oral site from splenic flex), while HP, TSA, and MIX lesions were observed more frequently in the distal colon (sigmoid colon and rectum). Regarding their gross appearance, most SSAP and MIX lesions were flat, while most HP, TSA, and CAD lesions were protruding. MIXs were frequently larger than any other polyp subtype.
The frequency of early colorectal cancer with each SP subtype is shown in Tables 3 and 4. HGDs and early cancer were rarely found in HP and TSA (0.1 % for both). The frequency of T1 cancer with SSAP was 0.2 % (1/430), and 3 (0.7 %) were found in SSAP with HGD/Tis. All lesions were flat and located in the proximal colon, and 75 % of lesions were large (sized ≧10 mm). The mean of diameter was 18 mm (SD 9 mm). Among MIX lesions, 2 % (1/56) contained sub-mucosal invasive carcinoma and 16 % (9/56) contained intra-mucosal carcinoma (HGD); 60 % of the MIX lesions were distal, and they had a mean diameter of 18 mm (SD 14 mm). In contrast, the frequency of HGD or early cancer with CAD was 6 % (1131/18,667). CAD with HGD/Tis was found in 5 % of lesions (964/18,667) and CAD with sub-mucosal invasive cancer was found in 1 % of lesions (166/18,667). When the frequency of early cancer including HGD was compared between SP subtypes using Fisher’s exact test, it was found that a significantly higher proportion of MIXs contained cancer than CADs (p = 0.0002), while cancer was significantly rarer in SSAP than in CAD (Table 3).
Discussion
There are two methods to evaluate malignant potential. One of these involves the analysis of genetic changes (e.g., MSI) and their relationship with the cancer’s speed of progression. The second involves the assessment of the cancerous rate, based on the frequency of cancer arising from SSAP.
The former method takes into consideration the serrated pathway with BRAF or KRAS. BRAF is implicated in the first stage of cytological dysplasia in SSAP, while CpG-island methylation phenotypes are implicated in the intermediate stages. Unfortunately, the cancers that develop from these pathways are reported to have a high likelihood of being MSI-high cancers. In contrast, TSA cancers associated with KRAS are reported to have low levels of methylation and MSI [4, 5, 22]. SSAP can appear as a large HP when examined endoscopically, although serrated adenoma with HGD or atypical and classical HPs can be distinguished pathologically. However, the gross appearance of large HPs is similar to that of SSAP and classical HPs [20], and there has been little awareness of the need to distinguish between these lesions in order to guide appropriate clinical treatment. It has now been reported though that SSAPs are precursor lesions of sporadic MSI-high cancer [7, 11, 13, 14], and SSAPs are now considered highly malignant precursor lesions. Therefore, it is necessary to discriminate between SSAPs and large HPs during endoscopic examination.
In addition to direct observation, the rate of cancer coexisting with each SP subtype might assist in endoscopic diagnosis, for developing an appropriate treatment strategy, and as a method of surveillance. There is high reported frequency of cancer derived from SP, although the inter-facility differences are large [15, 23, 24]. A likely explanation for this is that it is difficult to obtain a unified consensus regarding the frequency of cancer development, given the changing pathologic diagnostic criteria for SSAPs and the small study populations that may have introduced selection bias. In addition, several reports did not classify SPs into the four subtypes, and a number of previous studies reported a high frequency of serrated adenoma, including large HP, HGD, SSAP, MIX, and occasionally TSA.
Regarding the re-classification of lesions after pathologic diagnosis, the reported rates of HP revision to SSAP range from 8 to 18 % [11, 12]. In the present study, we also found that 19 % of lesions were revised from HP to SSAP. Furthermore, 25 % of lesions that were originally diagnosed as serrated adenomas were later re-classified as SSAPs. Thus, close attention should be paid to the pathologic evaluation criteria, the frequency of the lesions, and the development of cancer, when considering the four new SP subtypes.
Regarding the prevalence of non-cancerous lesions, among 1479 patients who were evaluated using the SSAP diagnostic criteria, Carr et al. reported that 65 % of lesions were CAD, 30 % were HP, 3.9 % were SSAP, 0.7 % were TSA, and 0.7 % were MIX [25]. With the exception of HP, their findings are similar to those of the present study. Regarding the clinical characteristics of the SP subtypes, distal lesions were common in cases with HP, TSA, and MIX lesions, although proximal flat lesions were common for SSAPs; similar findings have been reported previously [12, 26]. However, with respect to tumor diameter, histopathology revealed that many lesions sized <10 mm were re-classified as SSAPs. In the study, prevalence of SPs was described risk factors with analysis synchronous lesions [16, 17, 27, 28]; accordingly, large (≥10 mm) SP lesions or those located in the proximal colon were considered to be risk factors for the development of colorectal cancer, and these cases therefore require more frequent surveillance. The HGDs and early cancers with SSAP in this study were found most commonly in large and proximal SPs.
Regarding the frequency of concurrent cancer, only a few previous studies had a large sample size, although a 2010 study by Richard et al. [29] revealed that 2.1 % of 2416 sessile serrated adenoma specimens contained HGD, and 1.0 % were adenocarcinomas arising from within a sessile serrated adenoma. Our findings were similar, although not all lesions that we detected were excised. Therefore, it is impossible for us to calculate the exact frequency of concurrent cancer, and this is a possible limitation of the present study. However, during the study period, the treatment guidelines at our hospital gave priority to excising as much of the lesion as possible, except in cases with multiple small lesions in the sigmoid colon or rectum. Thus, snare polypectomy was performed in cases with lesions <10 mm, while EMR was performed for larger lesions, rather than forceps biopsy alone. Therefore, it is possible that our estimation is close to the actual number of cases. A prospective study, in which all detected colorectal polyps are resected, might reveal a lower frequency of lesions with coexisting cancer. We also found that HGDs and early cancer with HP and TSA were rare, and this needs to be confirmed in a future study. It was also notable that the frequency of HGD and invasive carcinoma with SSAP (1 %) was significantly lower than that of CAD (6 %) or MIX (18 %). Furthermore, the frequency of intra-mucosal cancer (HGD) with MIX was higher than that of other SPs and CAD. Almost all HGD and invasive carcinoma with SPs were of a large size (≧10 mm), and all carcinoma with SSAP were found in the proximal colon, while most carcinomas with MIX were found in the distal colon. Holme et al. made the interesting observation that large SPs located on the left side of the colon frequently do not progress to colorectal cancer [16], and these lesions may actually have been large HPs. We also found some large SPs in the left colon, especially malignant MIX variants, but those were sometimes incorrectly identified during endoscopy as other neoplasms including adenoma. Genomic analysis will be needed to distinguish between MIX and SSAP with cytological dysplasia. Based on our findings and those of previous studies, we hypothesize that the cancerous rate from SSAP is lower than from CAD or MIX, but the former tumors grow more quickly. We suggest that MIX should be subdivided based on whether it includes CAD, as MIX lesions with CAD may behave more like pure CAD, except that they follow a more complex malignant pathway, especially MIX with not including CAD in proximal colon may be having malignant potential like SSAP such as having cytological dysplasia.
Several studies have suggested that interval cancer may actually be SSAP-derived carcinoma, because sporadic MSI-high precancerous lesions quickly progress to progressive cancer [28, 30]. Unfortunately, it remains difficult to pathologically determine whether an advanced cancer is of the serrated type, and we are therefore not able to clearly describe the malignant potential of SSAPs, given the low frequency of cancers coexisting with this lesion.
Our findings suggest that clinical data obtained via endoscopic examination that we suggest can be used to more clearly discriminate between SSAP, MIX lesions, and classical HPs. Furthermore, it is necessary to establish endoscopic treatment and surveillance strategies for both early stage colorectal cancer from SP subtypes and high-grade atypical neoplastic lesions. Our findings could help establish indications for the intentional treatment of each SP subtype.
References
Snover DC, Ahnen DJ, Burt RW et al (2010) Serrated polyps of the colon and rectum and serrated polyposis. World Health Organisation classification of tumors: tumors of the colon and rectum. 160–165
Vogelstein B, Fearon ER, Hamilton SR et al (1988) Genetic alterations during colorectal-tumor development. N Engl J Med 319:525–532
Christopher SH, Francis AF, Shi Y et al (2011) The clinical significance of serrated polyps. Am J Gastroenterol 106:229–240
Massimo P, Andrea R, Vittorio C et al (2012) Genetic and epigenetic events multiple pathways in colorectal cancer progression. Pathol Res Int Article ID509348; 11pages
O’Brien JM (2007) Hyperplastic and serrated polyps of the colorectum. Gastroenterol Clin N Am 36:947–968
Andrew SW, Michael EG, Franz F (1994) Multiple large hyperplastic polyps of the colon coincident with adenocarcinoma. Am J Gastroenterol 89:123–125
Torlakovic E, Snover DC (1996) Serrated adenomatous polyposis in humans. Gastroenterology 110:748–755
Carlos AR, Edgar J (1996) Flat serrated adenoma of the colorectal mucosa. Jpn J Cancer Res 87:305–309
Iino H, Jass JR, Simms LA et al (1999) DNA microsatellite instability in hyperplastic polyps, serrated adenoma, and mixed polyps: a mild mutator pathway for colorectal cancer? J Clin Pathol 52:5–9
Khawaja A, John JS, Indru TK et al (2000) Hyperplastic polyps: “more than meets the eye”? Dis Colon Rectum 43:1309–1313
Torlakovic E, Skovlund E, Snover DC et al (2003) Morphological reappraisal of serrated colorectal polyps. Am J Surg Pathol 27:65–81
Higuchi T, Sugihara K, Jass JR (2005) Demographic and pathological characteristics of serrated polyps of colorectum. Histopathology 47:32–40
Kambara T, Simms LA, Whitehall VLJ et al (2004) BRAF mutation is associated with DNA methylation in serrated polyps and cancerous of colorectum. Gut 53:1137–1144
Snover DC, Jass JR, Fenoglio-Preiser C et al (2005) Serrated polyps of the large intestine a morphologic and molecular review of evolving concept. Am J Clin Pathol 124:380–391
Lazarus R, Junttila OE, Karttunen TJ et al (2005) The risk of metachronous neoplasia in patients with serrated adenoma. Am J Clin Pathol 123:349–359
Gao Q, Tsoi KK, Hirai HW et al (2015) Serrated polyps and the risk of synchronous colorectal advanced neoplasia: a systematic review and meta-analysis. Am J Gastroenterol 110:501–509
Holme O, Bretthauer M, Eide TJ et al (2015) Long-term risk of colorectal cancer in individuals with serrated polyps. Gut 64:929–936
Hazewinkel Y, de Wijkerslooth TR, Stoop EM et al (2014) Prevalence of serrated polyps and association with synchronous advanced neoplasia in screening colonoscopy. Endoscopy 46:219–224
Alton BF, Joseph M, Srivastava A et al (2008) Sessile serrated adenoma Challenging discrimination from other serrated colonic polyps. Am J Surg Pathol 32:30–35
Yamada A, Notohara K, Aoyama I et al (2011) Endoscopic feature of sessile serrated adenoma and other serrated colorectal polyps. Hepatogastroenterology 58:45–51
Daniela EA, Gustavo BB (2010) Serrated polyps of the colon and rectum (hyperplastic polyps, sessile serrated adenomas, traditional serrated adenoma, and mixed polyps)-proposal for diagnostic criteria. Virchows Arch 457:291–297
Bauer VP, Papaconstantinou HT (2008) Management of serrated adenomas and hyperplastic polyps. Clin Colon Rectal Surg 21:273–279
Longacre TA, Fenoglio-Preiser CM (1990) Mixed hyperplastic adenomatous polyps/serrated adenomas. A distinct from of colorectal neoplasia. Am J Surg Pathol 14:524–537
Makinen MJ, George SM, Jernvall P et al (2001) Colorectal carcinoma associated with serrated adenoma—prevalence, histological features, and prognosis. J Pathol 193:286–294
Carr NJ, Mahajan H, Tan KL et al (2009) Serrated and non-serrated polyps of the colorectum: their prevalence in an unselected case series and correlation of BRAF mutation analysis with the diagnosis of sessile serrated adenoma. J Clin Pathol 62:516–518
Kashida H, Ikehara N, Hamatani S et al (2011) Endoscopic characteristics of colorectal serrated lesions. Hepatogastroenterology 58:1163–1167
Yark H, Thomas RW, Esther M et al (2014) Prevalence of serrated polyps and association with synchronous advanced neoplasia in screening colonoscopy. Endoscopy 46:219–224
Hassan C, Quintero E, Dumonceau JM et al (2013) European Society of Gastrointestinal Endoscopy. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 45:842–851
Richard HL, Robert MG, Christopher MS (2010) Sessile serrated adenomas: prevalence of dysplasia and carcinoma in 2139 patients. J Clin Pathol 63:681–686
Jass JR (2001) Serrated route to colorectal cancer: back street or super highway? J Pathol 193:283–285
Acknowledgments
We thank Ms. Noriko Yamamoto MD, who performed the re-examination of the pathological diagnoses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chino, A., Yamamoto, N., Kato, Y. et al. The frequency of early colorectal cancer derived from sessile serrated adenoma/polyps among 1858 serrated polyps from a single institution. Int J Colorectal Dis 31, 343–349 (2016). https://doi.org/10.1007/s00384-015-2416-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2416-2