Abstract
Background
The purpose of the present study was to evaluate the problems, treatment outcome, and contributory factors to delayed presentation in Hirschsprung’s disease (HD) after 1 year of age in a resource-limited setting.
Methods
This retrospective study included 41 children aged >1 year with HD managed at the University of Nigeria Teaching Hospital, Enugu, in south eastern Nigeria, between January 2000 and June 2009.
Results
Complications of HD were evident at presentation in 38 (92.7%) of the 41 children. Late presentation was due to delayed referral in 27 cases (65.9%), parental ignorance in 11 (26.8%), and poverty in 3 (7.3%). The HD was rectosigmoid in 33 patients (80.5%) and was of ultra-short length variety in 8 patients (19.5%). Thirty-five patients (85.4%) required colostomy for decompression, and colostomy-related complications occurred in 24 of them (68.6%). The definitive surgical procedure was a Swenson pullthrough in 34 cases (82.9%) and posterior myectomy in 7 others (17.1%). Twenty patients (48.8%) experienced at least one postoperative complication. After follow-up of 7–64 months (mean: 31 months), 31 (75.6%) patients had a good outcome, 6 (14.6%) had persistent constipation, 3 had (7.3%) incontinence, and one child (2.4%) died from overwhelming infection.
Conclusions
Hirschprung’s disease presenting after 1 year of age may be associated with high colostomy rates and increased morbidity. Continued dissemination of updated information on HD to medical practitioners and a public awareness campaign may improve time to diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hirschsprung’s disease (HD) is an enteric nervous system disorder characterized by lack of ganglia in the enteric plexuses. The aganglionic segment extends from the anorectum for a variable colonic or intestinal distance [1]. The clinical presentation of HD is dependent not only on the length of the aganglionosis, but also on the age of the patient [1, 2]. About 90% of all cases of HD produce clinical signs during the newborn period [3, 4]. This, coupled with advancements in molecular studies, imaging, and histochemistry, presupposes early diagnosis for most cases of HD. Without early diagnosis and appropriate treatment, many children will go on to develop serious complications such as acute enterocolitis or toxic megacolon [1, 5]. Delayed presentation may also influence overall management protocol and preclude one-stage operative treatment. The net result may be increased morbidity and mortality.
Most reports from developing countries [6, 7] indicate that majority of children with HD present late to a tertiary health facility for management. This late presentation, among other factors, may be responsible for the less than optimal outcome for this disease in some developing countries.
The present study looks at HD presenting after 1 year of age and evaluates the problems, outcome of treatment, and factors that contribute to delayed presentation.
Materials and methods
The study design was retrospective and involved data collection and entry into a pro forma form. The data were collected from case notes, operation records, and discharge summaries. Patients studied were limited to those with histologically confirmed cases of HD managed by the Paediatric Surgery Unit of University of Nigeria Teaching Hospital Enugu (UNTH) from January 2000 to June 2009. At UNTH, patients presenting with HD are evaluated by unit medical staff and commenced on nonoperative bowel decompression with suppositories, rectal washout, or enema. Cases that decompress well are continued on this regimen pending full evaluation and definitive treatment. For patients that fail to decompress effectively, colostomy is performed and managed until definitive therapy is possible. Definitive diagnosis is by histology of a full-thickness rectal biopsy specimen. The extent of colonic involvement was defined by level of transition zone on a lateral film of a barium enema study.
For the purposes of the present study, the following were considered: patient and disease-related factors and treatment-related factors
Patient and disease-related factors
Only cases in which patients had symptoms from the neonatal period but that presented after 1 year of age were included. Age at presentation, gender, documented reason for delayed presentation, main clinical presentation, and type of HD were considered.
Treatment-related factors
The following factors were considered in describing the treatment protocol: mode of bowel decompression, indications for colostomy, types and complications of colostomy, duration of colostomy before definitive operation, types of definitive operation, complications of definitive operation, overall outcome, duration of follow-up, and duration of active treatment (interval from the time the initial bowel decompression was commenced to the time patient was discharged after definitive treatment and colostomy closure). Outcome was categorized according to the presence or absence of residual constipation, incontinence, or mortality. Patients with regular, unaided, and controlled 2–3 bowel movements per day were considered to have a good outcome.
Data analysis
The Statistical Package for Social Sciences (SPSS Inc, Chicago, IL, 11.5 version) was used for data entry and analysis.
Results
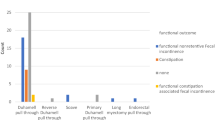
A total of 41 children were studied, and they represent 57.7% (41/71) of all cases of HD managed during the study period. There were 38 (92.7%) males and 3 (7.3%) females. The median age was 4 years (range: 1.2–14 years) (Table 1). Twenty-eight patients (68.3%) had delayed passage of meconium, and 13 (31.7%) did not have a history of delayed passage of meconium. The main presentation was chronic constipation in all cases (100%). There was abdominal distension in 29 (70.7%), and palpable fecaloma in 33 (80.5%); 22 patients (53.7%) had anemia, 13 (31.7%) presented with toxic colitis, and 10 (24.4%) had failure to thrive (Fig. 1).
Thirty-three (80.5%) patients had rectosigmoid disease, and 8 (19.5%) had ultra-short disease. Initially, 17 (41.5%) patients had adequate bowel decompression with nonoperative treatment, and 24 (58.5%) did not. Of the 17 that initially decompressed well nonoperatively, only 6 (35.3%) continued to decompress effectively. Overall, 35 patients (85.4%) required colostomy as a result of poor decompression (Fig. 1), and 6 patients (14.6%) did not require colostomy. The type of colostomy was loop in 21 patients (60%) and defunctioning in the other 14 (40%). After a median stoma duration of 6 months (range: 2–20 months), 24 (68.6%) patients had one or more complications directly related to the colostomy formation. The complications were skin excoriation (n = 11), stoma prolapse (n = 11), and stoma stenosis (n = 2). Two patients with stoma prolapse required operative revision of the colostomy. The remaining cases were managed nonoperatively.
Preoperatively, 22 (62.9%) of the patients with colostomy required manual disimpaction of fecaloma.
For definitive operative treatment, 34 (82.9%) patients had a Swenson pullthrough, and 7 (17.1%) had posterior myectomy. Twenty (48.8%) patients had one or more procedure-related complication (Table 2)—viz: constipation (n = 7; 17.1%), incontinence (n = 5; 12.2%), toxic colitis (n = 3; 7.3%), wound infection (n = 2; 4.9%), stenosis (n = 2; 4.9%), or pelvic abscess (n = 1; 2.4%).
Closure of colostomy was carried out 10 to 23 days (mean: 17 days) following definitive surgery in the 35 cases. Complications of colostomy closure occurred in 9 patients (25.7%) and included wound infection (4), stitch granuloma (2), incisional hernia (2), and superficial wound dehiscence (1).
Outcome
Overall, 31 (75.6%) children had a good outcome, 6 (14.6%) had mild persistent constipation, 3 (7.3%) had incontinence, and one (2.4%) child died from septicemia. The one death occurred in a 5-year old with rectosigmoid disease. Residual constipation was more common in patients who had myectomy compared to Swenson pullthrough (4/7 versus 2/34; P = 0.004), whereas incontinence occurred exclusively in patients who had a Swenson pullthrough. The patients with persistent constipation were managed nonoperatively by anal dilatation over a 3–4-week period. The children with incontinence were managed with antimotility drugs.
The average duration of active treatment was 7.5 months (range: 1–23 months), and the average duration of follow-up was 31 months (range: 7–64 months).
Delay in presentation
Delay in presentation was due mainly to delayed referral from primary and secondary health facilities in 27 cases (65.9%), parental ignorance in 11 cases (26.8%), and poverty in 3 cases (7.3%).
Discussion
The findings of the present study show that a considerable proportion of HD patients in our setting are seen late at the tertiary centers, where they are brought for appropriate treatment. This subset of patients has predominantly the rectosigmoid form of the disease, and the majority require colostomy and multi-staged treatment, with attendant increased morbidity.
Previous reports have indicated that the preponderance of HD cases produce clinical features in the newborn period, and >90% of affected children have a definitive diagnosis before the age of one [1–4]. In the present report, a significant number of the cases had features of the disease (delay in passing meconium and chronic constipation) from the newborn period. Despite this evidence, these patients had delayed presentation and definitive diagnosis. Similar delay in diagnosis has been documented in previous reports from developing countries [7, 8]. In our setting, the prime factor responsible for this impediment was delayed referral to a tertiary health facility from primary and secondary facilities. Evidently, there were physician errors in recognition of this disease at the primary and secondary levels of care. Nonetheless, this retrospective study may not allow conclusive determination of the main factor in the delayed diagnosis as there may be a complex interplay of sociocultural factors in our setting. Possible interventions may include educating primary care physicians/healthcare community workers in the early diagnosis of this disease. In the short term this can be achieved by organizing regular workshops on early diagnosis, initial interventions, and need for early referral not only for HD but for all surgically correctable anomalies. In addition, inclusion of basic clinical diagnosis of these anomalies in the curriculum of primary healthcare training may offer a long-term solution.
The presentation of the cases in the series reported here reflect features of complicated HD. Toxic colitis, anemia, fecal impaction, and failure to thrive are recognized complications that may follow delayed or inappropriate treatment of the disease [5]. The high incidence of these complications at presentation indicates that surgeons managing such cases may have to develop strategies to address these problems in order to minimize morbidity and mortality.
The patients in this series had rectosigmoid and ultra-short segment disease. There were no cases of long segment, total colonic, or total intestinal HD, probably because such cases would have manifested earlier with severe intestinal obstruction. Usually, cases of rectosigmoid and ultra-short HD can be effectively decompressed with nonoperative methods that employ suppositories, enemas, and rectal washout. In the present study, nonoperative decompression was not successful in more than 80% of the patients. This failure may be related to a high incidence of impacted feces and, possibly, associated chronic bowel inflammation. Patients with these complications will need colostomy for effectual decompression. This explains the high colostomy rate of 85.4% in the present report. Somerecent series [3, 9, 10] report an overall colostomy rate of less than 40% in HD. It is important to note that though colostomy is crucial in the management of selected cases of HD, it may be associated with complications and even death [11, 12]. The complications of colostomy in this study are similar to those of earlier reports [11], but the high incidence of prolapse may be related to the markedly dilated and redundant colon in most of these patients. It may also be related to the frequent use of the loop type of colostomy. Prolapse can be minimized by constructing defunctioning colostomies or, where facilities are available for frozen section, leveling colostomy.
Over the past decade, one-stage pullthrough procedures for the treatment of HD have become popular among pediatric surgeons. The advantages range from reduced hospital stay to reduced overall morbidity and mortality [13, 14]. Such procedures are ideal for patients with uncomplicated rectosigmoid and ultra-short HD. The cases in the present study could not have been managed by these procedures because of the impediments imposed by failed nonoperative decompression, the presence of huge fecalomas, and markedly dilated bowel. Multi-stage treatment is therefore inevitable in most cases presenting after 1 year in our setting. Definitive treatment of these patients may be challenging, as the fecalomas have to be disimpacted manually; megacolon must be allowed to return to regular caliber; and nutritional deficiencies and anemia must be corrected preoperatively. In addition, the multi-stage management may increase the overall morbidity, because each of the stages—colostomy formation, definitive operation, and colostomy closure—is associated with distinct complications.
The overall outcome of treatment in the present report may be similar and comparable to results reported in studies involving both older children and younger children [2, 9, 10]. However, for the reasons already stated, the incidence of complications of treatment is higher in older children than in younger children [4, 10, 15]. Given the short duration of follow-up in the present study, the overall complications may increase with the occurrence of some late complications as the duration of follow-up increases.
Conclusions
A significant proportion of children with HD presenting after 1 year in our setting have complications of the disease. Majority of these patients will require colostomy for effective bowel decompression, and multi-staged treatment with increased morbidity. Addressing the delay in presentation through enlightenment programs for primary care physicians, and public health education, will improve time to diagnosis and minimize challenges of managing HD in our setting.
References
Martucciello G (2008) Hirschsprung’s disease, one of the most difficult diagnoses in pediatric surgery: a review of the problems from clinical practice to the bench. Eur J Pediatr Surg 18:140–149
Higashi M, Ieiri S, Teshiba R, Saeki I, Taguchi T (2009) Hirschsprung’s disease patients diagnosed at over 15 years of age: an analysis of a Japanese nationwide survey. Pediatr Surg Int 25:945–947
Singh SJ, Croaker GDH, Manglick P, Wong CL, Athanasakos H, Elliott E, Cass D (2003) Cass D Hirschsprung’s disease: the Australian Paediatric Surveillance Unit’s experience. Pediatr Surg Int 19:247–250
So HB, Becker JM, Schwartz DL, Kutin ND (1998) Eighteen years experience with neonatal Hirschsprung’s disease treated by endorectal pull-through without colostomy. J Pediatr Surg 33:673–675
Powell RW (1909) Hirschsprung’s disease in adolescents. Misadventures in diagnosis and management. Am Surg 55:212–218
Momoh JT (1982) Hirschsprung’s disease: problems of diagnosis and treatment. Ann Trop Paediatr 2:31–35
Poenaru D, Borgstein E, Numanoglu A, Azzie G (2010) Caring for children with colorectal disease in the context of limited resources. Semin Pediatr Surg 19:118–127
Archibong AE (2002) Pattern of aganglionic megacolon in Calabar, Nigeria. S Afr Med J 92:642–644
Pratap A, Gupta DK, Shakya VC, Adhikary S, Tiwari A, Shrestha P et al (2007) Analysis of problems, complications, avoidance and management with transanal pull-through for Hirschsprung disease. J Pediatr Surg 42:1869–1876
Suita S, Taguchi T, Ieiri S, Nakatsuji T (2005) Hirschsprung’s disease in Japan: analysis of 3852 patients based on a nationwide survey in 30 years. J Pediatr Surg 40:197–202
Ekenze SO, Agugua-Obianyo NE, Amah CC (2007) Colostomy for large bowel anomalies in children: a case controlled study. Int J Surg 5:273–277
Chandramouli B, Srinivasan K, Jagdish S, Ananthakrishnan N (2004) Morbidity and mortality of colostomy and its closure in children. J Pediatr Surg 39:596–599
Pratap A, Shakya VC, Biswas BK, Sinha A, Tiwari A, Agrawal AS et al (2007) Single-stage transanal endorectal pull-through for Hirschsprung’s disease: perspective from a developing country. J Pediatr Surg 42:532–535
Obermayr F, Szavay P, Beschorner R, Fuchs J (2009) Outcome of transanal endorectal pull-through in patients with Hirschsprung’s disease. Eur J Pediatr Surg 19:220–223
Dasgupta R, Langer JC (2008) Evaluation and management of persistent problems after surgery for Hirschsprung’s disease in a child. J Pediatr Gastroenterol Nutr 46:13–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ekenze, S.O., Ngaikedi, C. & Obasi, A.A. Problems and Outcome of Hirschsprung’s Disease Presenting after 1 Year of Age in a Developing Country. World J Surg 35, 22–26 (2011). https://doi.org/10.1007/s00268-010-0828-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0828-2