Abstract
Purpose
In congenital diaphragmatic hernia (CDH), ultrasound (U/S) measurements of the contralateral lung commonly provide the observed-to-expected lung-to-head ratio (O/E LHR) and are used to determine the severity of pulmonary hypoplasia. Fetal magnetic resonance imaging (MRI) measurement of the observed-to-expected total lung volume (O/E TLV) has been used as an adjunct to O/E LHR in predicting outcomes. Since O/E LHR only measures the contralateral lung, we sought to investigate if MRI measurements of the contralateral lung volume (O/E CLV) can accurately predict outcomes in CDH. We hypothesize that O/E CLV is a better predictor of CDH outcomes than O/E LHR.
Methods
We identified all infants with a prenatal diagnosis of CDH at our fetal center who had both MRI and U/S measurements. Using lung volume ratios of right–left 55:45, we calculated O/E CLV from O/E TLV. We used receiver-operating characteristic (ROC) curves to calculate the area under the curve (AUC) to compare the predictive accuracy of O/E CLV to O/E LHR for ECMO support, as well as survival to both discharge and 1 year.
Results
Seventy-four patients had complete prenatal imaging with 39% requiring ECMO support. The median O/E CLV was 48.0% and the median O/E LHR was 42.3%. O/E CLV was a better predictor of the need for ECMO support (AUC 0.81 vs. 0.74). O/E CLV was a better predictor of survival to discharge (AUC 0.84 vs. 0.64) and 1-year survival (AUC 0.83 vs. 0.63) than O/E LHR.
Conclusion
O/E LHR is a well-validated standard for predicting outcomes and guiding prenatal counseling in CDH. We provide evidence that fetal MRI measurements of the contralateral lung volume corrected for gestational age were more accurate in predicting the need for ECMO and survival. Future prospective studies validating O/E CLV regarding outcomes and ECMO utilization are warranted.
Level of evidence
Level III, retrospective comparative study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital diaphragmatic hernia (CDH) carries long-term morbidity secondary to pulmonary hypoplasia and persistent pulmonary hypertension [1, 2]. Routine prenatal imaging for congenital anomalies has led to the prenatal diagnosis of over 60% of CDH cases [3]. Antenatal diagnosis allows for delivery at fetal care centers that specialize in perinatal management of CDH. Additionally, prenatal diagnosis and imaging can potentially be used for determination of prenatal intervention in severe cases and may improve parental counseling using imaging characteristics to predict patient outcomes. Unfortunately, there is no consensus on the optimal modality of prenatal imaging for predicting patient morbidity and mortality in CDH.
One of the most widely used prenatal predictive values for postnatal outcome in CDH is the observed-to-expected lung-to-head ratio (O/E LHR) [1, 4, 5]. Two-dimensional ultrasonography is used to measure the volumetric ratio of the lung contralateral to the diaphragmatic hernia to the fetal head while correcting for gestational age and expected lung development. O/E LHR combined with evidence of liver herniation is currently the gold standard for determining candidacy for fetal intervention [6, 7]. Unfortunately, O/E LHR accuracy is highly sonographer dependent [8], has poor predictive value when used alone [9], and has a limited role in right-sided hernias [10].
Prenatal imaging at many fetal care centers now includes magnetic resonance imaging (MRI) to further characterize congenital anomalies. MRI has the added benefit of more accurate volumetric analysis of the lungs [11, 12]. Total fetal lung volume when corrected for gestational age (O/E TFLV), calculated based on fetal MRI, has been shown to be comparable to ultrasound (U/S)-derived parameters as a predictor of mortality [13,14,15,16]. Additional studies suggest that O/E TFLV may provide superior predictive value when compared to O/E LHR [17, 18].
Volumetric analysis of the hypoplastic ipsilateral lung can be challenging and is often underestimated by both U/S and MRI [19]. MRI quantification of contralateral lung volume alone may offer a more reliable measurement of lung volume and allows for the direct comparison to the gold standard on U/S. As O/E LHR measures the contralateral lung volume alone, we sought to evaluate the prognostic value of MRI-derived observed-to-expected contralateral lung volume (O/E CLV). We hypothesized that O/E CLV is more accurate at predicting outcomes compared to O/E LHR.
Methods
Setting
This was an Institutional Review Board approved study. The records of all infants with a prenatal diagnosis of CDH who were referred to our Fetal Center between January 2008 and December 2018 were reviewed retrospectively.
Subjects and definitions
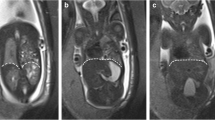
We identified all children in our prospectively maintained CDH database who had both MRI and U/S measurements within 1 week of each other. Our multi-disciplinary CDH teams’ practice is to have two clinic visits with all families with a prenatal diagnosis of CDH. The first visit occurs at < 31 weeks of gestational age (defined as the early visit) and the second visit occurs at ≥ 31 of gestational age (defined as the late visit). Our rationale for delayed imaging is that the late gestational MRI has been shown to be more accurate for determining lung volumes [20, 21]. At each visit, calculated MRI and US volumes were obtained from studies performed and interpreted by dedicated fetal radiologists. Throughout the study period, our team of fetal radiologists calculated lung volumes on both MRI and U/S. One fetal radiologist (senior author, M.L.M) retrospectively went back through all the patients’ imaging to calculate any missing values for lung volumes. All non-contrast fetal MRI studies were performed in a 1.5 Tesla scanner (either Siemens Healthcare Magneton Avanto; or Philips Ingenia- Philips Healthcare). All patients were scanned under the same pre-existing imaging protocol, specific for fetuses with a working diagnosis of congenital diaphragmatic hernia.
O/E LHR was calculated from the fetal U/S utilizing the trace method [6, 22]. MRI measurements of the Observed fetal lung volume were obtained by manually contouring each lung using a freehand tracing tool in a separate 3D workstation (TeraRecon software, Aquarius iNtuition INC). After the lungs are contoured in each slice visualized, a volume is generated by the software [23]. The Expected contralateral fetal lung volume was derived from the mean TFLV at each gestational age volume published by Meyers et al. using lung volume ratio of right–left 55:45 to calculate O/E CLV [23]. For example, a 23-week gestation fetus is expected to have a 24.1 mL of mean total lung volumes based on the work done by Meyers et al. Therefore, the expected right lung volume would be 13.3 mL (55% of the total lung volume) and the expected left lung volume would be 10.8 mL (45% of the total lung volume). A fetus with a left-sided CDH with a 9.9 mL right lung volume calculated on MRI at 23 weeks would have an O/E CLV of 74% (9.9 mL/13.3 mL).
To determine the generalizability and diagnostic accuracy of O/E CLV, we included all patients with right-sided CDHs, as well as those patients with any chromosomal abnormalities and cardiac defects if they had met our inclusion criteria (complete prenatal imaging). In all cases, we examined the oldest gestational age imaging available. Excluded from this study were any patients who had missing MRI or U/S measurements. Study data were collected from the electronic medical records of identified subjects with CDH, including baseline demographic data (gestational age at diagnosis and birth), ECMO support, and mortality.
Statistical analysis
Data are presented as means with standard deviations, medians with interquartile ranges, or frequencies with percentages as appropriate. Continuous variables were tested for group differences using Student’s t test, while Chi-squared testing was utilized for categorical variables. Next, we used receiver-operating characteristic (ROC) curves to define the optimal cut-points for early and late prenatal imaging to predict ECMO support, survival to discharge, and survival to 1 year. Finally, we used ROC curves to calculate the area under the curve (AUC) to directly compare the predictive accuracy of O/E CLV to O/E LHR for ECMO support, survival to discharge, and survival to 1 year. Significance was set at 0.05. R version 3.4.1 software (R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/) was utilized.
Results
Baseline demographics and imaging characteristics
Seventy-four infants met inclusion criteria and had complete prenatal imaging. A breakdown of the demographic characteristics of the 74 patients is shown in Table 1. Of these 74 patients, six had a right-sided defect. Significant co-morbidities worth noting include two patients who were never repaired and both expired (one with a complete laryngotracheal esophageal cleft and the other with Trisomy 18). The average gestational age of the last complete set of imaging was 34 ± 1.2 weeks. The average gestation age at the time of delivery is 36.9 ± 1.9 weeks. The overall survival at discharge was 78.4% (58/74) and the 1-year survival was 77.1% (54/70), with four CDH neonates still alive but less than 1 year old. Twenty-nine (39%) infants were supported on ECMO.
Imaging characteristics in the early visit (< 31 weeks) (n = 45)
Forty-five patients (58%) had imaging before 31 weeks. The median gestational age of the patients at the time of the early visit was 24 (IQR 23, 27) weeks. On MRI, the median contralateral lung volume was 7.5 mL (IQR 5.4, 12 mL). The median O/E CLV was 49.0% (IQR 42, 52) and the median O/E LHR was 39% (IQR 28, 53). To provide prognostic information for providers who care for a CDH fetus before 31 weeks, we generated ROC curves for the contralateral lung volume on MRI to determine the accuracy in predicting ECMO support, survival to discharge, and survival to 1 year. Furthermore, ROC curves were generated for O/E LHR for the same outcomes (Table 2).
Imaging characteristics in late visit (≥ 31 weeks) (n = 74)
All patients underwent imaging ≥ 31 weeks. The median gestational age of the late visit was 34 (IQR 33, 35) weeks. On MRI, the median late contralateral lung volume was 24 mL (IQR 18, 31). The median O/E CLV was 51% (42, 51). The median O/E LHR for the late visit was 42% (IQR 33, 53). ROC curves were generated for the contralateral lung volume on MRI for the late visit to determine the accuracy in predicting ECMO support, survival to discharge, and survival to 1 year. Moreover, ROC curves were generated for O/E LHR (Table 3).
Prognosis accuracy of O/E CLV vs. O/E LHR
Predictive ROC curves for predicting ECMO, survival to discharge, and survival to 1 year from O/E CLV and O/E LHR were taken using the oldest gestational age imaging available for each patient. O/E CLV was a better predictor than O/E LHR of the need for ECMO support (AUC 0.81 vs. 0.74) (Fig. 1). Furthermore, O/E CLV was a better predictor of survival to discharge (AUC 0.84 vs. 0.64) (Fig. 2) and 1-year survival (AUC 0.83 vs. 0.63) than O/E LHR (Fig. 3).
Discussion
In this single-center retrospective study of prospectively collected data, we provide evidence that the novel O/E CLV on fetal MRI is more accurate to O/E LHR at prenatally predicting the need for ECMO and survival in neonates with CDH. While O/E LHR is a well-validated standard for predicting outcomes and guiding prenatal counseling in CDH, these data provide additional evidence that the contralateral fetal lung size impacts prognosis in infants with CDH and may be used in the future. Although it is well established that fetal lungs undergo exponential growth after 24 weeks, we provide evidence that there are differences in the early (< 31 weeks) and late (> 31 weeks) MRI measurements of lung volumes (Table 2). In contrast, the accuracy of O/E LHR generally remains relatively consistent throughout gestation. This has important implications for ongoing research into the optimal gestational age by which providers should order a fetal MRI and provides ideal cutoffs for lung volumes that are gestational age-specific at predicting postnatal outcomes.
These findings are intriguing, because our work adds to a growing body of evidence that fetal MRI provides prognostic measurements that are at least equivalent to US O/E LHR. A recent systematic review showed that US O/E total fetal lung volumes could stratify fetuses to predict survival [16]. Moreover, Oluyomi-Obi T et al. found that MRI O/E total fetal lung volumes are marginally superior to US O/E LHR, but this difference dissipates when using the tracing method on ultrasound. Our study used the tracing method on ultrasound, yet we found that MRI was more accurate than ultrasound.
Past studies have shown that MRI does confer several advantages over U/S in prenatal measurements. First, it is that U/S is user-dependent, and measurements can be affected by the angle and the positioning of the ultrasound probe [14]. Second, early gestation ultrasound measurements may be prone to error [16]. Third, as we have a team of fetal radiologists who collaboratively review MRI lung volumes, the MRI measurements are less vulnerable to single user error.
What makes our findings unique is that all other studies comparing MRI to ultrasound examine the total lung volumes; however, O/E CLV only measures the contralateral lung. One reason for only measuring contralateral lung is that the ipsilateral lung could be challenging to identify and therefore measure given the surrounding herniated contents from the CDH defect. Another aspect that makes our findings more universal is that we included both right- and left-sided defects and did not exclude CDH neonates based on underlying genetic or cardiac syndromes. This point highlights a significant advantage of using O/E CLV over total lung volume, as total lung volume has mainly been studied in left-sided defects. Each fetal center can easily reproduce these findings as the lung volumes are already being measured on fetal MRI. Moving forward, the multi-disciplinary team involved in the care of CDH neonates can use these novel prenatal prognostic tools to better counsel families and arrange for appropriate prenatal and postnatal care.
Potential limitations of our study include the single-center and retrospective nature, which places us at risk for potential bias. Also, although our series of 74 neonates with CDH is one of the largest prenatal series, it is still a small sample size. Until validated in a multi-center prospective fashion, the results may not be generalizable to other fetal centers. Finally, our primary outcome measures were ECMO support and survival to 1 year, and we did not examine the utility of our novel tool to predict long-term co-morbidities (e.g., chronic lung disease).
Conclusions
We conclude that within our center, the novel fetal MRI O/E CLV provides more accurate prognostic capabilities compared to O/E LHR. This tool can be easily implemented at centers with fetal MRI capability and should be added to the prenatal evaluation for CDH. Future multi-institutional prospective studies validating the use of O/E CLV in predicting postnatal outcomes and ECMO utilization are warranted.
Change history
15 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00383-021-05033-7
References
Congenital DM, Hernia D (2018) Management & outcomes. Adv in Pediatr 65(1):241
Leeuwen L, Fitzgerald DA (2014) Congenital diaphragmatic hernia. J Pediatr Child Health 50(9):667–673
Harting MT, Lally KP (2014) The congenital diaphragmatic hernia study group registry update. Semin Fetal Neonatal Med 19(6):370–375
Cordier AG, Russo FM, Deprest J, Benachi A (2019) Prenatal diagnosis, imaging, and prognosis in congenital diaphragmatic hernia. Semin Perinatol 44:51163
Metkus AP, Filly RA, Stringer MD, Harrison MR, Adzick NS (1996) Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg 31(1):148–152
Jani JC, Benachi A, Nicolaides KH, Allegaert K, Gratacos E, Mazkereth R et al (2009) Prenatal prediction of neonatal morbidity in survivors with congenital diaphragmatic hernia: a multicenter study. Ultrasound Obstet Gynecol 33(1):64–69
Van der Veeken L, Russo FM, De Catte L, Gratacos E, Benachi A, Ville Y et al (2018) Fetoscopic endoluminal tracheal occlusion and reestablishment of fetal airways for congenital diaphragmatic hernia. Gynecol Surg 15(1):9
Senat MV, Bouchghoul H, Stirnemann J, Vaast P, Boubnova J, Begue L et al (2018) Prognosis of isolated congenital diaphragmatic hernia using lung-area-to-head-circumference ratio: variability across centers in a national perinatal network. Ultrasound Obstet Gynecol 51(2):208–213
Hedrick HL, Danzer E, Merchant A, Bebbington M, Zhao H, Flake A et al (2007) Liver position and lung-to-head ratio for prediction of extracorporeal membrane oxygenation and survival in isolated left congenital diaphragmatic hernia. Am J Obstet Gynecol 197(4):422-e1
Victoria T, Danzer E, Oliver ER, Edgar JC, Iyoob S, Partridge EA et al (2018) Right congenital diaphragmatic hernias: is there a correlation between prenatal lung volume and postnatal survival, as in isolated left diaphragmatic hernias? Fetal Diagn Ther 43(1):12–8
Deshmukh S, Rubesova E, Barth R (2010) MR assessment of normal fetal lung volumes: a literature review. Am J Roentgenol 194(2):W212-7
Rypens F, Metens T, Rocourt N, Sonigo P, Brunelle F, Quere MP et al (2001) Fetal lung volume: estimation at MR imaging—initial results. Radiology 219(1):236–41
Cannie M, Jani J, Meersschaert J, Allegaert K, Done’ E, Marchal G et al (2008) Prenatal prediction of survival in isolated diaphragmatic hernia using observed to expected total fetal lung volume determined by magnetic resonance imaging based on either gestational age or fetal body volume. Ultrasound Obstet Gynecol 32(5):633–9
Kastenholz KE, Weis M, Hagelstein C, Weiss C, Kehl S, Schaible T et al (2016) Correlation of observed-to-expected MRI fetal lung volume and ultrasound lung-to-head ratio at different gestational times in fetuses with congenital diaphragmatic hernia. Am J Roentgenol 206(4):856–66
Victoria T, Bebbington MW, Danzer E, Flake AW, Johnson MP, Dinan D et al (2012) Use of magnetic resonance imaging in prenatal prognosis of the fetus with isolated left congenital diaphragmatic hernia. Prenat Diagn 32(8):715–23
Oluyomi-Obi T, Kuret V, Puligandla P, Lodha A, Lee-Robertson H, Lee K et al (2017) Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg 52(5):881–8
Bebbington M, Victoria T, Danzer E, Moldenhauer J, Khalek N, Johnson M et al (2014) Comparison of ultrasound and magnetic resonance imaging parameters in predicting survival in isolated left-sided congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 43(6):670–4
Kim AG, Norwitz G, Karmakar M, Ladino-Torres M, Berman DR, Kreutzman J et al (2019) Discordant prenatal ultrasound and fetal MRI in CDH: wherein lies the truth? J Pediatr Surg 55:1879
Jani J, Cannie M, Done E, Van Mieghem T, Van Schoubroeck D, Gucciardo L et al (2007) Relationship between lung area at ultrasound examination and lung volume assessment with magnetic resonance imaging in isolated congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 30(6):855–60
Coleman A, Phithakwatchara N, Shaaban A, Keswani S, Kline-Fath B, Kingma P et al (2015) Fetal lung growth represented by longitudinal changes in MRI-derived fetal lung volume parameters predicts survival in isolated left-sided congenital diaphragmatic hernia. Prenat Diagn 35(2):160–6
Lee TC, Lim FY, Keswani SG, Frischer JS, Haberman B, Kingma PS et al (2011) Late gestation fetal magnetic resonance imaging–derived total lung volume predicts postnatal survival and need for extracorporeal membrane oxygenation support in isolated congenital diaphragmatic hernia. J Pediatr Surg 46(6):1165–71
Abbasi N, Ryan G, Johnson A, Sanz Cortes M, Sangi-Haghpeykar H, Ye XY et al (2019) Reproducibility of fetal lung-to-head ratio in left diaphragmatic hernia across the North American fetal therapy network (NAFTNet). Prenat Diagn 39(3):188–94
Meyers ML, Garcia JR, Blough KL, Zhang W, Cassady CI, Mehollin-Ray AR (2018) Fetal lung volumes by MRI: normal weekly values from 18 through 38 weeks’ gestation. Am J Roentgenol 211(2):432–8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest to disclose.
Ethical approval
All of the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study was evaluated and approved by the Colorado Multiple Institution Review Board (COMIRB), and a waiver of informed consent was obtained due to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Phillips, R., Shahi, N., Meier, M. et al. The novel fetal MRI O/E CLV versus O/E LHR in predicting prognosis in congenital diaphragmatic hernias: can we teach an old dog new tricks?. Pediatr Surg Int 37, 1499–1504 (2021). https://doi.org/10.1007/s00383-021-04936-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04936-9