Abstract
Background
Studies have demonstrated that same-day discharge (SDD) following thyroid resection is safe and feasible in adults but there are no similar studies in the pediatric age group. The purpose of this study is to evaluate the influence of SDD on 30-day readmission rates following thyroid surgery in pediatric patients.
Methods
This retrospective cohort study used the American College of Surgeons National Surgical Quality Improvement Program–Pediatric database to evaluate 30-day readmission rates among patients < 19 years of age who underwent thyroid resection between 2012 and 2017. Patients excluded were those discharged more than 2 days after surgery. The main exposure variable was SDD and the primary outcome was 30-day readmission. Secondary outcomes included wound complications, unplanned reoperation and death. Patient characteristics were compared using chi-squared testing and odds ratios for readmission were calculated using multivariate logistic regression.
Results
Of the 1125 patients (79% female, median age 15 years), 122 (11%) were discharged on the day of surgery. Total or near-total thyroidectomy represented the majority of operations (714, 63.5%) and patients undergoing these operations were less likely to be discharged on the same day as surgery compared to those undergoing thyroid lobectomy (4.3 vs. 22.1%, P < 0.001). Twenty-nine patients were readmitted within 30 days (3 in the same day group, 26 in the later group). There was no difference in the odds of readmission between the two groups (adjusted odds ratio in SDD compared to later discharge 1.04 [95% CI 0.29–3.75, P = 0.96; readmission rate, 2.46 vs. 2.59%). Wound complications were reported in two patients, both in the later discharge group.
Conclusion
Same-day discharge in pediatric patients undergoing thyroidectomy is not associated with an increase in 30-day readmissions or wound complications when compared to patients discharged 1 or 2 days after surgery. In selected patients, SDD may be an appropriate alternative to traditional overnight stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid nodules, malignancy, and Graves’ disease are frequent indications for thyroid surgery in the pediatric population. Although thyroid disease is less common in children, the incidence and number of thyroid operations is increasing [1,2,3].
With rising costs of healthcare in the United States, the number of surgical procedures performed on an outpatient basis has increased significantly over the last decade. In 2013, The American Thyroid Association published a consensus statement encouraging ambulatory thyroid surgery for adults. Additional studies have suggested that same-day discharge (SDD) after thyroid surgery could be undertaken safely in a select number of adult patients [4, 5].
Outpatient procedures have become more prevalent in pediatric surgery but patients undergoing thyroidectomy are more likely to be kept overnight due to fear of life-threatening complications such as expanding neck hematomas and hypocalcemia. Based on recently published data, however, the incidence of these complications is relatively low [6, 7].
This study hypothesized that same-day discharge after thyroidectomy in pediatric patients is safe and associated with no higher a rate of hospital readmissions or 30-day complications when compared to discharge on postoperative day (POD) 1 or 2.
Methods
The study protocol was reviewed and exemption was obtained from the Institutional Review Board at the University of Buffalo.
Data source
A retrospective review of the American College of Surgeons National Surgical Quality Improvement Program-Pediatric (NSQIP-P) database was performed from 1 January 2012 to 31 December 2017. The NSQIP-P is a multi-institutional, clinical surgical outcomes database that includes a sampling of cases by most pediatric surgical specialties (excluding trauma and transplant surgery) up to 30 days after a surgical procedure in patients younger than 19 years. Data for the NSQIP-P are collected in 8-day cycles for a select group of surgical procedures. These data include preoperative risk factors, Current Procedural Terminology codes for the procedure performed, and clinical data such as 30-day outcomes. More than 100 hospitals across the United States currently participate in the NSQIP-P [8, 9].
Case selection
We identified all patients younger than 19 years who underwent thyroid resection (lobectomy and total thyroidectomy) during the study period (1 January 2012–31 December 2017). SDD was defined as patients discharged on the same calendar day as surgery. Patients discharged on postoperative day 3 or later were excluded, reasoning that underlying differences in patient co-morbidities or factors unrelated to surgery, might result in prolonged postoperative hospital length of stay.
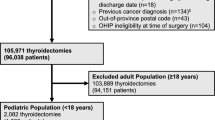
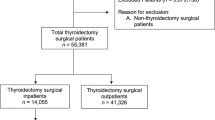
Variables collected on patients included: age, sex, race, American Society of Anesthesiology Physical Status (ASA) classification, cardiac risk factors and extent of thyroid resection (lobectomy vs. total thyroidectomy). Patients with SDD were then compared to those discharged on POD 1 or 2 (Fig. 1).
The primary outcome of interest was hospital readmission within 30 days and wound complications (e.g., superficial surgical-site infection, deep surgical-space infection, and wound dehiscence).
Statistical analysis
Analysis of retrospective data was performed and variables were incorporated into a logistic regression model to determine the odds ratio (OR) and a 95% confidence interval (CI) for readmission and wound complication rates. Categorical variables were compared using chi-squared testing and continuous variables were compared using the paired two-tailed t test. All P values were considered statistically significant if the P value was < 0.05. Statistical analyses were performed using Stata 15.1 (StataCorp, College Station, Tex., 2017).
Results
A total of 1236 patients under 19 years were identified during the study period (1 January 2012–31 December 2017) who underwent either total thyroidectomy or lobectomy. We excluded 111 patients due to postoperative stay of greater than two days. The final breakdown of patients was as follows: 122 patients (10.8%) were discharged on the same day of surgery, and 1 003 (89.2%) were discharged on POD 1 or 2 (Fig. 1). Patient demographics and type of operation are outlined in Table 1. Total or near-total thyroidectomy represented the majority of operations (714, 63.5%), and patients undergoing these procedures were less likely to be discharged on the same day as surgery compared to those undergoing thyroid lobectomy (4.3 vs. 22.1%; P < 0.001). Comparing the SDD to the later discharge group, we found that patient demographics were similar. However, male compared to female patients, and those greater than 12 years of age compared to younger were more likely to be discharged on the same-day of surgery. The two cohorts did not differ significantly by race or preoperative cardiac risk factors (Table 1).
On univariate analysis, the groups did not differ significantly in regards to both primary and secondary outcomes. Twenty-nine patients (2.6%) were readmitted within 30 days; 3 (0.3%) in the SDD group and 26 (2.3%) were patients discharged on POD 1 or 2 (P = 0.07) (Table 2). When stratified by type of operation (lobectomy or total thyroidectomy), there was also no difference in readmission rates (Table 3). Wound complications were reported in 2 patients (0.2%), both in the later discharge group. Five patients underwent unplanned reoperation. All of these patients were in the later discharge group, and among those who underwent total thyroidectomies. Reasons for reoperation included: secondary closure for hematoma, hematoma drainage, appendectomy, and completion thyroidectomy. The fifth case had missing data and did not specify reason for reoperation.
On multivariate analysis, none of the variables was associated with higher risk for 30-day readmission except for a higher ASA class (P < 0.005 for ASA Class 4). In addition, discharge timing was not associated with increased rates of readmission (adjusted odds ratio in SDD compared to later discharge 1.04 [95% CI 0.29–3.75]; P = 0.96) (Table 4). Due to the low wound complication rates (2 patients in the later discharge group), logistic regression was not feasible.
Discussion
Using data collected from a national surgical registry, we determined that SDD following pediatric thyroid surgery is not associated with an increased 30-day readmission rate or wound complication rate when compared to patients discharged on POD 1 or 2.
Although more pediatric surgical procedures are being performed as outpatient, fear of complications including expanding neck hematomas, vocal cord paresis, and hypocalcemia may influence the length of stay for pediatric patients undergoing thyroidectomy. However, the incidence of these complications is relatively low. A study reported low complications rates following pediatric thyroid surgery: hypocalcemia (permanent 1.7% and transient in 13.6%) and recurrent laryngeal nerve injury (permanent in 2.5% and transient in 1.7%). They also reported that the permanent complications occurred more frequently in very young patients with extensive or advanced disease [6]. A similar study by Scholz et al. [7] evaluated complications of 43 pediatric patients who underwent total thyroidectomy, of which two developed permanent hypocalcemia and one developed permanent vocal cord paralysis. These studies suggest that precautions can be undertaken to decrease the risk of post-thyroidectomy complications such as hypocalcemia. An example would be a protocol utilizing parathyroid hormone (PTH) levels to guide postoperative calcium replacement. A study of 30 patients by Patel et al. suggested protocolized use of point-of-service PTH measurement allowed physicians to predict which patients were at highest risk of postoperative hypocalcemia [10]. Another study demonstrated that postoperative PTH of less than 16 pg/mL predicted hypocalcemia with a sensitivity of 80% and specificity of 100%. This study suggested the use of PTH levels to initiate preventative calcium treatment and reduce LOS [11]. Implementation of a standardized protocol for postoperative management of hypocalcemia may help identify patients who can be safely discharged on the same day of surgery versus those who should be admitted for further monitoring.
With rising costs of healthcare, there has been a trend toward more outpatient procedures to reduce hospital length of stay. SDD after certain pediatric procedures, such as uncomplicated appendectomy, has become more prevalent. Various studies have outlined the numerous benefits of SDD after appendectomy, such as higher family and patient satisfaction along with reduction of hospital costs of greater than $4 000 per patient [12,13,14,15]. When accumulated over a number of procedures, SDD can effectively decrease costs and reduce inpatient resource utilization.
In our study, the two cohorts of patients (SDD and POD 1 or 2 discharge) did not differ in regards to race or preoperative cardiac risk factors. Younger patients (< 12 years of age) were less likely to be discharged on the same day of surgery, however when stratified by age (0–12 years and > 12 years), there was no significant difference in readmission or wound complication rates. This finding was different compared to other publications which outline higher rates of postoperative complications and greater length of stay (LOS) in younger children following thyroid surgery [16,17,18]. A cross-sectional analysis reported greater complication rates among pediatric patients aged 0–6 and 7–12 years when compared to patients over age 12; prolonged LOS was also seen in patients less than 12 years of age. Additionally, a retrospective analysis of 2 753 pediatric patients undergoing thyroid surgery concluded that younger children (age less than 6) had a significantly longer hospital course as well as greater risk of postoperative complications [18]. These studies suggest the need for closer monitoring in younger patients undergoing thyroid surgery and supports admission in this demographic of patients.
This study has several limitations, including its retrospective nature and the use of a single database. Although NSQIP-P is widely used in quality outcome-based research, it constitutes only a sample of all institutions in the United States, and therefore, may not provide data generalizable to all pediatric centers. The Kid’s Inpatient Database (KID) is a national database which includes majority of hospitals in the United states; 5118 hospitals within 44 out of 50 states. The database from 2012 revealed a total of 449 partial and 779 total thyroidectomies performed [19]. Our study reported a total of 1125 patients from 2012 to 2017, of which 714 underwent total and 411 underwent partial thyroidectomy. In addition, the decision to discharge a patient home safely on the first day of surgery is multifactorial, and not all relevant decision points are captured from a database. This study was also limited by its small sample size, and therefore has limited statistical power.
Despite these shortcomings, the NSQIP-P is a large database that samples a number of institutions, providing the opportunity to analyze data and 30-day outcomes of pediatric surgery patients. We believe this study effectively evaluates readmission and wound complication rates in pediatric patients who underwent thyroid surgery.
Conclusion
Same-day discharge in a select group of pediatric patients undergoing thyroidectomy is not associated with an increase in 30-day readmission rates or wound complications when compared to patients discharged 1 or 2 days after surgery. In a select group of patients, SDD may be an appropriate alternative to traditional overnight stay.
References
Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. The American Thyroid Association Guidelines Task Force on Pediatric Thyroid Cancer. Thyroid 25(7):716–759
Ward E, DeSantis C, Robbins A, Kohler B, Jemal A (2014) Childhood and adolescent cancer statistics. CA Cancer J Clin 64(2):83–103
Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7):716–759
Terris DJ, Snyder S, Carneiro-Plas D, Inabnet WB, Kandil E, Orloff L et al (2013) American Thyroid Association statement on outpatient thyroidectomy. Thyroid 23(10):1193–1202
Khandra H, Mohamed S, Hauch A, Carter J, Hu T, Kandil E (2017) Safety of same-day thyroidectomy: meta-analysis and systematic review. Gland Surg 6(4):292–301
Bussieres V, Roy S, Deladoey J, Rosseau E, St-Vil D, Piche N (2019) Pediatric thyroidectomy: favorable outcomes can be achieved by a multidisciplinary team of pediatric providers. J Pediatr Surg 54(3):527–530
Scholz S, Smith JR, Chaignaud B, Shamberger RC, Huang SA et al (2011) Thyroid surgery at Children’s Hospital Boston: a 35-year single-institution experience. J Pediatr Surg 46(3):437–442
Gallaway KE, Ahn J, Callan AK (2020) Thirty-Day outcomes following pediatric bone and soft tissue sarcoma surgery: a NSQIP pediatrics analysis. Sarcoma 14(2020):1283080
About ACS NSQIP Pediatric. American College of Surgeons. https://www.facs.org/quality-programs/childrens-surgery/pediatric/overview
Patel NA, Bly RA, Adams S, Carlin K, Parikh SR, Dahl JP et al (2018) A clinical pathway for the postoperative management of hypocalcemia after pediatric thyroidectomy reduces blood draws. Pediatr Otorhinolaryngol 105:132–137
Freire AV, Ropelato MG, Ballerini MG, Acha O, Bergada I, de Papendieck LG et al (2014) Predicting hypocalcemia after thyroidectomy in children. Surgery 156(1):130–136
Halter JM, Mallory B, Neilson IR, Langer M (2016) Same-day discharge following laparoscopic appendectomy for uncomplicated appendicitis as a measure of quality in the pediatric population. J Laparoendosc Adv Srg Tech A 25(4):309–313
Farasch SM, Damielson PD, Walford NE, Harmel RP Jr, Chandler NM (2014) Same-day discharge after appendectomy results in cost savings and improved efficiency. Am Surg 80(8):787–791
Skarda DE, Rollins M, Andrews S et al (2015) One hospital one appendectomy: the cost effectivemness of a standardized doctor’s preference card. J Pediatric Surg 50(6):919–922
Baumgarten HD, Bauer AJ, Isaza A, Mostoufi-Moab S, Kazahaya K, Adzick NS (2019) Surgical management of pediatric thyroid disease: complication rates after thyroidectomy at the Children’s Hospital of Philadelphia high-volume Pediatric Thyroid Center. J Pediatr Surg 54(10):1969–1975
Sosa JA, Tuggle CT, Wang TS, Thomas DC, Boudourakis L, Rivkees S et al (2008) Clinical and economic outcomes of thyroid and parathyroid surgery in children. J Clin Endocrinol Metab 93(8):3058–3065
Al-Qurayshi Z, Hauch A, Srivastav S, Aslam R, Friedlander P, Kandil E (2016) A national perspective of the risk, presentation, and outcomes of pediatric thyroid cancer. JAMA Otolaryngol Head Neck Surg 142(5):472–478
Hanba C, Svider PF, Siegel B, Sheyn A, Shkoukani M, Lin HS et al (2017) Pediatric thyroidectomy: hospital course and perioperative complications. Otolaryngol Head Neck Surg 156(2):360–367
Hanba C, Svider PF, Siegel B, Sheyn A, Shkoukani M et al (2017) Pediatric thyroidectomy. Otolaryngol Head Neck Surg 156(2):360–367
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jasmine Bhinder & David Rothstein. The first draft of the manuscript was written by Jasmine Bhinder and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any financial conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhinder, J., Bethin, K., Kukar, M. et al. Association of same-day discharge with hospital readmission after pediatric thyroidectomy. Pediatr Surg Int 37, 1259–1264 (2021). https://doi.org/10.1007/s00383-021-04927-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04927-w