Abstract
Background
A positive relationship between an individual surgeon’s operative volume and clinical outcomes after pediatric and adult thyroidectomy is well-established. The impact of a hospital’s pediatric operative volume on surgical outcomes and healthcare utilization, however, are infrequently reported. We investigated associations between hospital volume and healthcare utilization outcomes following pediatric thyroidectomy in Canada’s largest province, Ontario.
Methods
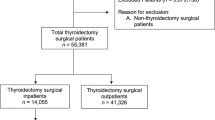
Retrospective analysis of administrative and health-related population-level data from 1993 to 2017. A cohort of 1908 pediatric (<18 years) index thyroidectomies was established. Hospital volume was defined per-case as thyroidectomies performed in the preceding year. Healthcare utilization outcomes: length of stay (LOS), same day surgery (SDS), readmission, and emergency department (ED) visits were measured. Multivariate analysis adjusted for patient-level, disease and hospital-level co-variates.
Results
Hospitals with the lowest volume of pediatric thyroidectomies, accounted for 30% of thyroidectomies province-wide and performed 0–1 thyroidectomies/year. The highest-volume hospitals performed 19–60 cases/year. LOS was 0.64 days longer in the highest, versus the lowest quartile. SDS was 83% less likely at the highest, versus the lowest quartile. Hospital volume was not associated with rate of readmission or ED visits. Increased ED visits were, however, associated with male sex, increased material deprivation, and rurality.
Conclusions
Increased hospital pediatric surgical volume was associated with increased LOS and lower likelihood of SDS. This may reflect patient complexity at such centers. In this cohort, low-volume hospitals were not associated with poorer healthcare utilization outcomes. Further study of groups disproportionately accessing the ED post-operatively may help direct resources to these populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical complications following thyroidectomy are more frequent in the pediatric population when compared to adults [1]. Thyroidectomy performed by a high-volume surgeon has been associated with improved clinical outcomes in adults and children [2,3,4,5,6,7,8,9,10] and, although less frequently reported, reduced healthcare utilization [2, 3, 5,6,7,8]. Current management guidelines advocate thyroidectomy by a high-volume thyroid surgeon—defined as more than 30 cervical endocrine procedures annually [11, 12]. Nevertheless, pediatric thyroidectomy volumes are typically lower than those for adult surgeons and often do not achieve these targets [1, 8].
A hospital’s overall surgical volume is distinct from an individual surgeon’s operative volume. Hospital volume has been associated with clinical outcomes; however, there are few pediatric studies investigating healthcare utilization outcomes [1, 5, 6, 9, 13,14,15]. We were interested in the impact of a hospital’s surgical volume on post-thyroidectomy healthcare utilization in children.
We describe the patterns of surgical care for children undergoing thyroidectomy in Ontario, Canada (a single-payor, publicly funded healthcare system). We investigate the relationship between hospital volume and healthcare utilization using population-level data, which are primarily collected for the purposes of billing and provincial healthcare resource allocation. In Ontario, access to linked administrative and healthcare-related provincial databases provides a unique opportunity to address these aims.
Methods
Data source and study population
We established a population-based cohort of provincially-insured Ontario residents, who underwent first thyroidectomy before age 18, between April 1, 1993 and March 31, 2017 (Fig. 1) via ICES. ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze healthcare and demographic data, without consent, for health system evaluation and improvement.
Ontario is divided into 14 administrative health regions (AHRs, also known as local health integration networks (LHINs)). Supplementary Table 1 shows each region’s population and the number of hospitals performing pediatric thyroidectomy in each region. Demographics and healthcare episode related data (including surgical data) were collected through several databases (Supplementary Appendix 1). Information on cancer diagnosis was derived from the Ontario Cancer Registry (OCR). Unique encoded identifiers link these datasets. For privacy, outputs were suppressed for event counts ≤ 5. Authorization under Sect. 45 of Ontario’s Personal Health Information Protection Act, which does not require Research Ethics Board review, permitted the use of these data.
Defining surgical volume
Hospital thyroidectomy volume was defined as the number of pediatric thyroidectomies completed within the preceding year, as has been described previously [9, 13]. This definition accounted for hospital mergers and closures, and changes in hospital volume over time.
A sensitivity analysis evaluated other definitions of hospital volume—thyroidectomies in patients aged <12 years, or all ages (adult and pediatric). The findings were consistent with our primary analysis and not further reported.
Outcome variables
Readmission and emergency department (ED) visits were measured within 30 days of the index surgery. Same day surgery (SDS) was defined as the same date of admission and discharge.
Secondary variables included the Johns Hopkins Aggregated Diagnosis Group (ADG; a co-morbidity index, divided by quintile, predictive of future healthcare utilization, and which was determined by data collected in the 5 years preceding surgery [16,17,18]) and material deprivation quintile (this equates to the marginalization index for an individual’s dissemination area—the smallest geographical unit in which they reside at the time of surgery—which is related to poverty and an individual or community’s ability to access basic material needs [19]).
Statistical analysis
The Chi-squared and one-way ANOVA tests were used, as appropriate, for univariate analysis. Statistical significance was defined by p < 0.05. Variables meeting statistical significance were included in multivariate regression analysis for each primary outcome; variables not meeting statistical significance were included a priori for improving face validity. Where there existed multi-collinearity—defined as two variables showing significance on univariate analysis and a variable inflation factor above 2.5—only one variable was chosen for multivariate analysis. For readmission and ED visit outcomes, a time-to-event multi-level Cox proportional hazard regression was performed to model the time to first event while accounting for clustering of patients around hospitals in the model [20]. LOS was modeled by linear regression analysis and SDS by logistic regression analysis. Variables for the multivariable model were based on a priori selection of known confounders. Statistical calculations were performed using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Overall, 1908 patients aged <18 years were included. Table 1 shows the hospital volume by quartile, cohort characteristics and univariate analysis. The lowest volume hospitals (which comprised 30% of index thyroidectomies) performed one or fewer thyroidectomies per year. The highest volume hospitals performed a median 38 thyroidectomies per year (range 19 to 60). Three of five tertiary pediatric hospitals in the province constituted the highest quartile.
The mean age was 10.4 ± 5.4 years (range 0–17), most were female (61.1%), a minority were from rural areas (6.0%) and 7.5% were immigrants. Half of patients underwent primary total thyroidectomy. Cancer was diagnosed in 19.7% and within this group 50% were treated by primary total thyroidectomy and RAI; a further 17% underwent primary total thyroidectomy without RAI; and 25% underwent two-stage thyroidectomy ± RAI. Cancer disproportionately affected those in the older age categories (Supplementary Table 2). Surgery at a high-volume hospital was associated with younger age, urban residence, increased co-morbidity, and total thyroidectomy.
Four (of 14) AHRs accounted for the majority (66.3%) of pediatric thyroidectomies, while one region accounted for 36.4% of thyroidectomies (Supplementary Fig. 1). The remaining regions each accounted for less than 6% of thyroidectomies. Supplementary Table 1 and Supplementary Fig. 1 show the thyroidectomy rate, hospital number and pediatric population within each AHR.
Patients’ administrative health region of residence determined the location of thyroidectomy
Figure 2 (and Supplementary Fig. 1 and Supplementary Table 3) summarize the pattern of thyroidectomy location based on patients’ AHR of residence at the time of surgery. Ninety-two percent of individuals living in an AHR with a high-volume hospital (these were situated in AHRs with higher population levels and the provinces’ major cities) remained in their local AHR for surgery, while 48% of those living in an AHR in quartiles 1–3 underwent surgery locally and 52% migrated out-of-region for surgery. Among AHR in quartiles 1–3, there was, however, variation with respect to referral patterns to high-volume AHR (Supplementary Fig. 1).
Pattern of referrals for thyroidectomy based on provincial administrative health region (AHR) of residence. Percentages in ovals reflect the proportion of patients living in an AHR (above) categorized by hospital volume that underwent thyroidectomy in a AHR (below) categorized by hospital volume. For instance, 2–6% of individuals living in an AHR with a high-volume hospital underwent surgery in an AHR with exclusively low volume hospitals. A patient was more likely to have a thyroidectomy in a high-volume hospital if they resided in an AHR with a high-volume hospital. The lower boxes provide broad context (based on our results) to these patterns. Ranges are provided to protect confidentiality, where small numbers would potentially lead to identifiability
Higher hospital volume is associated with increased LOS, while discrete patient characteristics were associated with post-discharge emergency department visits
Mean LOS rose from 1.35 ± 1.72 days to 1.95 ± 2.27 days between the lowest and highest volume quartiles (p = 0.01; Table 2). Multivariate analysis (Table 3) also demonstrated that LOS increased by 0.6 days in the highest, compared with the lowest quartile (95% CI 0.20, 1.08; p < 0.01). Total thyroidectomy (versus hemi-thyroidectomy) was independently associated with an increased LOS by 0.5 days (95% CI 0.20, 0.79; p < 0.01); cancer diagnosis increased LOS by 0.6 days (95% CI 0.45, 1.03; p < 0.01); and higher co-morbidity score increased LOS by 0.8 days (95% CI 0.38, 1.28; p < 0.01). Younger age (0–8 years) was independently associated with shorter LOS by 0.5 days (95% CI − 0.81, − 0.09; p = 0.01).
Overall, 17% of thyroidectomies province-wide were performed as SDS. SDS was 83% less likely in the highest quartile compared with the lowest quartile hospital volume (OR 0.17; 95% CI 0.07, 0.42; p < 0.01). Total thyroidectomy, cancer diagnosis, and older age (13–17 years) were less likely to be associated with SDS (Tables 2 and 3).
ED visits within 30 days of discharge occurred in 8.2% of patients (136/1658). There was a 4% absolute decrease in ED visits in the highest quartile compared to the lowest (p = 0.02; Table 2), although this did not remain significant in multivariate analysis (Table 3). Discrete patient characteristics were independently associated with the rate of ED visits: male sex increased the rate by 1.68 (95% CI 1.16, 2.43; p < 0.01); the highest material deprivation quintile by 1.89 (95% CI 1.10, 2.37; p = 0.02) compared to the lowest quintile; and rurality by 2.48 (95% CI 1.38, 4.46; p < 0.01).
The overall 30-day readmission rate was 1.9% (37/1908), which was not different across quartiles (Tables 2 and 3). The highest co-morbidity group was associated with a 4.65-fold increased rate of readmission when compared to the lowest co-morbidity group (95% CI 1.31, 16.54; p = 0.02; Table 3).
Discussion
We present the healthcare utilization outcomes after pediatric thyroidectomy over 24 years across a large population, using health administrative data with high capture rate, and describe their association with hospital surgical case volume. To our knowledge, only two other studies have related outcomes to hospital surgical thyroidectomy volume in children. Herein, we show a comparable rate of cancer to these studies [1, 15].
Defining a hospital’s surgical volume
Definitions of hospital surgical volume are inconsistent among existing studies. We defined hospital volume as the annual rate of pediatric thyroidectomy in the year preceding a thyroidectomy. Prior pediatric studies describing thyroidectomy outcomes defined “high hospital volume” variably as: the top 10% of hospital pediatric thyroidectomy volumes (>51/year) [1]; the top 10% of overall thyroid cancer admissions—adult and pediatric (>199/year) [8]; the top patient-level tertile (≥ 22/year) [9]; or a value statistically modelled by hospital volume and the probability of readmission (>39/year) [15]. The surgical volume of our highest quartile (mean 38, range 19–60) is comparable to these previous pre-defined cut-offs despite their adopting different methodologies. In this series, by methodological design, 25% of thyroidectomies were performed at the highest-volume hospitals, whereas this differs between 9 and 42% in other pediatric cohorts [1, 8, 15]. In contrast, 30% of thyroidectomies were performed at the lowest-volume hospitals, whereas this differs between 21 and 86% in other pediatric cohorts [1, 8, 15]. The most comparable cohort, of 644 admissions for pediatric thyroid cancer, found 21% of admissions to low-volume hospitals—defined as 1–10 admissions/year [8]. Our findings reinforce other studies that show a large proportion of pediatric thyroid surgeries performed at low surgical volume hospitals.
Referral patterns and healthcare utilization
High-volume hospitals were more likely to treat younger and more medically complex children, which is consistent with findings from other pediatric and adult cohorts [5, 6, 12, 15]. Low-volume hospitals were not associated with compromised healthcare utilization outcomes as captured in this dataset. These findings may therefore reflect referral pathways appropriate for the necessary level of care. We propose that the current emphasis on universal referral to high-volume centers might take into consideration additional variables (patient age, diagnosis, case complexity, burden of travel) to optimize both patient care and healthcare resource stewardship. For example, in the right circumstances, older, lower-risk adolescent patients may avoid significant disruption and costly travel to distant high-volume centres where resources can be directed to younger, higher risk patients who would benefit most from such expertise.
We found a longer LOS in the highest hospital volume quartile, which remained statistically significant after adjusting for age and co-morbidity burden and which was consistent with the lower likelihood of SDS in the highest quartile. The absolute difference in LOS of 0.6 days, however, is unlikely to be clinically meaningful. Despite higher surgeon volume consistently associated with shorter LOS [1,2,3, 5,6,7,8], hospital volume has not been independently associated with LOS in prior studies [1, 9, 15].
Hospital volume did not independently predict ED visits and this variable has not been previously analyzed against hospital volume. We did find, however, an increased rate of ED visits associated with male sex, increased material deprivation, and increased rurality. These same variables are associated with worse thyroid cancer-specific survival in adolescents and young adults [21]. Increased scrutiny is thus warranted to identify those factors that underlie the higher rates of ED visits in these groups and to address any obstacles to care. We also found an increased readmission rate in patients with higher co-morbidity group; however, these data cannot distinguish whether surgical care or inherent medical complexity explain this association.
Strengths and limitations
This is the first study to relate hospital surgical volume to outcomes in children, outside of a United States population [1, 15]. The strengths of this study derive from access to all of Ontario residents’ administrative and healthcare data, linked through ICES, because of Ontario’s single-payor system; this created a statistically powerful dataset and, through complete population coverage, strengthens the generalizability of our results. By capturing the entire provincial population’s procedure and outcome data we were able to minimize selection biases that may influence studies utilizing other data sets such as single-hospital, health maintenance organizations, managed care consortia or voluntary-reporting registries. Hospital level data are mandated by the Canadian Institute for Health Information (CIHI), separate from billing data, and are thus an accurate measure of surgical volume. We accounted for changes in hospital volume over time by defining volume per thyroidectomy on the previous years’ surgical data. Limitations of this study are inherent to the nature of this data set, which reflects a retrospective analysis of population-level administrative health data rather than prospective patient-level data. While the former offers many strengths with respect to cohort size and breadth of collected data, certain details are unavailable, such as the indication for thyroidectomy (other than cancer) and some specific surgical details (for example, extent of neck dissection). Surgeon sub-speciality was unrecorded in 50% of cases, as a subset of hospitals utilize a funding paradigm that does not consistently capture this variable. Thus, we could not assess clinical or healthcare resource outcomes in relation to surgical specialty. Similarly, individual surgeon volume was not captured; many pediatric surgeons are not reimbursed using a fee-for-service model and thus do not routinely bill per procedure, which limits applying this variable in our dataset. Nonetheless, the relationship between surgeon volume and pediatric thyroidectomy outcomes has previously been well-established and we sought to answer a different question, with broader policy implications. Clinical decision-making is not captured by administrative data therefore the reason for ED visits, readmission, and referral out of region are unknown.
Conclusion
We present a large, population-level cohort of thyroidectomies performed province-wide, with data derived from administrative records in a single-payor universal healthcare system. We demonstrate that increased hospital pediatric surgical volume was associated with an increased length of stay and lower likelihood of SDS, which we speculate is a reflection of increased case complexity at these centres. The highest volume centers operated on the youngest and more medically complex patients. For younger patients and those with medical complexity (such as metastatic carcinoma or Graves’ disease), facilitating access to appropriate surgical expertise should be a priority. In this series, low-volume hospitals were not associated with poorer healthcare utilization outcomes but may have selected for lower-risk cases.
Male sex, rural residence and material deprivation were associated with more frequent ED visits and might endorse a focus on the allocation of healthcare resources and discharge planning to support these patient populations. Pediatric specialist centers are often great distances from families’ homes, which could result in additional economic burden and logistical challenges accessing specialist post-operative assessment—these are important realities to recognize even within a universal healthcare system and may be a disadvantage of stringent, regionalization initiatives.
These findings will help inform the future provision of care for children requiring thyroidectomy—and may impact approaches to care more broadly—in a region with an extremely varied sociodemographic and geographical landscape.
References
Sosa JA, Tuggle CT, Wang TS et al (2008) Clinical and economic outcomes of thyroid and parathyroid surgery in children. J Clin Endocrinol Metab 93(8):3058–3065
Adam MA, Thomas S, Youngwirth L et al (2017) Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg 265(2):402–407
Hauch A, Al-Qurayshi Z, Randolph G et al (2014) Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 21(12):3844–3852
Krishnamurthy VD, Jin J, Siperstein A et al (2016) Mapping endocrine surgery: workforce analysis from the last six decades. Surgery 159(1):102–112
Sosa JA, Bowman H, Tielsch J, Powe NR et al (1998) The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg 228(3):320–330
Stavrakis AI, Ituarte PHG, Ko CY et al (2007) Surgeon volume as a predictor of outcomes in inpatient and outpatient endocrine surgery. Surgery 142(6):887–899
Al-Qurayshi Z, Randolph GW, Srivastav S (2015) Outcomes in endocrine cancer surgery are affected by racial, economic, and healthcare system demographics. Laryngoscope 126(3):775–781
Al-Qurayshi Z, Hauch A, Srivastav S et al (2016) A national perspective of the risk, presentation, and outcomes of pediatric thyroid cancer. JAMA Otolaryngol Head Neck Surg 142(5):472–477
Drews JD, Cooper JN, Onwuka EA (2019) The relationships of surgeon volume and specialty with outcomes following pediatric thyroidectomy. J Pediatr Surg 54(6):1226–1232
Meltzer C, Hull M, Sundang A et al (2019) Association between annual surgeon total thyroidectomy volume and transient and permanent complications. JAMA Otolaryngol Head Neck Surg 145(9):830–838
Breuer C, Tuggle C, Solomon D et al (2013) Pediatric thyroid disease: when is surgery necessary, and who should be operating on our children? J Clin Res Pediatr Endocrinol 5(Suppl 1):79–85
Francis GL, Waguespack SG, Bauer AJ et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7):716–759
Birkmeyer JD, Siewers AE, Finlayson EV et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137
McAteer JP, LaRiviere CA, Drugas GT et al (2013) Influence of surgeon experience, hospital volume, and specialty designation on outcomes in pediatric surgery. JAMA Pediatr 167(5):468–468
Youngwirth LM, Adam MA, Thomas SM et al (2018) Pediatric thyroid cancer patients referred to high-volume facilities have improved short-term outcomes. Surgery 163(2):361–366
Weiner JP, Abrams C (2011) The Johns Hopkins ACG® system technical reference guide version 10.0. John Hopkins Bloomberg School of Public Health
Arim RG, Guevremont A, Kohen DE et al (2017) Exploring the Johns Hopkins aggregated diagnosis groups in administrative data as a measure of child health. Int J Child Health Hum Dev 10(1):19–29
Maltenfort MG, Chen Y, Forrest CB (2019) Prediction of 30-day pediatric unplanned hospitalizations using the Johns Hopkins Adjusted Clinical Groups risk adjustment system. Kamolz L-P, ed. PLoS ONE 14(8):e0221233
Matheson FI, Van Ingen T (2018) 2016 Ontario marginalization index: user guide. St. Michael’s Hospital. Joint Publication with Public Health Ontario, Toronto, ON
Austin PC (2017) A tutorial on multilevel survival analysis: methods. Models Appl Int Stat Rev 85(2):185–203
Keegan THM, Grogan RH, Parsons HM et al (2015) Sociodemographic disparities in differentiated thyroid cancer survival among adolescents and young adults in California. Thyroid 25(6):635–648
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by: Canadian Institute for Health Information (CIHI); Immigration, Refugee and Citizenship Canada Permanent Resident Database (IRCC), Ontario Health (OH), Ontario Registrar General (ORG). The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Parts or whole of this material are based on data and/or information compiled and provided by IRCC current to May 2017. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of IRCC. Parts of this material are based on data and information provided by OH. The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of OH. No endorsement by OH is intended or should be inferred. Parts of this report are based on ORG information on deaths, the original source of which is ServiceOntario. The views expressed therein are those of the author and do not necessarily reflect those of ORG or the Ministry of Government and Consumer Services. We thank the Toronto Community Health Profiles Partnership for providing access to the Ontario Marginalization Index.
Funding
Dr. AD Chesover was funded by the Canadian Paediatric Endocrine Group. This work was supported by the Pitbaldo Basic/Translational Discovery Grant from the Garron Family Cancer Centre, The Hospital for Sick Children, Toronto (JDW, NEW). This work was also supported through a Harry Barberian Research Grant from the University of Toronto Department of Otolaryngology—Head and Neck Surgery (NEW).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. A Eskander has received research funds from Merck (2019) and has been a paid consultant for Bristol-Myers (2019) both of which were for work not related to this study. Dr. JD Wasserman was a paid consultant for Bayer (2019) for work unrelated to the study. The remaining authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chesover, A.D., Eskander, A., Griffiths, R. et al. The Impact of Hospital Surgical Volume on Healthcare Utilization Outcomes After Pediatric Thyroidectomy. World J Surg 46, 1082–1092 (2022). https://doi.org/10.1007/s00268-022-06456-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06456-6